Abstract
Severe Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2) known as Coronavirus surfaced in late 2019. It turned out to be a life-threatening disease and is causing chaos all around the world. The World Health Organisation (WHO) declared it a pandemic in March 2020. To handle COVID-19 related problems, research in many areas of science was introduced. Machine learning (ML), being one of the most successful stories in recent times is widely used to solve a variety of problems in our everyday life. Here, an overview of machine learning that tackles the pandemic is discussed in the beginning. Various datasets related to COVID-19 are also explored. Diagnosis of this viral disease using CT-Scans, X-ray images, sound analysis and blood tests using machine learning are presented in-depth. Drug and vaccine development using machine learning for COVID-19 are also discussed. Pandemic management and control were also examined. The main objective of this paper is to conduct a systematic review of machine learning applications that fight the deadly virus. This paper helps the researchers to understand and analyse the data trends related to COVID-19 and also prepare for a future outbreak which might happen due to new strains of COVID-19. Challenges and directions for the future are also provided.
PUBLIC INTEREST STATEMENT
COVID-19 has been identified as a potentially fatal disease that is wreaking havoc all around the planet. The RT-PCR (Reverse Transcription Polymerase Chain Reaction) test is the golden standard for COVID-19 diagnosis. It is, however, prone to false negatives and erroneous outcomes. As a result, CT scans, X-rays, blood tests, and sound analyses can all be used in the diagnosis of COVID-19. In the health care industry, machine learning applications are frequently deployed since they are renowned to deliver accurate results after being trained. They can be used in the field of drug and vaccine development too. The preceding investigations have demonstrated that the application of Machine Learning and Deep Learning in the diagnosis of COVID-19 is particularly beneficial. Every day, a large volume of research is conducted. Therefore, it is critical to classify and group the literature utilising the systematic literature review procedure. This aids in bridging the gap between researchers and the technology at hand.
1. Introduction
Commonly known as Coronavirus (SARS-COV-2), is a very infectious disease which has spread all over the globe. This virus belongs to the Coronavirdae family. Cough, fever, shortness of breath, headache, muscle ache, loss of smell and taste can all be symptoms of COVID-19 (Razai et al., Citation2020). The origin of this virus is still not known, but studies have concluded that it is linked to Beta-coV genera, a virus which infects rodents and bats (Cascella et al., Citation2020). Wuhan city, China reported the first case in December 2019. 182,276,267 cases have been confirmed and 3,947,630 deaths have been reported as of 29 June 2021. Various health industries are looking at new techniques and methods to tackle this pandemic. Data Science is currently one of the hottest trends in the modern era. It covers artificial intelligence, machine learning, deep learning, algorithms, modelling, statistics and simulation. It has been argued that Artificial Intelligence (AI) will play a crucial role to help fight against this highly infectious virus. It also provides great support to academic and clinical studies (Browning et al., Citation2020). ML has a lot of scope in a variety of fields like engineering, interdisciplinary science, psychology, social analysis, earth observations, hazard mitigations, urbanized locations etc. Various implementations of Machine Learning (ML) ideas were used in applications like tracking people using facial recognition, disinfecting areas using drones (Estrada, Citation2020), medicines and food delivery by automated robots, detection of COVID-19, drug discovery etc. AI’s subset is ML.
Referring to available literatures, the applicability of ML and hybridized models successfully in various field of engineering and natural disasters (Abbaszadeh Shahri, Asheghi et al., Citation2021; Abbaszadeh Shahri, Kheiri et al., Citation2021; Abbaszadeh Shahri & Maghsoudi Moud, Citation2020, Citation2021), psychometric analysis (Orrù et al., Citation2020; Rosenbusch et al., Citation2021), medical and pharmaceutics (Kan, Citation2017; Réda et al., Citation2020; Vamathevan et al., Citation2019), incorporating with graph theory (Abderrahim et al., Citation2014) as well as social sciences (N. C. Chen et al., Citation2018; Grimmer et al., Citation2021; Hindman, Citation2015) have been approved.
ML uses statistical models (Gale, Citation1988) with a minimum amount of knowledge to solve complicated problems. The algorithms include Linear Regression, Logistic Regression (LR), Decision tree (DT), Random Forest (RF), K-Nearest Neighbours (KNN), Support Vector Machine (SVM), K-means clustering, Naïve Bayes (NB) model, etc. Deep Learning (DL) is a subcategory of ML and it concentrates on building Neural Network (NN) models which use feed-forward and backpropagation to learn various data trends. They are playing an important role in battling COVID-19 as well. They aid in the diagnosis of the viral disease and also predict the severity of the same. In the pharmaceutical industry, these models are used to observe the genetics and mutations of COVID-19 to enhance drug prediction and vaccination. AI learns various disease transmission models which are used in predicting outbreaks, public monitoring, epidemic detection and patient tracking. We first analyse a few papers which have surveyed and reviewed machine learning methods to tackle COVID-19. In section 3, a brief overview of different ML algorithms is presented along with its applications that tackle COVID-19. Emphasis is given to supervised, unsupervised and reinforcement learning algorithms. In section 4, we look at the existing datasets and other resources. In section 5, the contribution made by the various data scientists in diagnosing COVID-19 are explained. Medical images which include Computerized Tomography (CT) scans and X-ray images to detect this deadly virus are discussed. Recent discoveries have proved COVID-19 can also be detected using sound analysis and breathing patterns. Haematological parameters obtained using routine blood tests can be used to diagnose COVID-19 too and severity progression can also be monitored by using laboratory and demographic parameters. The development of various vaccines and drugs for COVID-19 with the help of ML are discussed in section 6. Different ways to control and manage the pandemic wisely are explained in section 7. In section 8, we provide a brief insight on key issues and future scope for researchers. In section 9, we conclude this paper. The structure of the paper can be seen in .
