Abstract
Background: Although research has examined patients’ perception of quality of life while in opioid maintenance treatment, the focus has mainly been on health-related quality of life. Objectives: This study aimed to investigate opioid maintenance treatment patients’ subjective overall quality of life and the potential association between quality of life and factors, such as housing, the relationship with their partner, children and friends, leisure, work, financial situation and health during the first year in treatment. Methods: Self-recruited first-time enrolled patients met for a structured registration through face-to face interviews every third month for 12 months. Sociodemographic factors and nine indicators of quality of life from the National Quality Register for Substance Abuse Treatment were utilized. Results: Participants (N = 38), reported a significant improvement in overall quality of life in the first year F (1, 40.4880) = 7.532, p = .009, with a positive effect on .19 per time unit. In particular, the domain financial situation predicted improved quality of life, F (1, 37.774) = 14.212, p = .001. Moreover, there was no significant change for subjective factors such as leisure, relationship with children, housing, health, and relationship with a partner across time. Specific domains of quality of life such as housing, leisure and financial situation were positively associated with overall quality of life. Conclusions: These results suggest that to address factors as a part of patients’ treatment can be instrumental in improving quality of life. Further research is needed to explore these findings in a larger opioid maintenance treatment population.
PUBLIC INTEREST STATEMENT
There is a positive change in quality of life for people addicted to opioids when they enroll in opioid maintenance. This change relates mainly to improvements in health, such as fewer infections and drug related diseases. But, what are patient’s own views on their quality of life? What association is there between the overall quality of life and their housing situation, the relationship with their children and friends, leisure and financial situation in the first year in treatment? Based on answers from face-to face interviews every third month, the article answers these questions. It was found that the overall quality of life improved during the first year, and the financial situation, in particular, predicted improved quality of life. Housing, leisure and financial situation were positively associated with overall quality of life. Exploration of these issues in treatment can help patients improve their quality of life.
Individuals with substance use disorders (SUD) experience harmful impacts and long-term impairments in their lives such as mental and physical problems, issues related to social relationships, housing and personal economy (McLellan, Lewis, O’Brien, & Kleber, Citation2000; Muller, Skurtveit, & Clausen, Citation2017; Shion, Sambamoorthy, Ying, & Aznal, Citation2014; Tiffany, Friedman, Greenfield, Hasin, & Jackson, Citation2012). SUD treatment emphasizes reduction in drug use, deemed successful when patients test negative for drugs (Mitchell et al., Citation2015; Strada et al., Citation2017; Tiffany et al., Citation2012). However, with a comprehensive perspective on SUD, abstinence is no longer the only goal (Bolek, Yargic, & Ekinci, Citation2016; De Maeyer, Vanderplasschen, & Broekaert, Citation2010; Mitchell et al., Citation2015). Although the increasing emphasis on patients’ empowerment and the interest in patients’ viewpoint may present important insights into treatment and life in general, few studies utilize substance (ab)users’ perspectives as an important source of information (De Maeyer, van Nieuwenhuizen, Bongers, Broekaert, & Vanderplasschen, Citation2013; Strada et al., Citation2017). Thus, the concept of quality of life (QOL) is becoming increasingly important in the field of addiction research (Mitchell et al., Citation2015; Rudolf & Watts, Citation2002; Strada et al., Citation2017).
The concept of QOL has been used inconsistently in different research fields (Gill & Feinstein, Citation1994; Laudet, Becker, & White, Citation2009; Zubaran & Foresti, Citation2009). Terms like life satisfaction, subjective well-being and health-related quality of life (HRQOL) are sometimes used synonymously with QOL (Camfield & Skevington, Citation2008; De Maeyer et al., Citation2010). Although there is no consensus on the content of the term QOL, researchers agree that QOL is subjective and multidimensional (De Maeyer et al., Citation2010; Laudet et al., Citation2009; WHO, Citation1995b). A widely used definition of QOL is “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (WHO, Citation1995b, p. 1405).
A widely applied standard in addiction research has been the focus on how a disease affects a person`s functioning. In this context the absence of disease is essential (De Maeyer et al., Citation2010; Moons, Citation2004; Zubaran & Foresti, Citation2009). Today, a more comprehensive approach acknowledges QOL as a reflection of how people perceive and react to different aspects of a person’s life (Gill & Feinstein, Citation1994). Domain satisfaction is a judgement of a specific aspect of an individual’s life, and life satisfaction and domain satisfaction are generally correlated (Pavot & Diener, Citation2008). To better understand patients’ satisfaction with life overall, and to give attention to social aspects, it has been suggested that the best patient reported outcome measure to use is QOL (De Maeyer et al., Citation2010; Muller, Citation2017).
In relation to the SUD population, research has primarily been concerned with socially desirable outcomes such as abstinence, reduced criminality and prostitution and health-related issues. Research on opioid maintenance treatment (OMT) with a focus on QOL has primarily had a health-related perspective (De Maeyer, Vanderplasschen, & Broekaert, Citation2009; De Maeyer et al., Citation2010; Laudet, Citation2011; Muller, Skurtveit, & Clausen, Citation2016b). Research has also focused on the correlation between addiction severity and QOL, has compared groups with and without dual diagnosis, and has analysed the impact of methadone or buprenorphine on patients’ QOL (Zubaran & Foresti, Citation2009). Concerning health-related quality of life (HRQOL), research has documented significant improvements in physical and psychological health components of QOL (Karow et al., Citation2011; Mitchell et al., Citation2015; Nosyk et al., Citation2011; Padaiga, Subata, & Vanagas, Citation2007; Torrens et al., Citation1997; Tran et al., Citation2016). At a 12-month follow-up, improvements were reported in the realm of pain/discomfort and anxiety/depression (Nosyk et al., Citation2011). On the other hand, symptoms of sleep problems, pain and depression influence OMT patients’ quality of life and the ability to function (Peles, Schreiber, & Adelson, Citation2006; Pud, Zlotnick, & Lawental, Citation2012). A recent study demonstrates a significant negative correlation between high methadone dosage (> 90 mg/day) and QOL in several domains, including the physical and psychological domains (Pedrero-Perez, Citation2017).
In comparison to the general population and patients with other chronic diseases, patients in OMT report significantly poorer QOL (Best et al., Citation2013; De Maeyer et al., Citation2010; De Maeyer, Vanderplasschen, Lammertyn et al., Citation2011; Laudet et al., Citation2009; Rudolf & Watts, Citation2002). A study of 549 Norwegian patients, including inpatients and outpatients in both opioid maintenance treatment and medication-free treatment, found that about three-fourths reported their overall QOL to be poor or very poor. Furthermore, the results showed that those who stated methadone/buprenorphine as their preferred substance were more likely to report neutral, good or very good QOL rather than very poor QOL (Muller, Skurtveit, & Clausen, Citation2016a). Research shows that QOL improves after starting OMT, especially during the first months of treatment (De Maeyer, Vanderplasschen, Lammertyn et al., Citation2011; Feelemyer, Jarlais, Arasteh, Phillips, & Hagan, Citation2014). The positive effect of QOL is often explained by improvements in health (Nosyk et al., Citation2011).
Social support is an important predictor of success in OMT (Chou et al., Citation2013; Khuong, Vu, Huynh, & Thai, Citation2018; Laudet, Morgen, & White, Citation2006; Lin, Wu, & Detels, Citation2011). Ponizovsky et al. (Citation2010) found that the best predictor of QOL was social support from friends and significant others. A study of 159 patients enrolled in methadone treatment for about a decade identified social relationships and support, psychological well-being, employment, independence and a meaningful life as important components of a good QOL (De Maeyer, Vanderplasschen, Camfield et al., Citation2011). Other factors linked to improved QOL are a life less controlled by the addiction, fewer social issues and a better relationship with family and friends. Health was rarely mentioned in this context (Brekke, Vetlesen, Høiby, & Skeie, Citation2010). Muller (Citation2017) found that 12 month after initiation of treatment changes in general QOL were related to development in patients’ social network. Those who expanded or maintained an abstinent network reported a greater increase in QOL. Merely patients who remained in OMT one year after enrolment reported improved social quality of life.
One of the goals of OMT is to improve the QOL of opioid-dependent individuals (Norwegian Directorate of Health, Citation2010). The way in which opioid-dependent individuals experience their daily life is not well researched (De Maeyer et al., Citation2009; Pasareanu, Opsal, Vederhus, Kristensen, & Clausen, Citation2015). It is important to utilize user-driven approaches to gain insights into aspects that determine OMT individuals’ self-perceived QOL (De Maeyer, Vanderplasschen, Camfield et al., Citation2011). Instruments for measuring QOL in opioid-dependent patients tend to focus on health-related aspects (Strada et al., Citation2017). Health is important for OMT patients’ QOL. However, the broader impact of opioid dependence calls for instruments that also incorporate how social and material living conditions add to the understanding of QOL. Patients’ social and material living conditions have an impact on their overall QOL. On this background, our study addresses the following aims:
to examine patients’ overall QOL during the first year after enrolment in OMT, and
to investigate potential correlations with overall QOL to domain-specific QOL indicators in housing, relationship with children and friends, work, leisure, health and financial situation.
1. Material and methods
1.1. Sample
Participants for this study were recruited from eight OMT outpatient units in the catchment area of Haukeland University Hospital, Bergen, Norway. The geographic catchment area includes approximately 350 000 inhabitants from Bergen municipality and surrounding municipalities. There are about 1000 OMT patients in the catchment area of Haukeland University Hospital, including patients who have been in OMT from 1998 to newly enrolled patients.
The National Quality Register for Substance Abuse Treatment (NQR-SAT) applies to individuals with substance use disorders enrolled in treatment. NQR-SAT originates from western Norway and is awaiting approval as a national registry. The initially established registry was used in the present study.
Data used in this paper were collected from 47 self-recruited patients in OMT. They were recruited during two periods: January to December 2013, and September 2015 to June 2016. Inclusion criteria were opioid dependence according to ICD-10 or DSM-IV, age > 18 years, first time admittances to OMT, living in Haukeland University Hospitals’ catchment area, and commencement of OMT medication (Buprenorphine or Methadone) before the first registration. Lack of competence to consent was the only exclusion criterion.
Patients received either buprenorphine or methadone as medical treatment with a variation in dosage from 4 mg to 20 mg buprenorphine and 80 to 100 mg methadone. Two participants received extended-release injections with naltrexone which blocks the effects of opioids. The majority of patients came to their local outpatient unit for daily medication and a short conversation with the employee at the outpatient unit, while those in prison received medicine on a daily basis from health employees in prison or prison staff. The two patients who received naltrexone got a muscle injection once a month.
During the first year, five participants dropped out, three withdrew from the study due to lack of interest, and one was excluded due to cognitive impairment and inability to provide consent. Data from these participants were included in the analysis up to the time they completed the research participation. The total sample included 47 opioid-dependent individuals’, 11 females and 36 males. For sociodemographic characteristics see (Carlsen & Torsheim, Citation2019).
1.2. Data collection
Participants met for structured registrations through face-to-face interviews every third month for a period of two years. The current study utilizes data from baseline (T0) and every third month through the first 12-month follow-up from T1 to T4. In total, 291 observations of a total of 47 individuals were analysed and distributed as follows: 47 participants at T0, 38 participants at T1 and T2, 34 participants at T3 and 36 at T4. Of the 47 included participants, 29 participants completed all registrations, eight completed four, one completed three, four completed two, and five participants completed only baseline registrations.
The principal investigator was responsible for data management. Participants provided written informed consent to participate in the study, and the study was approved by the Regional Committee for Medical and Health Research Ethics (2013/429/REK South-East C).
1.3. Measures
NQR-SAT collects Patient Reported Outcome Measures (PROM- data) and Patient Reported Experience Measure (PREM-data). PROMs capture a patient’s perception of their health (self-reported health status, symptoms, QOL, etc.) (Black, Citation2013; Neale et al., Citation2016; SKDE, Citation2017), whereas PREMs capture a patient’s perception of their experience with health care or treatment (involvement, communication, service access, etc. (SKDE, Citation2017). In other words, data in NQR-SAT are patients’ subjective perceptions on given topics.