2. Related work
A number of researchers have already tried to review the applications of machine learning to tackle the pandemic. Chamola et al., (Chamola et al., Citation2020) reviewed the applications of IoT, blockchain, drones, AI and 5 G to fight COVID-19. Clinical features, diagnostic procedures, various transmission mechanisms, managing and limiting the damage from this virus using the above technologies were discussed in the paper. Pandey et al., (Panday, Citation2020), surveyed automatic CT scans along with image processing and DL to diagnose COVID-19. She explored 74 papers that included specified preprocessing techniques, classification methods and experimental results. Mohamadou et al., (Mohamadou et al., Citation2020), used a mathematical approach along with AI to explore various datasets and also predict the pandemics that might occur in the future. It was also found that most of the AI implementations on X-ray and CT images were based on CNN models. Modern approaches to tackle COVID-19 were discussed in (A. Kumar et al., Citation2020). Effective tracking and patient quarantine were effectively done using various applications in this paper. The application of ML to tackle COVID-19 was surveyed in (J. Chen et al., Citation2020b). Disease diagnosis, drug and vaccine development, pathogenesis and virologic studies with the help of ML were looked into. Deep learning techniques to manage the pandemic were discussed in (Sufian et al., Citation2020). Systematic study of Deep Transfer Learning (DTL) and Edge Computing (EC) along with DL was presented along with a DTL pipeline to mitigate future COVID-19 outbreaks. An overview of speech and language processing to tackle COVID-19 was discussed in (Deshpande & Schuller, Citation2020). The paper further explains non-speech modalities that may complement further audio and speech analysis. A review regarding the use of ML applications in battling pandemics was discussed in (Lalmuanawma et al., Citation2020). The paper targeted medication, screening, treatment, forecasting, prediction, contact tracing and vaccination procedures for the pandemic. The disadvantages of AI in battling this deadly disease were discussed in (Naudé, Citation2020a). The paper discussed about the lack of data available in clinical research and also about data privacy and rigorous AI-human interaction. The involvement of big data along with AI to fight the pandemic was reviewed in (Pham et al., Citation2020). The research emphasized the use of the above techniques in preventing the severe effects caused by the pandemic. Chest x-ray images along with AI for detection of COVID-19 were reviewed in (Ilyas et al., Citation2020; Tsikala Vafea et al., Citation2020). Deep learning architecture models like Inception net, Resnet, Google net etc., were discussed here. Automatic COVID-19 detection is very important to prevent the spread of the virus through contact. A short review regarding the applications of AI for COVID-19 were seen in (Ahuja et al., Citation2020; Vaishya et al., Citation2020). Proper screening, predicting future patients along with early diagnosis and detection of this infectious virus were reviewed in the paper. The reduction of workload among health care workers with the help of ML was also discussed. Applications of AI in developed countries to combat COVID-19 were discussed in (Naudé, Citation2020b; Unberath et al., Citation2020). The study claimed that AI is a very powerful tool to reduce the economic and health impacts of the pandemic. Social control and drug/vaccine development can be enhanced using the applications of AI. In another study (Nguyen et al., Citation2020), applications of AI along with blockchain to combat COVID-19 were discussed. Blockchain helped in managing the pandemic by protecting user privacy and enabling early outbreak detection, whereas AI was used to identify various treatments and played a vital role in drug manufacturing according to the study. Image processing along with machine learning to process medical images for COVID-19 was reviewed in (Ulhaq et al., Citation2020). This survey paper provides an initial review on the available articles on computer vision and COVID-19. Management of COVID-19 using AI was discussed in (Shaikh et al., Citation2021). Epidemic models were surveyed in (Shinde et al., Citation2020). The paper explained forecasting techniques that was divided into two types, mathematical models with stochastic theory and machine learning techniques. This helped in analyzing various trends which led to the spread of the disease. Sharma et al., (Sharma & Gupta, Citation2021), surveyed ML applications related to COVID-19 diagnosis. The study was based on the Indian population. Future diagnosis with the help of AI to make medical decisions was discussed. Review on the applications of big data and AI to manage the pandemic were discussed in (Barragán & Manero, Citation2020). The above technologies were used to handle large volumes of data obtained from epidemic outbreak monitoring, public health surveillance, regular situation briefing, trend forecasting from health facilities and government institutions. Forecasting the number of cases using machine learning was explored in (Ahmad et al., Citation2020). Various researches about the prediction of the number of confirmed cases using ML was reviewed in this paper. A brief overview of recent studies to tackle the viral disease using ML was performed in (Bullock et al., Citation2020). Kannan et al., (Kannan et al., Citation2020), used ML to find and discover new drugs that could potentially cure COVID-19. In this paper, vaccine development using ML techniques was discussed in depth. Critical patients were managed using AI in (Rahmatizadeh et al., Citation2020). ML was used with other diagnostic factors to predict whether a patient would require an ICU facility or not. Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) scans with the aid of ML were used in the diagnosis of COVID-19 (Dong et al., Citation2021). The paper indicated that imaging characteristics and their changes help in the diagnosis of this viral disease. ML methods were desperately needed to bring out the best of imaging, claimed the study. Chest X-ray (XSR) images along with AI were used to recognize COVID-19 patients in (Goodwin et al., Citation2020). Even though there are so many researches, cooperation must always exist between data scientists when it comes to exchanging data, tools and code (Luengo-Oroz et al., Citation2020; Peiffer-Smadja et al., Citation2020). The main challenges in battling COVID-19 were studied in (Van der Schaar et al., Citation2021) and they also discussed the use of ML to solve those problems independently. Shi et al., (Shi et al., Citation2020) used machine learning techniques for data acquisition, diagnosis and prognosis of infected patients. Biological data mining was used to perform COVID-19 detection in (Dasgupta et al., Citation2020). Another paper (Tayarani N, Citation2021), discussed the uses of AI in battling COVID-19. In (CitationChamola et al.,), disaster management using ML approach was discussed. Alafif et al., (Alafif et al., Citation2021), surveyed AI applications in COVID-19 diagnosis. In (Latif et al., Citation2020), a review of DL techniques to combat COVID-19 was discussed in detail. summarizes the existing literature that uses ML applications to tackle COVID-19.
Table 1. Existing literature of the application of artificial intelligence and machine learning in battling COVID-19
RT-PCR (Reverse Transcription Polymerase Chain Reaction) test is the golden standard to diagnose COVID-19. However, it is also prone to false negatives and inaccurate results. It might also not be able to detect newer strains of COVID-19 in the future. Hence the use of CT-Scans, X-rays, blood tests and sound analysis should also be used in COVID-19 diagnosis. They can also be used in events, such as a pandemic peak, since the RT-PCR test takes a considerable amount of time to give results. These methods can also be used along with RT-PCR tests to increase the sensitivity.
Machine learning applications are constantly used in health care industries. They can be trained with a large amount of data. Once trained, they are known to produce accurate outputs. They can assist the health care workers, since these algorithms are extremely fast and efficient. The above studies have proved that the use of Machine Learning and Deep Learning in the diagnosis of COVID-19 are extremely helpful. A huge amount of research is happening each day; hence it is very important to classify and group the literature using the process of systematic literature review. This helps in bridging the gap between the researchers and the technologies involved. This paper aims to answer the following questions:
How does the use of cutting-edge machine learning techniques in COVID-19 improve system accuracy?
Which of the various COVID-19 diagnostic techniques are better when compared to each other?
What are the current challenges and the possible future research trends?
3. Machine learning overview
This section presents a brief recapitulation of the ML algorithms that help in tackling COVID-19. The application of ML in tackling COVID-19 is very important for the current situation. Supervised learning, unsupervised learning and reinforcement learning are the main types of ML algorithms.
3.1. Supervised learning
The training data is labelled in supervised learning ML algorithms. The set of output/labels are also given. These algorithms learn from the dataset and after training a certain amount of data, predict accurate outputs.
3.1.1. Classification
Trained data is grouped into one of the predefined classes (Soofi & Awan, Citation2017). One of the disadvantages of these algorithms is their inability to handle missing data. But fortunately, these missing data can be replaced with existing data (Kantardzic, Citation2020). There are many classification algorithms which are being used to analyse COVID-19 trends. The following are some of them.
K Nearest Neighbours (KNN)—Classification is based on the location of the data points. Similar objects are grouped together based on the number of neighbours. The classification is non-parametric. No assumptions are made about the data. It is also called a lazy learner algorithm since its learning procedure is slow and the action is performed only at the time of classification. A user-defined k is set as the minimum number of neighbours required. Generally, when the value of k is higher, the predictions are more trustworthy. Weights are attached to the neighbours to increase accuracy during classification. KNN was used in (Ginantra et al., Citation2020) to detect respiratory infections. Yin et al., (Yin et al., Citation2018), used KNN to detect serious influenza. Locations of the infected users were tracked in (Cho, Citation2016) using KNN.
Support Vector Machine (SVM)—A hyperplane is used to classify the data into different groups. SVM finds the maximum marginal distance to find the minimum gap among data points. Hyperplanes act as boundaries and separate the data points into classes. A single line exists when there are only two attributes. A 2D plane is generated when the input size is increased to three. When the number of features increases, it gets very difficult to picture the hyperplane. Mori et al., (Mori et al., Citation2016), used SVM to predict the outbreak of disaster for a specific location. SVM was used with IoT (Internet of Things) and CNN (Convolutional Neural Networks) for the diagnosis of COVID-19 (Le et al., Citation2021).
Naïve Bayes—Bayes’ theorem can also be used to classify the dataset. All the features which get classified are assumed to be completely independent of each other, hence the name naïve. Splitting of data is done into two components, feature matrix and response vector. In the feature matrix, all data is stored in the form of rows, and in response vector, the outcome class is defined. In (Sadhukhan et al., Citation2018) and (Assery et al., Citation2019), Naïve Bayes classifier has been used to group tweets. It helped manage social networking problems during the period of the pandemic.
Logistic Regression—It is used to predict the categorical variable (dependant variable) based on one or more independent variables using a sigmoid curve as a cost function. Sigmoid function (Logistic function) is a S-shaped curve that classifies the data into one of the classes. Logistic regression can be used in binomial, multinomial and ordinal classification. Mohammadi et al., (Mohammadi et al., Citation2021) used ANN and LR to classify COVID-19 patients in Iran. In (Bhandari et al., Citation2020), Logistic Regression was used to predict the mortality rate from various blood and clinical parameters. Forecasting of COVID-19 in Kuwait was done using LR in (Almeshal et al., Citation2020).
Decision Trees—Leaf nodes predict the outcome, decisions are taken by the branches and the features represent internal nodes of a decision tree. Decision trees distribute instances by assembling them down the tree from the root to leaf nodes, which provides the classification of the instance. In (Elhoseny, Citation2019), the location of the users has been detected using decision trees during pandemics. In (Chen & Liu, Citation2021), the prediction of different factors which led to psychological distress during the pandemic was discussed with the help of decision trees. A hybrid face mask detection application was developed by using decision trees in (Loey et al., Citation2021).
Random Forests—Classification using a decision tree can lead to overfitting when the data is large. These limitations can be fixed by random forests. Different decision trees are classified and then merged together to improve accuracy. This method is called “bagging”. COVID-19 health prediction was made using the RF algorithm in (Iwendi et al., Citation2020). The random forest machine learning approach was used to estimate the spatial-temporal distribution of COVID-19 daily instances around the world (Yeşilkanat, Citation2020).
Artificial Neural Network (ANN)—They are a completely connected network and are multi- layered. The layers include an input layer, an output layer and many hidden layers. The nodes in one layer are attached to the previous and next layers. Inputs pass through an activation function. The output of one layer becomes the input for the next layer. ANN along with IoT was used to detect the location of the user (Luoh, Citation2013). Here the data was limited, yet there was a high accuracy. In (Polese et al., Citation2020), ANN was used to detect the exact group of people present in an area.
Deep Neural Network (DNN)—DNN is an adaptive model and also offers creativity since neural networks are generally monotonous. The total number of nodes to analyse results are very large. DNN consists of three layers- Input, output and many masked levels. Progressive learning and the ability to modify their results are the reasons DNN is used. Chhikara et al., (Chhikara et al., Citation2021), used DNN for emergency crowd evacuation. It is important to transfer healthy people to non-infectious zones.
Convolutional Neural Network (CNN)—CNN is a better algorithm to classify images since it has a
better accuracy and capturing orientation. They have many different layers called pooling layer, convolutional layer, fully connected layer, etc. A CNN based model (More et al., Citation2020) was used with IoHT (Internet of Health Things) for diagnosing people with COVID-19.
3.1.2. Regression
The regression technique is a predictive learning feature that maps a data object to a predictive variable with real meaning (Gutierrez et al., Citation2016). Regression uses methods of statistics to establish a relationship between the target and predictor variable. Regression also helps us to model the association between a dependent and independent variable. Variables like age, temperature, salary, etc. can be easily forecasted after training a certain amount of data.
Linear Regression—Linear regression is a simple algorithm that is used for predictive analysis. It shows the linear relationship between dependent and independent variables. If only one input exists, such a model is called simple linear regression and if more than one input exists, the model is termed a multiple linear regression model. A multivariate linear regression model was used to predict new active cases of coronavirus disease (COVID-19) (Rath et al., Citation2020). Predictive modelling of COVID-19 positive samples in Nigeria was made using a linear regression model (Ogundokun et al., Citation2020).
Polynomial Regression—Non-linear dataset can be modelled using polynomial regression. A non-linear curve is set for the dependent and independent variables. Polynomial features of a given degree are obtained from original features and then the model is developed using linear regression. COVID-19 epidemic estimates in India based on the polynomial regression model were analysed in (Pandey et al., Citation2020). The use of hierarchical polynomial regression models to forecast COVID-19 spread at the worldwide scale was used in (Ekum & Ogunsanya, Citation2020).
Support Vector Regression—Support Vector machines can be used for classification as well as regression. A hyperplane with maximum marginal distance is determined to fix the maximum number of data points near the margin. Maximum data points must be within the boundary lines and the maximum number of data points must be included in the hyperplane. It was used in the short-term prediction of COVID-19 confirmed cases in Brazil (Ribeiro et al., Citation2020).
Ridge Regression—Ridge regression includes a small amount of bias which helps in getting better long-term predictions. This bias is called the ridge regression penalty. The penalty can be calculated by the individual features. High collinearity between independent variables is the use case of the algorithm, since both linear and polynomial regression would fail in the above condition. The model can also be used if there are more samples than parameters. It also reduces the complexity of models; hence it is also a regularization technique. Forecasting the development of the COVID-19 epidemic using a hybrid polynomial-Bayesian ridge regression model was discussed in (Saqib, Citation2021).
3.2. Unsupervised learning
The data is unlabelled in unsupervised learning. The user does not know the pattern of the data. The algorithms use distinct techniques to analyse the information structure. The most common algorithm which uses unsupervised learning is clustering.
K-Means—Data is divided into different clusters. Initially, total number of clusters are assigned and random centroids are chosen among the dataset. In each iteration, the centroids are updated. Either Euclidean distance or cosine distance is used to calculate the similarity score. Projection of the number of reported COVID-19 cases using k-means was discussed in (Vadyala et al., Citation2020). The prediction of COVID-19 cases using the K-Means algorithm in the United States of America was discussed in (Zhang & Lin, Citation2021).
K-Medoids—It is used when there are a lot of outliers in the data. Data points are chosen randomly as a median. The rest of the data points are placed among these medoids depending upon the minimum distance. After certain iterations, we get medoids which successfully cluster the dataset. Deployment of Data Mining Techniques which included k-medoids algorithm in National Food Security in Indonesia during the COVID-19 pandemic was discussed in (Elsi et al., Citation2020).
Fuzzy C-Means—Centroids are randomly assigned and data is initialized randomly to these clusters. This algorithm operates by assigning membership to each data point corresponding to each cluster centre based on the distance between the cluster centre and the data point. More the data is near the cluster centre, more is its membership towards the particular cluster centre. A development of an intelligent model based on the Lévy slime mould algorithm and adaptive fuzzy C-means for detecting COVID-19 infection in chest X-rays has been developed in (Anter et al., Citation2021). ROI extraction in CT lung images of COVID-19 using Fast Fuzzy C means clustering was discussed in (S. N. Kumar et al., Citation2021). This helped the radiologists and other medical professionals.
3.3. Reinforcement learning
Maximizing the reward by taking suitable action in a particular situation is called reinforcement learning. Various machines and software try the best path or behaviour for a given situation in this method. In supervised learning, the answer key is available to the data during the training phase, whereas, in reinforcement learning, the reinforcement agent determines the course of action and no answer key is available to guide the model. The models learn from experience even in the absence of training data set.
Q-learning—Sequential decision making is used in Q-learning. For each input, the best solution is calculated and the corresponding input always depends upon the previous output. Objective function Fπ can be maximized or minimized based on various scenarios. π corresponds to the policy and P defines a state. Its optimal policy comes from its interactions with the environment. A strategy for the prevention of COVID-19 affected patients using multi-robot collaboration and the Q-learning approach was presented in (Sahu et al., Citation2021). A Novel Methodology Based on Deep Q-learning/Genetic Algorithms for Optimizing Covid-19 pandemic government actions was discussed in (Miralles-Pechuán et al., Citation2020).
Markov’s decision process—Learning from interactions to achieve a specific goal is the fundamental technique in this algorithm. The environment and the reinforcement agent continually interact with each other, the agent selects the action and the response to these actions
are given by the environment, which in turn presents new scenarios to the agent. The epidemiological Markov model was used to analyse the COVID-19 pandemic and clinical risk factors of patients in (W. Zhang et al., Citation2021).
4. Datasets and resources
Datasets are very important when it comes to research. They should be easily accessible too. We begin with useful public datasets for COVID-19. They are summarised in .
Table 2. Prominent COVID-19 datasets
4.1. COVID-19 case data
COVID-19 patients and their corresponding locations can help keep track of the pandemic growth in many areas. Many countries are supporting data collection and sharing information related to COVID-19. John Hopkins University collects the data regarding the positive cases which occur each day. It also collects information regarding the death rate and also the number of patients cured (CSSEGISandData, Citation2021). Kaggle also updates the COVID-19 data regularly (sudalairajkumar Data, Citation2021). Here, other details of patients, including location, reporting date, etc. are shared. nCOV2019 (nCoV2019Data, Citation2021) contains important information like national health reports of the COVID-19 victims. Details like date of confirmation, travel history, list of symptoms and geo-locations are shared. New York Times gives state wise details which consist of positive cases and casualties each day (Nytimes, Citation2021). The above datasets are given by the government but community datasets are also available. People also report new infections using their social network (B et al., Citation2021). Applications which thrive on data visualization can use the dataset (Koubaa, Citation2021). The limitation of these datasets is that they belong to a particular country most of the time.