Questions from validated tools are incorporated in NQR-SAT, and nine indicators of QOL were utilized in this study. One indicator measured the overall QOL, and eight indicators measured QOL in specific social domains. To measure the overall QOL, we used the question “How would you rate your quality of life as a whole?”, which is used in several instruments on QOL, including WHOQOL-Brief and WHOQOL (WHO, Citation1995a, Citation1996) and Personal Wellbeing Index (Cummins, Eckersley, Pallant, van Vugt, & Misajon, Citation2003). The eight specific indicators reflect on various social life domains, where some of them are strongly related to global life satisfaction (Tomyn, Tyszkiewicz, & Cummins, Citation2011). The specific domain questions were: “How satisfied are you with: 1) your personal relationship with partner, 2) your relationship with children, 3) your relationship with friends (International Wellbeing Group, Citation2013; Tomyn et al., Citation2011; WHO, Citation1996) 4) housing (WHO, Citation1995a, Citation1996) 5) your health (International Wellbeing Group, Citation2013; WHO, Citation1996) 6) work (WHO, Citation1995a) 7) leisure (WHO, Citation1995a), and 8) financial situation (WHO, Citation1995a). Equally to the WHO-BRIEF (WHO, Citation1996) the participants reported, their QOL on a five-point Likert-type response scale, ranging from 1 = “very dissatisfied” to 5 = “very satisfied” at each measurement point.
To measure participants drug use the NQR-SAT uses the question “How many days have you used alcohol or drugs during the last 30 days?” which is the same question as in EuropASI (Blacken et al., Citation1994).
1.4. Data analysis
Descriptive statistics with frequency analysis were used to examine the participants’ demographic characteristics at baseline.
Linear mixed models for repeated measures were used to estimate level and change in general and specific domains of QOL from baseline to 12-month follow up. Main and interactive effects were tested with Satterthwaite’s corrected F-test. A significance level of p < 0.05 was considered statistically significant in all the analyses. SPSS version 24 was used for the analysis.
The linear mixed analysis was conducted in two stages. The objective of the first stage was to establish a proper model of change, regressing the dependent variable on time and relevant group factors. In the random part of the model, we compared a random intercept only model with a random intercept and random slope of time model. In the random intercept model, individuals differed with respect to their intercept at time 0, but shared the effect of time. In the random intercept and slope model, individuals differed in their intercept on time and in their slope of change. Model fits were compared using likelihood ratio tests for nested models.
In the second stage of analysis, time invariant baseline factors were included to test differences in intercept and change. Significance was assessed by omnibus F-tests per factor term. In addition, we tested whether the effect of time interacted with baseline characteristics such as level of education (no education/primary/secondary school/high school/higher education), marital status (single/married), and type of living situation (own apartment/permanently with parents/temporary housing/homeless). Time is coded as four time points, one for every three months data were collected.
2. Results
2.1. Attrition
There was attrition from baseline to follow-up. In the first year, eight participants missed one data point, one participant missed two data points, four participants missed three data points, and five participants missed four data points and had only baseline registration. Twenty-nine participants had no missing values.
An independent sample t-test showed no significant differences for the first year between non-completers and completers for level of education, marital status, and type of living situation. There were no statistically significant differences at baseline between completers and non-completers with respect to quality of life in the domains of relationship with a partner, children and friends, housing, health, work, leisure, and financial situation.
2.2. Demographic characteristics at T0
At baseline, the mean age of the 47 participants was 37.8 years, 76.6 % were men, and 93.6 % were of Norwegian ethnicity. Among women who participated at baseline 73 % participated in the follow-ups, while the average was 79 % among men. Approximately 50 % (n = 24) lived in their own apartment, while 29.8 % (n = 14) had temporary housing such as rehabilitation homes, treatment institutions or prison facilities. Seventy-six point six percent (n = 36) were single. Primary/secondary school were reported as the participants’ highest level of education during the entire 12-month follow-up. Fifty-eight percent (n = 22) had a meaningful activity at baseline, yet none of the participants had work. Twenty-five participants had children, and 80 % (n = 20) of them had visitation rights or custody of their own children under the age of 18 years, while 16 % (n = 4) had no custody/visitation rights, and 28 % (n = 7) had adult children. At baseline, 63.8 % (n = 30) had no unresolved issues with the police or justice system.
2.3. Change in QOL
Table shows that the results form a series of linear mixed models regressing QOL on time. The overall QOL increased significantly during the 12 months in OMT, F (1, 40.880) = 7.532, p = .009. The positive effect of the overall QOL was b = .19 per time unit, corresponding to a moderate effect size of 0.62 SD change during the 12 months. The random intercept and slope components were statistically significant, indicating that patients differed in their level at baseline, as well as in their rate of change. To exemplify, according to the effect of time, patients with a change rate at 2 SD below the mean change rate would have a decline in QOL, whereas patients with a change rate at 2 SD above the mean would increase their overall QOL across time.
Table 1. Estimates of Covariance Parameters and Fixed Effects Estimates for social measures of QOL
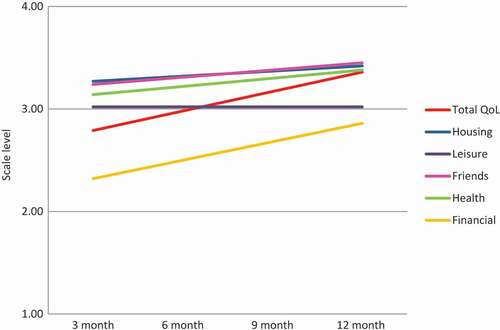
The rate of change for the first 12 months was positive for all specific QOL domains, except for leisure, see Figure . Statistical significance of change per time unit was only achieved for financial QOL F (1, 37.774) = 14.212, p = .001. At baseline, the average patients were dissatisfied with their financial QOL and the increase per time unit was b = .18. A significant variation between patients was also identified.