4.2. Textual data
Online sources are used to collect a huge amount of data which can be used to understand the nature of the virus. An important source is social media. Discussions made about COVID-19 are already available. Tweet ID’s (E. Chen et al., Citation2020) and tweet text data (Smith, Citation2020) are being used by various communities. These datasets can be used with NLP (Natural Language Processing) to monitor the spread of this deadly virus (Aramaki et al., Citation2011; Culotta, Citation2010; Lampos et al., Citation2010). Sharma et al. (Sharma et al., Citation2020) has also separated COVID-19 data after summarising 5 million tweets. Zarei et al. (Zarei et al., Citation2020) have used Instagram to analyse 5300 posts related to COVID-19. Academic publications have also created a lot of textual information. Clinical studies are used to extract information (Zhao et al., Citation2020). NLP models are used for this purpose (Manning, Citation2016). Allen Institute has contributed 45,000 articles which relate to COVID-19 (Allen-Institute, Citation2020). NCBI (National Centre for Biotechnology Information) is also contributing with data (NCBI, Citation2020). WHO has collected recent research publications and has dedicated an entire database to it (WHO, Citation2020). Wikipedia has also collected substantial information about COVID-19 which can be easily downloaded for analysis (Citation2020).
4.3. Medical data
Medical data is used for this diagnosis and treatment of COVID-19. X-rays and pathology reports can be used for prognosis. There are a few open-source X-ray scans of COVID-19 patients (Wang & Wong, Citation2020). They can be used to assess and diagnose infections using computer vision (Mery, Citation2015). There are other X-ray datasets as well, such as (Citation2020; Cohen et al., Citation2020; Mvd, Citation2020). These datasets cannot be easily understood by a non-biological student. Thus, we require help from radiologists and clinicians to properly label the data. The datasets are small and deep learning techniques might not be efficient on them. Along with X-rays, CT scans are also used for COVID-19 diagnosis. A lot of CT scan datasets are already available. In (MegSeg, Citation2020), CT scans of 60 patients were taken. A larger dataset which includes 288 CT scans is present in (J. Zhao et al., Citation2020). The United Kingdom also provides COVID-19 chest X-rays and CT scans of various patients who were infected (Nhsx, Citation2020). Leeds University Institute[119], UK NHSx [120] and Ellis Alicante (E. A. Foundation, Citation2020) also provide images of infected lungs of COVID-19 patients. Genomic sequencing datasets are also available. The datasets RCSB (Research Collaboratory for Structural Bioinformatics) data (Goodsell et al., Citation2020), And GHDDI (Global Health Drug Discovery Institute) (Zhavoronkov et al., Citation2020a) analyse the structure of RNA, the structure of spike protein, etc.
4.4. COVID-19 data from developing countries
Countries like Algeria, Kenya, Egypt, South Africa, Nigeria and Tanzania are sharing data. Zhao et al. (Z. Zhao et al., Citation2020) studied the COVID-19 analysis for African countries like Senegal, South Africa and Kenya. The dataset provides the number of cases occurring each day, deaths and the recovered patient details. West Africa has also provided the dataset (Martinez-Alvarez et al., Citation2020). State-wise analysis along with other demographics are provided by these datasets.
4.5. Other datasets
There have been other useful datasets which have become prominent during the time of the pandemic. For example, air quality improved during lockdown since there were very few vehicles and the industries had shut down. Air quality of six major cities had improved rapidly due to the lock down (Cadotte, Citation2020). The data is available to the public (W. Inc., Citation2020). Mobility trace data is available in [128]. In (Wurtzer et al., Citation2020), samples of wastewater were taken. It was found that 6 samples tested positive for COVID-19.
5. Medical diagnosis OF COVID-19 using ML
COVID-19 cases are increasing every day. Medical images have started to play an important role in the diagnosis of COVID-19. CT scan and X-ray of patients using AI have been used to facilitate health care personnel. These images are tested and classified based on geographic infection classification, organ recognition and disease classification. The prediction of diagnosis becomes faster using these methods. The prognosis of the disease can also be easily monitored.
5.1. COVID-19 detection using lung CT scan
CT scans are used to diagnose COVID-19 along with RT-PCR (Real-Time Polymerase Chain Reaction) tests. It has been found that the infection generates ground-glass opacities and long periphery consolidations. These can also occur before the lab test. Hence, health care professionals can use CT scans to diagnose the disease when a lot of people are being tested. The scan also shows the severity of the affected lungs and also how the illness can progress. The doctors can make medical decisions based on it. Lung defects because of COVID-19 are unique and can be easily diagnosed. The CT scan can take up to 15 minutes, but the AI can validate the extent of severity within seconds [143]. The function of CT Scan can improve using Advanced Image Processing and ANN by training a large amount of CT scan images of the COVID-19 patients. CT imaging tests with AI normally have the following steps, division of Region of Interest (ROI), pulmonary tissue removal, infected region removal and finally, classification of COVID-19. The images of lung organs and ROIs combined with AI-based testing turns out to give favourable results.
ROIs can be used to find ulcers, bronco pulmonary segments, lobes of the lungs infected, etc. The CT images are classified using various types of DL networks. E.g.: V-Net, U-Net, VB-Net, RPN have been used. After the primary CT scan is taken, deep CNN is used to evaluate the characteristics of the image concerning SARS-CoV-2 victims. The CNN based algorithm obtained an Area Under Curve (AUC) of 92%. Detection of patients using AI systems enhanced and it correctly classified 17 patients out of 25(65%) and the radiology department confirmed that they were negative (Mei et al., Citation2020). The CNN model predicted 13 out of 25 (52% of the images), as positive. The clinical model classified 16 out of 25(64%), as COVID-19 positive. The combination of the models classified 17 out of 25 as COVID-19 positive. A research team of the Tianjin Medical University Cancer Institute and Hospital had obtained CT scans of 180 patients who had severe pneumonia even before the pandemic (PhysicsWorld, Citation2020). CT scans of 79 positive COVID-19 patients were taken in (Wang et al., Citation2021a). A CNN based model was trained using these images. An accuracy of 89.5 % was obtained after testing the images. The radiologists who identified the images were only 55% correct. RADLogics algorithm (Scudellari, Citation2020) was used to monitor the condition of diagnosed COVID-19 patients using CT-scan imaging. A study (K. Zhang et al., Citation2020) used DL to train CT scan images to search for COVID-19 infection among patients admitted to the hospital. A few researchers trained 532,000 CT images to train their AI-based model. The feature they were concentrating on was “tell-tale lesions” which was unique for COVID-19 patients. The AI model had an accuracy of 85% and successfully differentiated COVID-19 patients from pneumonia. For radiologists, it is very difficult to distinguish between regular pneumonia and the disease which led to the pandemic. Hence a company, VIDA Diagnostics (VIDA. LungPrint Clinical Solutions, Citation2020), created a LungPrint device which uses AI to analyse CT scans which correctly identified all respiratory conditions, including COVID-19. In (Analytics, Citation2020), companies NLH and NVIDIA created a DL model to diagnose COVID-19 using CT scans. The datasets came from Italy, China and Japan. 2724 samples were taken from 2619 patients. Two models were developed (Full 3D, Hybrid 3D). These models were trained to predict COVID-19 by using lung CT Scan images. The hybrid model had a better accuracy of 92%, whereas the full 3D model had 91.7% accuracy. Chen et al. (Chen et al., Citation2020) designed U-Net++ which used a deep learning structure. 46,096 images were collected for model creation and validation. It achieved an accuracy of 95.24%, specificity of 93.5% and 100% sensitivity. Huang et al. (L. Huang et al., Citation2020) used a method called InferRead TM (Thermo Meter) CT which measures the infection severity in the lungs. Pulmonary and lobe extraction, categorization of pneumonia and medical metrics were the three modules incorporated in the tool. Mild, moderate, severe and fatal stages were the four modalities. A deep learning software was trained with 126 images, six were mild, 94 were moderate, 20 severe and 6 fatal cases. CT Scans of 52 COVID-19 patients were analysed by Qi et al., (Qi et al., Citation2020). A methodology called pyradiomics was used to find 1218 traits from each image. CT radiomics models used two algorithms, LR and RF. Pneumonia lesion extracts were used as classifiers during training. They successfully predicted the severity of COVID-19 among patients. The duration of time a person had to stay in the hospital was differentiated. If the person stayed for less than 10 days, it was a short term stay, while the long-term stay was more than 10 days. LR model achieved a sensitivity of 100% and a specificity of 89 %. The RF model showed a sensitivity of 75 % and a specificity of 100%.
5.2. COVID-19 detection using chest X-rays
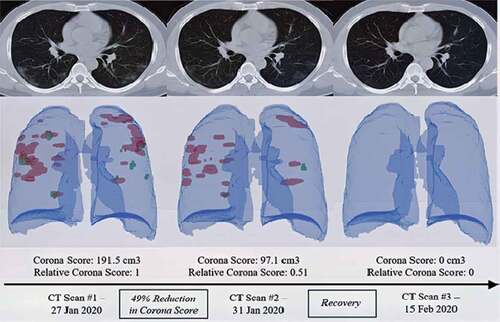
Chest X-ray (CXR) images are an exceptionally useful method to diagnose COVID-19 patients. shows the architecture of DL-based CT image classification for COVID-19 diagnosis (Scudellari, Citation2020). X-ray images are easier to understand and can also be easily acquired unlike CT images. The studies (Basu & Mitra, Citation2020; Pandit & Banday, Citation2020) analyse X-ray images for detection of COVID-19. AI based CXR image testing involves correction of data, training and finally testing of the images. Deep learning algorithms such as CNN, U-Net++, etc. are used for faster detection of COVID-19 from CXR images. CXR machines are less costly than CT scan machines and the images are processed faster. Normally, the X-rays are interpreted manually by radiologists. When it comes to COVID-19 cases, radiologists can detect only 69% of X-rays due to lack of technology (Cristobal.baeza, Citation2020). Trained ML models can detect COVID-19 accurately and quickly.
Figure 2. The RADLogics method calculates the amount of recovery using a specific score based on different computed tomography (CT) scans (Scudellari, Citation2020)
In (Pandit & Banday, Citation2020), a dataset of positive COVID-19 cases, typical pneumonia and non-infectious cases were compared and 1428 CXR scans were taken. A trained model of VCG-16 was used to perform the classification. The results had an accuracy of 96 percent. Many DL algorithms exist which provide accurate results using CXR images in detecting COVID-19. Basu and Mitra (Basu & Mitra, Citation2020) worked on a concept called domain transfer learning to detect COVID-19. A collection of 20,000 CXRs was trained and tested by the Gradient Class Activation Map to detect the viral infection. The CXR dataset was divided into 4 groups, i.e., no disease, other viral diseases, bacterial pneumonia and the dreaded COVID-19. A fivefold cross validation technique was used for disease diagnosis. 100% accuracy was achieved for COVID-19 data and the overall accuracy was 95.33 %. Students of Cranfield University developed an AI-based model to detect COVID-19 using CXR images (Cranfield University, Citation2020a, Citation2020b). To obtain various characteristics of CXR images, various ML and DL techniques were used. The model would detect COVID-19 which would not appear generally to the naked
eye. There were 2 models, the first model differentiated normal patients and patients with pneumonia. The second model distinguished between pneumonia and COVID-19. Using chest X-ray scans for COVID-19 detection, another model (Ozturk et al., Citation2020) using the Darknet-19 model was developed. The sensitivity achieved was 85.35%, specificity 92.18% and f1-score of 87.37%. Researchers of King’s College London General Hospital and a tech company called “Zoe” used AI-based detection to identify COVID-19 pathogens. Symptoms were assessed along with the routine RT-PCR COVID-19 tests (Cranfield University, Citation2020c). 100% sensitivity and 90.5% accuracy were achieved by a model called COVID-19AID (Mangal et al., Citation2020). It used a DNN model which was trained on CXR images that were publicly available. In (Das et al., Citation2020), a CNN model named Truncated Inception Net accurately distinguished between COVID-19 positive and negative cases. The dataset was divided into four categories- Tuberculosis positive, pneumonia positive, COVID-19 positive and healthy patients. A 99.96% accuracy was obtained when detecting COVID-19 from normal cases and pneumonia. While comparing COVID-19 patients with others, the accuracy achieved was 99.92%. Transfer learning was used on CXR images to predict COVID-19 patients by Minaee et al. (Minaee et al., Citation2020). Four CNN models, DenseNet-161, Squeeze Net, ResNet, ResNet50 were used. They used datasets of both healthy and COVID-19 patients. The average specific rate was 90%, sensitivity was in the range of 97.5% for these models. A decision tree classifier was used to classify CXRs in (Yoo et al., Citation2020). There were three decision trees which were trained by CNN. The first tree separated normal X-rays from abnormal ones, the second decision tree separated tuberculosis images from normal images and the third tree separated COVID-19 from tuberculosis images. An accuracy of 98%, 80% and 90% was obtained by the decision trees respectively. GAN (Generative Adversarial Network) was used in a study (Loey et al., Citation2020) along with deep transfer learning to identify COVID-19 patients. There were 4 classes mainly normal, COVID-19, viral pneumonia and bacterial pneumonia. The three transfer models GoogleNet, AlexNet and ResNet18 were used for testing. In the first scenario, all 4 data classes were used, while three classes were used in the second scenario and only two classes were used in the last scenario. COVID-19 class was present in all scenarios. 80.6% accuracy was obtained in the first scenario using GoogleNet. In the second scenario, AlexNet obtained an accuracy of 85.62%. In the third scenario, 100% accuracy was obtained by GoogleNet. To classify COVID-19, 24,678 CXR images were used in (RadBoudumc, Citation2020). CAD4COVID-19-XRay, a deep learning model was trained. Segmentation of lungs was obtained using U-Net and CNN. An AUC of 81% was obtained by the model. The author concluded that it could be useful in low resource systems where there are no proper diagnostics equipment. provides some of the best algorithms for COVID-19 detection using CT and CXR images.
Table 3. Detection of COVID-19 with ML using chest X ray and CT scan images
5.3. Classifying the extent of severity of COVID-19 with ML
Disease progression using CXR images of lungs can be monitored efficiently with the help of ML and DL techniques. In (Cohen et al., Citation2020), studies are being made to determine a severity score based on CXR images. A DenseNet neural network model is used to predict disease progression. 94 images of COVID-19 patients were used for disease progression classification. Two kinds of scores are being used as in . The lung participation and ambiguity are being shown in a single X-ray image. The severity of patients using the DenseNet model can be observed in
Figure 3. DenseNet model to predict severity of COVID-19 from X-rays (Cohen et al., Citation2020)
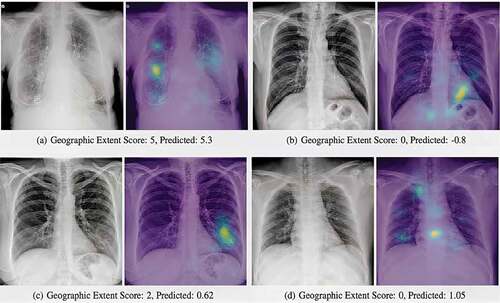
Table 4. DenseNet neural network model to monitor COVID-19 disease progression
For each particular lung, the lung involvement level was calculated by using a degree of unification and ground glass ambiguity. An increase or decrease of supervision, tracking of the effectiveness of treatment in the ICU, can be found out using the score. CSNN (Convolutionary Siamese Neural Network) was used in (Ridley, Citation2020) to generate a score which would predict whether the patient required intubation or not. In (Qi et al., Citation2020), 71 CT scans of 52 COVID-19 patients were obtained. 1218 attributes were extracted from CT images using the methodology pyradiomics. Models using LR and RF were built based on pneumonia lesions. 97% and 92% AUC were obtained during testing of LR and RF models respectively. LR model obtained a sensitivity of 100% along with 89% specificity. RF model obtained 75 % sensitivity and 100% specificity. If the number of days a patient stayed in the hospital was less than 10 days, then it was classified as short term stay, or else it was classified as long term stay. In (Health EUROPA, Citation2020; New York University, Citation2020), a mobile application was developed which used CXR images of 160 patients. The biomarkers would diagnose the severity of COVID-19 from mild (level 0) to extreme levels (level 100).