Based on few observations for QOL in relation to partner, relationship with children and work, these domains were excluded from this analysis.There was no significant rate of change for friends F (1, 38.542) = 1.488, p = .230, housing F (1, 38.847) = 7.33, p = .385 and health F (1, 37.014) = 3.140, p = .085. Participants did vary on the abovementioned domain-specific QOL and spread across the entire scale. However, this variation was not significant.
In the last sequence of models, overall QOL was regressed on QOL in specific domains, using specific QOL as time-varying covariates, see Table . QOL domains such as financial situation, housing and leisure were associated with higher overall QOL. Leisure was the strongest contributor b = .32, p = .001, followed by housing b = .22, p = .001 and financial situation b = .15, p = .03.
Table 2. Overall QOL regressed on specific QOL social domains
We also tested for interaction effect for level of education, marital status and type of housing. None of these had any significant prediction on overall QOL, F (4, 43.822) = 1.103, p = .367, F (2,104.367) = .413, p = .662, F (3, 94.529) = 1.670, p = .179, respectively.
3. Discussion
Patients are generally dissatisfied with their overall QOL before enrolling into OMT (De Maeyer, Vanderplasschen, Lammertyn et al., Citation2011). Our main finding was that, although OMT patients QOL fluctuated, on average their overall QOL improved after starting OMT, corresponding to a moderate effect size. This result is congruent with previous research. The continuous positive improvement in overall QOL can indicate that the gap between what patients expect and what they receive from OMT is little.
Different aspects can influence patients’ QOL. Giacomuzzi et al. (Citation2003) found a significant increase of QOL score for finances at six months follow-up. In the current study, participant’s satisfaction with their financial situation was a significant predictor for positive overall QOL. Norwegian OMT patients experience an immediate effect of the enrolment; they do not pay for their OMT medication as this is covered by the welfare state. This releases capital that previously was linked to purchase of opioids and other substances (Redden, Tracy, & Shafer, Citation2013). When starting in OMT, patients are given an opportunity to address the economic challenges and utilize official help from the Norwegian Labour and Welfare Administration (NAV). NAV assists patients with several issues, e.g. ensuring that bills are paid, setting up a budget for debt repayment, and applying for social benefits or disability pension. Many OMT patients have little regular work experience and do not have a regular income. By applying for social benefits or disability pension, those who meet the requirements will receive a fixed monthly income from the welfare state. By achieving control over their financial situation, patients can achieve a security that they have not previously experienced, which can result in economic freedom: they might have the opportunity to save money and/or buy things they earlier could not afford (Redden et al., Citation2013).
About 68.6 % of the patients with five to ten years in outpatient methadone treatment reported low QOL scores for financial situation (De Maeyer, Vanderplasschen, Lammertyn et al., Citation2011). In our study, we also found that the average level of satisfaction with financial QOL was low at baseline, yet it increased during the first 12 months. Some patients are heavily in debt and live in an economic chaos, spending all their money and not being able to pay rent for housing or other bills (Carlsen, Gaulen, Alpers, & Fjaereide, Citation2018; Gaulen, Alpers, Carlsen, & Nesvåg, Citation2017). Losing contact and status in the drug environment can lead to a worse economic situation, e.g. possible loss of income from illegal activity and less access to income. Many patients emphasized the importance of having basic comforts such as affordable housing, money for personal transportation, food and an income (De Maeyer et al., Citation2009) nevertheless, living on disability benefits, for many, means that they must live on an existence minimum.
By achieving financial security, housing, family, and basic comforts, OMT patients achieve a stability in life and thereby a meaningful life (De Maeyer, Vanderplasschen, Camfield et al., Citation2011). To improve QOL it is important to support OMT patients in their daily life with practical, social and environmental support (De Maeyer, Vanderplasschen, Camfield et al., Citation2011). In this context, leisure time is important. Engagement in meaningful activity has been associated with better QOL (Best et al., Citation2012), and our findings show an association between high QOL leisure and high overall QOL. Having something to do, an activity or interest, gives life meaning and purpose and may reduce the loneliness many OMT patients’ experience and remove it as a prominently negative factor.
Social network and relationship to family and friends have been highlighted as important predictors for QOL (De Maeyer et al., Citation2009; De Maeyer, Vanderplasschen, Camfield et al., Citation2011; Muller et al., Citation2017). Sun et al. (Citation2015) found that family relations among patients, and the quality of such relations, improved after starting OMT. Others have demonstrated that gaining an abstinent social network improved the global QOL (Best et al., Citation2012; Muller et al., Citation2017). In our study, no domains such as friends, partner or children were significant predictors for overall QOL. A possible explanation for the discrepancy between previous research and our study may be that participants experience loss of network and a social arena. Starting in OMT may be a new beginning for many patients, a possibility to break with drug-using friends and the drug users’ network. Sun et al. (Citation2015) found that OMT patients reduced daily contact with drug-using friends after starting in OMT. However, establishing a new drug-free network, or reconnecting with family members or old friends, may take longer or occur later than during the first 12 months (Karow et al., Citation2011). Other explanations can be that participants in our study were satisfied or dissatisfied with their friends both before and after enrolling in OMT; the friends were still the same, and enrollment in OMT did not change the friendship. Or, participants experienced themselves unable to establish a drug-free network, or they wanted to wait to reconnect with drug-free friends until they were back on their feet. Participants also reported that they had few or no friends in the drug environment, but many acquaintances. Lack of social network support, few friends and little or no contact with family members are also factors demonstrated to be common in older patients in OMT (Carlsen et al., Citation2018).
There is a significant time effect in the domains of general well-being (Winklbaur, Jagsch, Ebner, Thau, & Fischer, Citation2008). Research has documented an increase in satisfaction with life for patients during the first months in OMT (Maremmani, Pani, Pacini, & Perugi, Citation2007; Xiao, Wu, Luo, & Wei, Citation2010), or during the first half-year (Karow et al., Citation2011; Padaiga et al., Citation2007). Our study is in line with previous research regarding the effect of time on overall QOL. Moreover, we found the effect to be present even twelve months after participants were enrolled in OMT. Muller et al. (Citation2017) showed that for those still in OMT, social QOL increased during 12-month follow-up, and the increase was a function of treatment retention, not a function of time.