5.4. COVID-19 detection using sound analysis
Coughing can be a symptom for more than 30 diseases other than COVID-19. So COVID-19 detection using cough alone is difficult. Various sounds like breathing, moaning, heartbeat, etc. can be used for diagnosis. Auscultation was used in the hospitals to collect such signals. gives a brief overview of researches related to COVID-19 detection using sound analysis. Research has already started on how sounds can be recorded and trained to diagnosis healthy and COVID-19 patients. A phone app (Imran et al., Citation2020) used the dataset of 48 COVID-19, 131 pertussis, 102 bronchitis and 76 healthy cough recordings to train the model (Stevens et al., Citation1937). KAs (HospiMedica, Citation2020a), a mobile application was developed by Zensar Technologies. They used AI to monitor patient health by using various cough signatures which were disease-specific. The patients had to answer 15 questions and the cough sound was recorded by the company’s AI platform. Based on the answers and cough sounds, a rating from 1 to 10 was given where 1 meant minimum risk and 10 meant maximum risk. A person’s score was monitored for many days to diagnose COVID-19 accurately. Computer Audition (CA) was combined with AI to study the cough sounds of various COVID-19 patients (Schuller et al., Citation2020). However, there is not much documentation about the effectiveness of this method. A respiratory simulation called BI-AT-GRU (Y. Wang et al., Citation2020) was developed using neural networks. It differentiated 5 types of respiratory sounds such as biots, Cheyne-Stokes, Central-Apnea, Eupnea and Tachypnea. Sputum testing was used in COVID-19 diagnosis. The project was called Coswara (Sharma et al., Citation2020) and it used various biomarkers like cough, breath and other speech sounds. Nine different vowel sounds were recorded. The classification mechanism was still under development when this paper was written. Flusense (Al Hossain et al., Citation2020), a portable device, was developed by the University of Massachusetts, Amherst. It is based on a neural network model which identifies cough and properly detects diseases including COVID-19. The developers claim that this device is being used in many medical centres. Ravelo et al. (Ravelo, Citation2020), recently launched an AI-based system which used cough to diagnose COVID-19. The user had to provide information such as geographic location, symptoms, cough sound, etc. Individuals also had to mandatorily upload the results of their COVID-19 test too. Using these, a DL based algorithm was used to determine COVID-19 infection using the patient cough sounds and other data. Iqbal et al. (Iqbal & Faiz, Citation2020) used a mobile application which recognised suspicious cough sounds to determine the respiratory health of a person. A system which used both coughing and breathing was created by a research group at the University of Cambridge (Brown et al., Citation2020). The breath sounds of COVID-19 patients, healthy people and asthma patients were separated. 7000 users were tested with a minimum of 200 registered COVID-19 patients. LR, Gradient Boosting Trees and SVM models were used. AUC curve along with other parameters were used to find the efficiency of the algorithm classified. The average AUC was around 60%. 367 breath sounds were taken to develop a low-cost cell phone model (Bagad et al., Citation2020). Analysis was done extensively on the breath sound. The model detected pneumonia from non-pneumonia successively.
Table 5. Diagnosing COVID-19 with ML using sound and speech
5.5. COVID-19 prediction using blood tests
Identification of COVID-19 infection is generally done using RT-PCR tests. However, the test takes a considerable amount of time to give results (4–5 hours under ideal conditions). It also needs trained personnel to handle the samples. Its sensitivity is also an issue (unable to avoid false negatives). CT scans and X-rays have been used with the help of ML to provide accurate results. CT scans can be very expensive and might not be affordable for everyone, especially those who live in underdeveloped countries. They can also cause cancer if used excessively. However, X-rays are affordable, but they are also prone to false-negative results (Echenique, Citation2020). Blood test results are available within 15 minutes. They can be used to detect COVID-19 in low resource countries or in events such as a pandemic peak. It can also be used together with RT-PCR test, to increase the sensitivity. Two ML models were used to predict COVID-19 in San Raffaele Hospital (Brinati et al., Citation2020). White blood cells (WBC), platelets, C-reactive protein (CRP), Aspartate Aminotransferase (AST), Alanine Transaminase (ALT), Gamma-glutamyl transferase (GGT), Alkaline phosphatase (ALP), Lactate dehydrogenase (LDH) of 279 patients were taken from routine blood tests which were used to train the ML models. One model was used to predict positive cases and the other to predict negative cases. The accuracy obtained was 82% and 86% respectively. 879 confirmed COVID-19 cases from NHS Trust hospital, England were studied in (Heldt et al., Citation2021). Anonymised demographic data, laboratory results and physiological clinical variables were extracted from EHRs (Electronic Health Report). Multivariate logistic regression, extreme gradient boosted trees and random forest algorithms were used for classification. The severity of COVID-19 cases was predicted based on the blood samples. Blood lactate and creatinine levels played a pivotal role in predicting COVID-19 patient trajectories. AUC scores ranged from 0.76 to 0.87. 72 features from the blood sample of 1624 patients were used for COVID-19 detection with the help of ML models in (Federico et al., Citation2020). AUC obtained by the algorithms were in the range of 0.83 to 0.90. EHR reports of 1357 patients from different European countries were collected to predict COVID-19 in (Tschoellitsch et al., Citation2020). Blood count, electrolytes, creatinine, liver enzymes, bilirubin, c-reactive protein were all included in the final model. An accuracy of 86% percent and an AUC of 0.74 was obtained by this model. In (Kang et al., Citation2021), blood reports of 151 COVID-19 patients from Tongji Medical College, China was collected. ANN algorithms were used to develop the models which predicted the severity in COVID-19 patients. The average AUC obtained was 0.953. 253 samples from 169 patients were collected from four different hospitals in China (Wu et al., Citation2020). 24 haematological parameters and 25 biochemical parameters were selected for analysis. Accuracy of 0.9795 and 0.9697 was obtained from the training and testing set respectively. Prediction of Accurate Respiratory Distress Syndrome (ARDS) was researched in (CitationXu et al.,). Details of 659 COVID-19 patients were taken from 11 different regions in China. The studies concluded that male patients with BMI > 25 were more prone to develop ARDS. Abnormal count of lymphocytes, Creatine kinase, NLR (Neutrophil to lymphocyte ratio), LDH and CRP led to ARDS. DT algorithm achieved the best results. A Gradient Boosting Decision Tree (GBDT) model was used to detect COVID-19 in (Yang et al., Citation2020). 3356 patients (1402 positive, 1954 negative) were observed and 27 blood parameters were used to know the COVID-19 infection status. An AUC of 0.854 was obtained. The external dataset result had an AUC of 0.838. Non-severe COVID-19 patients showed high values for lymphocytes, platelets and eosinophils and had low neutrophils, delta neutrophil index (DNI), NLR and platelet-to-lymphocyte ratio (PLR) in the study (Kazancioglu et al., Citation2020). However, severe patients showed an increasing trend for PLR, platelets and eosinophils. Laboratory data of 120 patients were chosen for this research. An AUC of 0.819, 0.817 and 0.716 was achieved. The research concluded that NLR and PLR values could be used to predict the severity of COVID-19 using different models in ML. Various ML models and ANN was used to identify COVID-19 from full blood counts in (Banerjee et al., Citation2020). The data was used from Israelita Albert Einstein hospital, Brazil. RF, flexible ANN and shallow learning models were used for prediction. The study said that COVID-19 patients tend to fewer less platelets, eosinophils, leukocytes, lymphocytes and basophils. However, an increase in monocytes was noted. An AUC of 94–95% was achieved by the models. gives an overview of other researches which use ML to identify COVID-19 by using routine blood samples. compares all the above models which were discussed.
Table 6. COVID-19 detection using blood tests and ML
Table 7. Comparison of various models to diagnose COVID-19
6. Machine learning for vaccine and drug development
In combination with a huge quantity of data, the capacity for automatic abstract component learning has had a great impact on the efficacy of ML. Vaccination and drug discovery are fields of extreme importance. ML is used to provide behaviour prediction, integrated property prediction and ligand-protein interactions. The vaccines which are used for the treatment of COVID-19 focus on genomics and proteomics study. ML has contributed to intelligent medicine, using which the development of new medicines has taken place.