The present study did not incorporate the perspective of health on QOL. There is vast evidence about the relationship between QOL and health (Fei, Yee, Habil, & Danaee, Citation2016; Karow et al., Citation2010; Mitchell et al., Citation2015), and more research on the association between social and material living conditions and QOL is needed. Besides, our study showed that health was not significant, even though it was close to the significance level of .05. This finding is not in line with the literature which states that health improves upon OMT entry. There may be several reasons why health was not significant. One explanation may be that the Norwegian welfare system ensures everyone equal treatment in the health care system regardless of the status as OMT patient or not. Another possibility is that participants have underreported both physical and mental ailments. Some participants did not agree with diagnoses given them earlier in life, and chose therefore not to report these. Others did not enter treatment in a very poor health condition, nor did they consider health as an important factor for their QOL whereas other variables were weighted more heavily. According to De Maeyer et al. (Citation2009) substance (ab)users primarily associate social inclusion and self-determination with QOL, and not health.
4. Strengths and limitations
When interpreting the results, some limitations must be taken into account. This study consists of self-selected participants, and the sample may therefore not be representative of OMT patients in general. However, substance abusers’ self-reports are regarded as generally accurate (Kopak, Proctor, & Hoffmann, Citation2017; Reinert & Allen, Citation2007; Robinson, Sobell, Sobell, & Leo, Citation2014).
There are several potential explanations for the small sample size in this study. One explanation is that life was too chaotic and not compatible with participation in this research project. OMT patients rather needed time to arrange for a place to stay, to settle the economy, attend meetings with their doctor, social services and other official helping services. This was “a full time job” and they did not have the surplus at that time that was needed to participate in this research project. Another explanation is the way patients were recruited. The first year, participants were mainly recruited by the means of OMT advisors working at the OMT units who informed newly enrolled patients about the study. Besides, an information leaflet and an invitation to participate were sent to all first time enrolled patients. This proved to be ineffective. Hence, more proactive strategy was chosen in the second recruitment stage, with a better outcome.
Participants assessment of QOL may be influenced by their current mood (Pavot & Diener, Citation2008), but the effects produced in a study are small compared to the stable variance in the measure settings. Occasion-specific mood effects were not inherently important in ecological measurement (Eid & Diener, Citation2004).
To grasp the full scope of change in OMT patients’ QOL, a follow-up period of 12 months may be too short. According to clinical experience patients are going through many changes in life during the first 12 months in treatment, such as getting a structured meaningful everyday life, regain control over mental, social, economic and environmental issues that emerges after years of substance abuse. QOL changes over time, and in a 12 month period we might just capture temporary changes in QOL. With patients staying in OMT for years or even forever, research needs to focus on QOL in long-term conditions. Thereby we might identify important predictors of lasting improved QOL.
The uniqueness of our study is the frequency of the follow-up, every third month. A time interval of three months enables participants to recall important events that affect them, in contrast to studies with annual or longer recall periods, because recall deteriorates with time (Fadnes, Taube, & Tylleskar, Citation2009).
5. Implications of the study
The main objective of this study was to take a social perspective on factors that affect the quality of life of OMT patients. Although the QOL perspective provides a more comprehensive understanding of patients’ experiences with OMT, QOL used to be neglected in SUD studies. An important implication of this study is that social aspects can improve QOL in OMT patients. These aspects need to be addressed in clinical practice in a larger OMT population. By integrating QOL in clinical practices, additional information, aside from the diagnostic information, can be provided for a total picture of the patient, and the concept of QOL can go beyond the boundaries of the research field (De Maeyer et al., Citation2010). It appears that the treatment system would benefit if more attention were given to QOL factors rather than merely health issues. Improved QOL of OMT patients may have positive effects on other issues in life.
6. Conclusion
Participants QOL vary, in terms of both overall QOL and domain-specific QOL, at enrolment in OMT and throughout the 12-month follow-up period. Nevertheless, patients in this study experienced a small increase of overall QOL, and a specific significant improvement was found for financial QOL during the first 12 months in treatment. Level of education, marital status and type of housing did not predict overall quality of life, however, higher quality of life for leisure; housing and financial situation was associated with higher overall QOL. It is essential to enhance aspects of life that matter to patients in OMT, as this has important implication for better treatment outcomes. The clinical practice currently lacks this focus, which can and should be elaborated to a greater extent than today.
Acknowledgements
We thank the participants for their contribution and sharing their histories and experiences.
Additional information
Funding
Notes on contributors
Siv-Elin Leirvaag Carlsen
Siv-Elin Leirvaag Carlsen is a researcher at the Department of Addiction at Haukeland University Hospital in Bergen, and a PhD-student at the Department of Psychosocial Science at Faculty of Psychology at University in Bergen, Norway. Her topic for the PhD is changes experienced by first time enrolled patients in opioid maintenance treatment, with a specific focus on their quality of life.
Linn-Heidi Lunde
Linn-Heidi Lunde is clinical psychologist and researcher at Department of Addiction Medicine, Haukeland University Hospital and associate professor at Department of Clinical Psychology, University of Bergen.
Torbjørn Torsheim
Torbjørn Toseheim is a Professor of psychometrics at the Department of Psychosocial Science, University of Bergen.
References
- Best, D., Gow, J., Knox, T., Taylor, A., Groshkova, T., & White, W. (2012). Mapping the recovery stories of drinkers and drug users in glasgow: Quality of life and its associations with measures of recovery capital. Drug and Alcohol Review, 31(3), 334–14. doi:10.1111/j.1465-3362.2011.00321.x
- Best, D., Savic, M., Beckwith, M., Honor, S., Karpusheff, J., & Lubman, D. I. (2013). The role of abstinence and activity in the quality of life of drug users engaged in treatment. Journal of Substance Abuse Treatment, 45(3), 273–279. doi:10.1016/j.jsat.2013.02.010
- Black, N. (2013). Patient reported outcome measures could help transform healthcare. BMJ (Clinical Research Ed). doi:10.1136/bmj.f167
- Blacken, P., Hendriks, V., Pozzi, G., Tempesta, E., Hartgers, C., Koeter, M., … Uchtenhagen, A. (1994). European Addiction Severity Index (EuropASI). EMCCDA. Retrieved from http://www.emcdda.europa.eu/html.cfm/index3647EN.thml
- Bolek, S., Yargic, I., & Ekinci, O. (2016). The effects of Buprenorphine/Naloxane maintenance treatment on the quality of life, substance use and functionality in opiate dependence: A follow-up study. Klinik Psikofarmakoloji Bülteni-Bulletin of Clinical Psychopharmacology, 26(2), 141–151. doi:10.5455/bcp.20151101022909
- Brekke, M., Vetlesen, A., Høiby, L., & Skeie, I. (2010). Livskvalitet hos pasienter i legemiddelassistert rehabilitering (Quality of life in patients in opioid maintenance treatment). Tidsskriftet Den Norske legeforening, 13–14(130), 1340–1342. doi:10.4045/tidsskr.09.1117
- Camfield, L., & Skevington, S. (2008). On Subjective Well-Being and Quality of Life. Journal of Health Psychology, 13, 764–775. doi:10.1177/1359105308093860
- Carlsen, S.-E. L., Gaulen, Z., Alpers, S. E., & Fjaereide, M. (2018). Beyond medication: Life situations of older patients in opioid maintenance treatment (Submitted). Addiction Research & Theory. doi:10.1080/16066359.2018.1515351
- Carlsen, S-E. L, & Torsheim, T. (2019). Self-reported adverse experiments and age of opioid onset for first time admitted to opioid maintenance treatment (in press). Heroin addiction & related clinical problems.
- Chou, Y.-C., Shih, S.-F., Tsai, W.-D., Li, C.-S. R., Xu, K., & Lee, T. S.-H. (2013). Improvement of quality of life in methadone treatment patients in northern Taiwan: A follow-up study. BMC Psychiatry, 13(1), 190. doi:10.1186/1471-244x-13-190
- Cummins, R. A., Eckersley, R., Pallant, J., van Vugt, J., & Misajon, R. (2003). Developing a national index of subjective wellbeing: The Australian unity wellbeing index. Social Indicators Research, 64(2), 159–190. doi:10.1023/a:1024704320683
- De Maeyer, J., van Nieuwenhuizen, C., Bongers, I. L., Broekaert, E., & Vanderplasschen, W. (2013). Profiles of quality of life in opiate-dependent individuals after starting methadone treatment: A latent class analysis. International Journal of Drug Policy, 24(4), 342–350. doi:10.1016/j.drugpo.2012.09.005
- De Maeyer, J., Vanderplasschen, W., & Broekaert, E. (2009). Exploratory study on drug users’ perspectives on quality of life: More than health-related quality of life? Social Indicators Research, 90(1), 107–126. doi:10.1007/s11205-008-9315-7
- De Maeyer, J., Vanderplasschen, W., & Broekaert, E. (2010). Quality of life among opiate-dependent individuals: A review of the literature. International Journal of Drug Policy, 21, 364–380. doi:10.1016/j.drugpo.2010.01.010
- De Maeyer, J., Vanderplasschen, W., Camfield, L., Vanheule, S., Sabbe, B., & Broekaert, E. (2011). A good quality of life under the influence of methadone: A qualitative study among opiate-dependent individuals. International Journal of Nursing Studies, 48(10), 1244–1257. doi:10.1016/j.ijnurstu.2011.03.009
- De Maeyer, J., Vanderplasschen, W., Lammertyn, J., Nieuwenhuizen, C., Sabbe, B., & Broekaert, E. (2011). Current quality of life and its determinants among opiate-dependent individuals five years after starting methadone treatment. Quality of Life Research : an International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 20, 139–150. doi:10.1007/s11136-010-9732-3
- Eid, M., & Diener, E. (2004). Global judgments of subjective well-being: Situational variability and long-term stability. Social Indicators Research, 65(3), 245–277. doi:10.1023/B:SOCI.0000003801.89195.bc
- Fadnes, L. T., Taube, A., & Tylleskar, T. (2009). How to identify information bias due to selfreporting in epidemiological research. Internet Journal of Epidemiology, 7(2), 1-10. Retrieved from: https://pdfs.semanticscholar.org/8f8f/83f0888d8058fd37a3e449c62b9938808909.pdfga=2.33702121.952303785.1547541319-1349503116.1521721717
- Feelemyer, J. P., Jarlais, D. C. D., Arasteh, K., Phillips, B. W., & Hagan, H. (2014). Changes in quality of life (WHOQOL-BREF) and addiction severity index (ASI) among participants in opioid substitution treatment (OST) in low and middle income countries: An international systematic review. Drug and Alcohol Dependence, 134, 251–258. doi:10.1016/j.drugalcdep.2013.10.011
- Fei, J. T. B., Yee, A., Habil, M. H. B., & Danaee, M. (2016). Effectiveness of methadone maintenance therapy and improvement in quality of life following a decade of implementation. Journal of Substance Abuse Treatment, 69, 50–56. doi:10.1016/j.jsat.2016.07.006
- Gaulen, Z., Alpers, S. E., Carlsen, S.-E. L., & Nesvåg, S. (2017). Health and social issues among older patients in opioid maintenance treatment in Norway. Nordic Studies on Alcohol and Drugs, 34(1), 80–90. doi:10.1177/1455072516682167
- Giacomuzzi, S. M., Riemer, Y., Ertl, M., Kemmler, G., Rössler, H., Hinterhuber, H., & Kurz, M. (2003). Buprenorphine versus methadone maintenance treatment in an ambulant setting: A health‐related quality of life assessment. Addiction, 98(5), 693–702. doi:10.1046/j.1360-0443.2003.00352.x
- Gill, T. M., & Feinstein, A. R. (1994). A critical appraisal of the quality of quality-of-life measurements. JAMA, 272(8), 619–626.