6.1. Vaccine development using ml for COVID-19
ML and DL help by observing the viral protein structure that helps in the vaccine components dissemination, and also helps medical and biological researchers in reviewing large research papers at a fast pace. Vaccines are mainly available in three types: Vaccines for pathogens (e.g.: Common flu), subunit vaccines (e.g.: shingles, pertussis) that use only a small part of the virus such as a protein, and vaccines which use nucleic acid that inject a small number of viral genes, so as to make the body immune to the virus (Decario, Citation2020). ML is used to speed up the growth of nucleic acids and subunit vaccine types. The structure of protein composition has to be analyzed and researchers develop new
drugs that can work for different protein structures. However, finding this unique 3D structure takes a lot of time. Evaluating genetic sequences and protein structure can be simplified with the help of ML and DL systems. AlphaFold was introduced by Google DeepMind (HospiMedica, Citation2020b; Institute for Protein Design, Citation2020), an advanced ML application that predicts the function of 3D proteins using their genomic sequences. The system can be used for COVID-19 as well. It also helped the scientific community to understand the virus by publishing a protein prediction for all the proteins that are related to SARS-CoV-2. The first 3D atomic map to understand the spike protein component of the virus was developed by the researchers at the University of Texas. AlphaFold has provided accurate predictions for the protein spike structure. 3D atom models for the SARS-CoV-2 protein scale that were simulated (Rees, Citation2020) was used by the researchers of the University of Washington. New proteins were created to emulate Coronavirus. These proteins would embed with the healthy cells to prevent viral attacks. AI was combined with cloud computing to prevent the spike protein from binding to healthy human cells. A vaccine could be produced using this technique (TABIP, Citation2020). The researchers of Flinders University studied the structure of Coronavirus and then designed a vaccine using the data collected (Flinders University, Citation2020). It was called Covax-19 as shown in .
Figure 4. Covax-19™ is an Australian-designed COVID-19 vaccine modelled by AI-based technologies (Flinders University, Citation2020)
The team used AI and cloud technologies to speed up the production of COVID-19 vaccines in (Flinders University, Citation2020; Herst et al., Citation2020; Institute for Protein Design, Citation2020). Computer- based models of S protein along with its human receptor, the enzyme converting angiotensin 2 (ACE2) was used to understand how the COVID-19 virus was harming healthy human cells. Herst et al. (Ong et al., Citation2020), used MSA (Multiple Sequence Alignment) algorithm for the detected GenBank’s SARS-CoV-2 protein sequence to model the nucleocapsid phosphoprotein sequence in the future peptide sequencing. A peptide-based vaccine was used to treat another epidemic which had happened in West Africa (Ebola, 2013–2016). Ong et al. (CitationDeoras) used reverse vaccinology (RV) and ML to test various COVID-19 vaccines. RV was used to analyse bioinformatics pathogen genomes. Biological signals were forecasted using models called Vaxign and Vaxign-ML. Algorithms like vector support, RF, proximity neighbour, and overgrowth (XGB) strategies were used by the above models. Researchers from MIT (Rahman et al., Citation2020) have developed an AI-based method that chooses peptides that give large vaccine numbers. The design software is named “OptiVax”. It designs new peptide vaccines by learning from the existing vaccines to improve composition. Immunoinformatic methods were used to beat the virus. Rahman et al. (Sarkar et al., Citation2020), produced an antipeptid vaccine for COVID-19 which consisted of envelop, membrane and spike protein. A predictive system called Ellipro antibody epitope was used to predict B-specific epitopes in spike protein. To visualize and forecast a protein sequence, Ellipro used several models of ML. The epitope-based vaccine model of COVID-19 was also explored by Sarkar et al. (Prachar et al., Citation2020). SVM technique was applied to predict the toxicity of choses epitopes. 174 epitopes of COVID-19 were forecasted by Prachar et al. (Xue et al., Citation2018). IEDB (Immune Epitope Database) was used to collect data and PSSM (Position-Specific Scanning Matrix) and ANN was used for prediction.
6.2. Drug development using ml for COVID-19
AI systems can be used to battle infectious diseases like COVID-19, by easily classifying and predicting appropriate drugs. Drug development is a very costly, lengthy and dangerous phase. The success rate is only 2.01% and it takes a minimum of ten to 15 years to develop a completely new drug according to Eastern Research Group (ERG) (Mohanty et al., Citation2020). Drug repurposing uses an experimental strategy to reuse pre-approved, discontinued and shelved medications. Normally, drug development involves 5 steps: Drug discovery and development, pre-clinical research, clinical research, FDA (Food and Drug Association) drug review and FDA drug aftermarket safety control. However, drug repurposing involves only 4 steps (Beck et al., Citation2020): Compound identification, Drug clinical research and FDA drug after-market safety control and development. In one research, AI is used for drug discovery at the very molecular level. Beck et al. (Pahikkala et al., Citation2015), recommended a DL-based drug-target interaction model, named Molecule Transformer Drug Target Interaction (MT-DTI). This model can be used to predict drugs for COVID-19. The MT-DTI model used amino-acid sequences and SMILES strings to classify target protein. The inhibitory potency of the chemical compound atazanavir (a drug to treat and prevent HIV) was the best according to the study. Remdesivir also produced positive results. Two similarity-based models KronRLS (He et al., Citation2017) and SimBoost (Öztürk et al., Citation2018) that use ML for drug discovery have been proposed. However, there are a couple of disadvantages. The representation of features is reduced drastically which can result in faulty products. Also, estimation of matrix of similarity limits the number of molecules. A DTI model which used DL, DeepDTA (K. Huang et al., Citation2021), was introduced to improve the above models. It used a CNN based model that waives requirements related to feature engineering. From protein sequences and raw molecules, useful features are automatically detected by the model. Sim-Boost and KronRLS both used this model. Feature representation from SMILES strings and raw protein sequences were trained using a CNN model, and named it DeepDTA. Proteins and ligands pair-wise similarities were processed using Smith-Waterman and Pubchem similarity algorithms respectively. Three alternative combinations were trained to develop a more advanced DeepDTA model. These included training compound representations alone, training protein sequence representation alone and the third model used both protein and compound representation. The combined model was used in many COVID-19 drug repurposing researches (Anwar et al., Citation2020; Pahikkala et al., Citation2015; Zeng et al., Citation2019). DeepDR (Anwar et al., Citation2020), a network-based DL model was used for silico drug repurposing. DeepDR uses heterogenous networks to understand different high stage features using deep auto encoder. The AUC obtained by using the model was 90.08% surpassing all other ML and DL methods. DeepPurpose (Kojima et al., Citation2020), kGCN (Ramsundar et al., Citation2019), DeepChem (Y. Shi et al., Citation2020), and D3Targets-2019-nCoV (Bung et al., Citation2021) were the other models which used ML for drug repurposing. Bung et al. (Tang et al., Citation2020), used deep learning technology to develop a modern chemical framework called SARS-CoV-2 3 CL pro. A RL based RRN method was established for protease inhibitor molecules. From CheMBL database, 2515 SMILES protease inhibitors molecules were trained. The SMILES sequence was used as location, symbol and time series. The 3CLpro structure was used to embed these molecules with a minimum force to select the participants in the development of anti-SARS-CoV-2 based on visualization. Tang et al. (Moskal et al., Citation2020), pursued the development of anti-COVID-19 drugs using 3CLpro with a structure that was similar to SARS-CoV. Leading SARS-CoV-2 3CLpro compounds were developed using Q-learning network called ADQN-FBDD. 284 molecules of SARS-CoV-2 3CLpro inhibitors were collected and classified using an optimized BRICS technique in order to understand the SARS-CoV-2 3CLpro targeted library. The ADQN-FBDD model trained each target and classified the corresponding molecules. 47 compounds were identified, that could be used as anti-SARS-CoV2-drugs with the structure-based optimization policy. shows ML and DL methods for drug development of COVID-19.
Table 8. Drug development of COVID-19 using ML
7. Managing and controlling the pandemic
Pandemic control deals with curbing the spread of this viral infection to the maximum extent. AI methods can be efficiently used in curbing the spread of the deadly virus. ML can be used to reduce the infection rate in many ways which are discussed below.