- International Wellbeing Group. (2013). Personal wellbeing index, 5th ed. Melbourne, Australia. Retrieved from: http://www.acqol.com.au/uploads/pwi-a/pwi-a-english.pdf
- Karow, A., Reimer, J., Schafer, I., Krausz, M., Haasen, C., & Verthein, U. (2010). Quality of life under maintenance treatment with heroin versus methadone in patients with opioid dependence. Drug and Alcohol Dependence, 112(3), 209–215. doi:10.1016/j.drugalcdep.2010.06.009
- Karow, A., Verthein, U., Pukrop, R., Reimer, J., Haasen, C., Krausz, M., & Schaafer, I. (2011). Quality of life profiles and changes in the course of maintenance treatment among 1,015 patients with severe opioid dependence. Substance Use & Misuse, 46(6), 705–715. doi:10.3109/10826084.2010.509854
- Khuong, L. Q., Vu, T.-V. T., Huynh, V.-A. N., & Thai, T. T. (2018). Psychometric properties of the medical outcomes study: Social support survey among methadone maintenance patients in Ho Chi Minh City, Vietnam: A validation study. Substance Abuse Treatment, Prevention, and Policy, 13, 8. doi:10.1186/s13011-018-0147-4
- Kopak, A. M., Proctor, S. L., & Hoffmann, N. G. (2017). The cumulative risk associated with demographic background characteristics among substance use treatment patients. Addiction Research & Theory, 25(3), 216–224. doi:10.1080/16066359.2016.1265109
- Laudet, A. B. (2011). The case for considering quality of life in addiction research and clinical practice. Addiction Science & Clinical Practice, 6(1), 44–55.
- Laudet, A. B., Becker, J. B., & White, W. L. (2009). Don’t wanna go through that madness no more: Quality of life satisfaction as predictor of sustained remission from illicit drug misuse. Substance Use & Misuse, 44, 227–252. doi:10.1080/10826080802714462
- Laudet, A. B., Morgen, K., & White, W. L. (2006). The role of social supports, spirituality, religiousness, life meaning and affiliation with 12-step fellowships in quality of life satisfaction among individuals in recovery from alcohol and drug problems. Alcoholism Treatment Quarterly, 24(1–2), 33–73. doi:10.1300/J020v24n01_04
- Lin, C., Wu, Z., & Detels, R. (2011). Family support, quality of life and concurrent substance use among methadone maintenance therapy clients in China. Public Health, 125(5), 269–274. doi:10.1016/j.puhe.2011.01.009
- Maremmani, I., Pani, P. P., Pacini, M., & Perugi, G. (2007). Substance use and quality of life over 12 months among buprenorphine maintenance-treated and methadone maintenance-treated heroin-addicted patients. Journal of Substance Abuse Treatment, 33, 91–98. doi:10.1016/j.jsat.2006.11.009
- McLellan, A. T., Lewis, D. C., O’Brien, C. P., & Kleber, H. D. (2000). Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA, 284, 1689. doi:10.1001/jama.284.13.1689
- Mitchell, S. G., Gryczynski, J., Schwartz, R. P., Myers, C., O’Grady, K. E., Olsen, Y. K., & Jaffe, J. H. (2015). Changes in quality of life following buprenorphine treatment: Relationship with treatment retention and illicit opioid use. Journal of Psychoactive Drugs, 47(2), 149–157. doi:10.1080/02791072.2015.1014948
- Moons, P. (2004). Why call it health-related quality of life when you mean perceived health status? European Journal of Cardiovascular Nursing : Journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology, 3(4), 275–277. doi:10.1016/j.ejcnurse.2004.09.004
- Muller, A. E. (2017). Quality of life, substance use disorders, and social lives: Exploring one-year outcomes and intrinsic links ( Ph.D.). Institute of Clinical Medicine, Oslo. Retrieved from https://www.duo.uio.no/bitstream/handle/10852/59519/PhD-Muller-DUO.pdf?sequence=5&isAllowed=y
- Muller, A. E., Skurtveit, S., & Clausen, T. (2016a). Many correlates of poor quality of life among substance users entering treatment are not addiction-specific. Health and Quality of Life Outcomes, 14(1), 39. doi:10.1186/s12955-016-0439-1
- Muller, A. E., Skurtveit, S., & Clausen, T. (2016b). Validating the generic quality of life tool “QOL10” in a substance use disorder treatment cohort exposes a unique social construct. BMC Medical Research Methodology, 16. doi:10.1186/s12874-016-0163-x
- Muller, A. E., Skurtveit, S., & Clausen, T. (2017). Building abstinent networks is an important resource in improving quality of life. Drug and Alcohol Dependence, 180, 431–438. doi:10.1016/j.drugalcdep.2017.09.006
- Neale, J., Vitoratou, S., Finch, E., Lennon, P., Mitcheson, L., Panebianco, D., … Marsden, J. (2016). Development and validation of ‘SURE’. A Patient Reported Outcome Measure (PROM) for Recovery from Drug and Alcohol Dependence Drug Alcohol Depend, 165, 159–167. doi:10.1016/j.drugalcdep.2016.06.006
- Norwegian Directorate of Health. (2010). Nasjonale retningslinjer for Legemiddelassistert rehabilitering ved opioidavhengighet. [National Guidelines for opioid maintenance treatment]. Retrieved from https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/100/IS-1701-Legemiddelassistert-rehabilitering-ved-opioidavhengighet.pdf
- Nosyk, B., Guh, D. P., Sun, H., Oviedo-Joekes, E., Brissette, S., Marsh, D. C., … Anis, A. H. (2011). Health related quality of life trajectories of patients in opioid substitution treatment. Drug and Alcohol Dependence, 118(2), 259–264. doi:10.1016/j.drugalcdep.2011.04.003
- Padaiga, Z., Subata, E., & Vanagas, G. (2007). Outpatient methadone maintenance treatment program. Quality of life and health of opioid-dependent persons in Lithuania. Medicina (Kaunas, Lithuania), 43(3), 235–241.
- Pasareanu, A. R., Opsal, A., Vederhus, J.-K., Kristensen, Ø., & Clausen, T. (2015). Quality of life improved following in-patient substance use disorder treatment. Health and Quality of Life Outcomes, 13, 35. doi:10.1186/s12955-015-0231-7
- Pavot, W., & Diener, E. (2008). The satisfaction with life scale and the emerging construct of life satisfaction. The Journal of Positive Psychology, 3(2), 137–152. doi:10.1080/17439760701756946
- Pedrero-Perez, E. J. (2017). Methadone dosage and its relationship to quality of life, satisfaction, psychopathology, cognitive performance and additional consumption of non-prescribed drugs. Adicciones, 29(1), 37–54.
- Peles, E., Schreiber, S., & Adelson, M. (2006). Variables associated with perceived sleep disorders in methadone maintenance treatment (MMT) patients. Drug and Alcohol Dependence, 82(2), 103–110. doi:10.1016/j.drugalcdep.2005.08.011
- Ponizovsky, A. M., Margolis, A., Heled, L., Rosca, P., Radomislensky, I., & Grinshpoon, A. (2010). Improved quality of life, clinical, and psychosocial outcomes among heroin-dependent patients on ambulatory buprenorphine maintenance. Substance Use & Misuse, 45(1–2), 288–313. doi:10.3109/10826080902873010
- Pud, D., Zlotnick, C., & Lawental, E. (2012). Pain depression and sleep disorders among methadone maintenance treatment patients. Addictive Behaviors, 37(11), 1205–1210. doi:10.1016/j.addbeh.2012.05.025
- Redden, S. M., Tracy, S. J., & Shafer, M. S. (2013). A metaphor analysis of recovering substance abusers’ sensemaking of medication-assisted treatment. Qualitative Health Research, 23(7), 951–962. doi:10.1177/1049732313487802
- Reinert, D. F., & Allen, J. P. (2007). The alcohol use disorders identification test: An update of research findings. Alcoholism, Clinical and Experimental Research, 31(2), 185–199. doi:10.1111/j.1530-0277.2006.00295.x
- Robinson, S. M., Sobell, L. C., Sobell, M. B., & Leo, G. I. (2014). Reliability of the timeline followback for cocaine, cannabis, and cigarette use. Psychology of Addictive Behaviors, 28(1), 154–162. doi:10.1037/a0030992
- Rudolf, H., & Watts, J. (2002). Quality of life in substance abuse and dependency. International Review of Psychiatry, 14(3), 190–197. doi:10.1080/09540260220144975
- Shion, L. D., Sambamoorthy, V. R., Ying, D. L. S., & Aznal, S. S. S. (2014). Assessment effects of maintenance therapy on quality of life of opiate abusers. ASEAN Journal of Psychiatry, 15(2), 131–139.
- SKDE. (2017). PROM. Retrieved from https://www.kvalitetsregistre.no/artikkel/information-english#idx-1
- Strada, L., Vanderplasschen, W., Buchholz, A., Schulte, B., Muller, A. E., Verthein, U., & Reimer, J. J. Q. (2017). Measuring quality of life in opioid-dependent people: A systematic review of assessment instruments. Quality of Life Research, 26(12), 3187–3200. doi:10.1007/s11136-017-1674-6
- Sun, H. M., Li, X. Y., Chow, E. P. F., Li, T., Xian, Y., Lu, Y. H., … Zhang, L. (2015). Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: A systematic review and meta-analysis. BMJ open, 5(1), e005997–e005997. doi:10.1136/bmjopen-2014-005997
- Tiffany, S. T., Friedman, L., Greenfield, S. F., Hasin, D. S., & Jackson, R. (2012). Beyond drug use: A systematic consideration of other outcomes in evaluations of treatments for substance use disorders. [Research Support, N.I.H., Extramural]. Addiction, 107, 709–718. doi:10.1111/j.1360-0443.2011.03581.x
- Tomyn, A. J., Tyszkiewicz, M. D. F., & Cummins, R. A. (2011). The personal wellbeing index: Psychometric equivalence for adults and school children. Social Indicators Research. doi:10.1007/s11205-011-9964-9
- Torrens, M., San, L., Martinez, A., Castillo, C., Domingo-Salvany, A., & Alonso, J. (1997). Use of the Nottingham health profile for measuring health status of patients in methadone maintenance treatment. Addiction, 92, 707–716. doi:10.1111/j.1360-0443.1997.tb02937.x
- Tran, B. X., Nguyen, L. H., Nong, V. M., Nguyen, C. T., Phan, H. T. T., & Latkin, C. A. (2016). Behavioral and quality-of-life outcomes in different service models for methadone maintenance treatment in Vietnam. Harm Reduction Journal, 13(ArtID 4), 13.
- WHO. (1995a). Field trial WHOQOL-100 February 1995: The 100 questions with response scales. Geneva: World Health Organization. Retrieved from http://www.who.int/iris/handle/10665/77084
- WHO. (1995b). The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. doi:10.1016/0277-9536(95)00112-K
- WHO. (1996). WHOQOL-BREF: Introduction, administration, scoring, and generic version of the assessment P. o. M. health. Geneva: WORLD HEALTH ORGANIZATION.
- Winklbaur, B., Jagsch, R., Ebner, N., Thau, K., & Fischer, G. (2008). Quality of life in patients receiving opioid maintenance therapy: A comparative study of slow-release morphine versus methadone treatment. European Addiction Research, 14(2), 99–105. doi:10.1159/000113724
- Xiao, L., Wu, Z., Luo, W., & Wei, X. (2010). Quality of life of outpatients in methadone maintenance treatment clinics. Journal of Acquired Immune Deficiency Syndromes, 53, S116–S120. doi:10.1097/QAI.0b013e3181c7dfb5
- Zubaran, C., & Foresti, K. (2009). Quality of life and substance use: Concepts and recent tendencies. Current Opinion in Psychiatry, 22(3), 281–286. doi:10.1097/YCO.0b013e328328d154