7.1. Contact tracing
Pandey et al., (Hashem et al., Citation2020), developed an AI application called “Washkaro” that can track people who spread misinformation about COVID-19. The interactions of people are automatically recorded and all wrong information is monitored using a self-assessment tool. Prevention and detection of the spread of the pandemic were proposed in (Lee et al., Citation2020). This machine learning model was used to forecast pandemics and epidemics which might occur further.
7.2. Identification of COVID-19 cases
Continuous inspection and monitoring are required to control the spread of this virus. In (Simsek & Kantarci, Citation2020), an agent which uses a call-based model is used to actively monitor and identify the people in South Korea and Japan. For optimal mobilization, mobile assessment agents were deployed in (Mashamba-Thompson & Crayton, Citation2020). In (Rao & Vazquez, Citation2020), a combination of blockchain and AI was used as a tracking system for COVID-19. A phone-based survey was used to identify cases in (Muthya et al., Citation2020). Infections among several communities can be measured using particular indicators according to this paper. In (Pirouz et al., Citation2020), symptoms like conjunctivitis, diarrhoea, nausea etc. were used to monitor different groups of the population.
7.3. COVID-19 testing
Testing is also very important in the battle against COVID-19. In (B. Wang et al., Citation2020), ML was used to understand the correlation between the swab tests and the positive cases. The authors state that a correlation between swab tests and confirmed cases, placid cases, fatal cases and death rates definitely exists. ML along with graph theory is used to reduce the infection rate using an optimization problem called minimum weight vertex problem (Mowery et al., Citation2020). In (Sangiorgio & Parisi, Citation2020), COVID-19 infection is tested using lateral flow assays (LFA) along with ML. The authors reported that the pairing of LFA’s obtained a better classification.
7.4. Risk assesment
In (Yan et al., Citation2020), ANN-based algorithms were used for many urban districts to perform risk assessments. Community based risk assessment was proposed in (Uddin et al., Citation2020). Based on the state, country and city, a specific risk was measured.
7.5. Social distancing
One of the most effective methods in curbing the virus is social distancing. A CNN based algorithm (Yang et al., Citation2020) was proposed to monitor the people in public places. The algorithm checked whether the people had symptoms like cough and fever. In (Punn et al., Citation2020), people who do not follow social distancing were caught using a machine vision algorithm. A surveillance video-monitored social distancing norm with the help of DL (Khandelwal et al., Citation2020). In (Qin & Li, Citation2020), AI along with machine vision was used to detect social distancing violations among workers. Class projective geometry and deep learning techniques were combined. Wearing facemasks reduces the chances of getting infected by this virus. In (Sesagiri Raamkumar et al., Citation2020), people were checked for face masks using image processing and machine learning. In (Johnstone, Citation2020), deep learning models were used to classify context on Facebook. The model was studied to understand the public perception towards face masks and social distancing.
7.6. Helping various organisations
In (Nawaz et al., Citation2020), ML was used to help various charities to organize funds during the pandemic. Library services were optimized along with resource allocation (Bandyopadhyay & DUTTA, Citation2020). A neural network model is presented (T. Chen et al., Citation2020) to detect fraud transactions. The education system has been completely changed during this pandemic. New platforms have emerged to help students continue their education. Education satisfaction was modelled using ANN (Li et al., Citation2020).
7.7. Pyschological effect
A lot of people have experienced unemployment, helplessness, hopelessness and social isolation during the pandemic. Many of them have had little or no psychological support. People’s mental health during COVID-19 is explained in (Hossain & McKyerand P. Ma, Citation2020). ML was used to manage the psychological effects in (Khattar et al., Citation2020). In (Prakash Jha et al., Citation2020), ML was used to understand the mental health of students of India. In (Ćosić et al., Citation2020), ML was used to determine various factors which impact mental health of people during the lockdown period. Bayesian Network was used to understand the key factors. In (Cosic et al., Citation2020), high distress among people was calculated which directly led to chronic mental health disorder. Mental health during pandemic was also studied in (Ehrlich & Ghimire, Citation2020).
7.8. Other impacts
The entire sporting industry has changed during the pandemic. Lack of fans, bio-bubbles, social distancing, etc. has impacted the performance of players. ML was used to study the same in (Rahman et al., Citation2020). A clustering framework was used to study the economic impact during lockdown in (Ghamizi et al., Citation2020). Economic crisis of various countries was studied using data driven models in (Tarrataca et al., Citation2021). Epidemiological forecasting was also made with the aid of a deep learning method. A natural regression model was proposed (Allam & Jones, Citation2020) which predicted the effect of COVID-19 in Brazil. The idea of developing smart cities to tackle the effects of the pandemic have also been discussed. In (Minetto et al., Citation2021), ML methods are used to understand various outbreaks and how smart cities can be built to increase data sharing during the pandemic. Human activities have changed drastically during COVID-19. To understand this change in pattern, a deep learning algorithm was used (D. Wang et al., Citation2020). CNN is combined with strategic location sampling. A DNN was proposed in (Asheghi et al., Citation2020) to understand various transportation trends during the pandemic.
8. Sensitivity analysis for developing ml models
For predictive modelling, performance normally improves with the dataset quantity. This is dependent on the datasets and the model used, but it frequently means that using more data might result in greater performance and that discoveries made using smaller datasets to predict model performance often translates to using bigger datasets. The issue is that the relationship is unknown for every given dataset and model, and it might not exist for some datasets and models. Furthermore, if a co-relation exists, there may be a point or points of diminishing returns where adding additional data does not increase model performance or where datasets are too tiny to adequately capture a model’s potential at a wider scale. To address these difficulties, sensitivity analysis can be used to quantify the relationship between dataset size and model performance (May Tzuc et al., Citation2019). We may then analyse the findings of the research and decide how much data is sufficient and how small a dataset should be in order to accurately estimate performance on larger datasets. One method to approach this challenge is to conduct a sensitivity analysis and see how the performance of your model on your dataset changes as you add or subtract data May Tzuc et al. Citation2019). This could entail comparing the same model with different dataset sizes to see if there is a link between dataset size and performance or if there is a point of diminishing returns. In most cases, especially for nonlinear models, there is a high correlation between training dataset size and model performance. As the dataset size grows, the model’s performance improves to a point and the predicted variance of the model decreases. This relationship between your model and dataset might be useful for a variety of reasons, including:
Evaluation of models.
Finding a more suitable model.
Making the decision to collect more information.
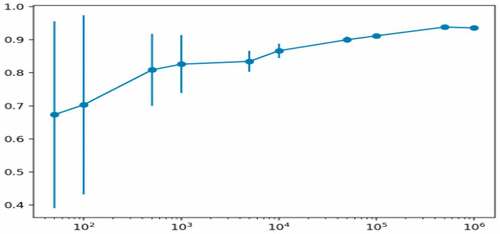
We can quickly test a large number of model configurations on a smaller sample of the dataset and be confident that the results will generalize in a predictable manner to a larger training dataset. This may allow you to evaluate many more models and configurations than you would otherwise be able to given the time constraints, allowing you to find a model that performs better overall. We can also extrapolate and estimate the model’s expected performance to much bigger datasets, and determine whether it’s worth the effort or price to collect more training data. These results could be used to test additional model configurations and even different design types. The risk is that the different models will perform differently with more or less data, therefore it’s a good idea to run the sensitivity analysis again with a different model to make sure the association persists. Alternatively, you may run the study again using a variety of other model types. compares the model performances with different dataset sizes.
Figure 5. Line plot with error bars of dataset size vs. model performance Brownlee, Citationn.d.)
When the probability estimates of a data point belonging to a class is critical, the model can be calibrated. Calibration is the comparing of a system’s actual output with its expected output Ranjan, Citationn.d.). In this process, we strive to enhance our model so that the probability predicted has a distribution and behavior that is similar to the probability distribution and behavior observed in training data. To get the best results out of AI, it is very important to perform sensitive analysis and calibration for the design models.
9. Challenges and future directions
This section elaborates the various challenges while using ML to fight COVID-19. Additionally, we give clear directions for future research.
9.1. Challenges
A lot of ML applications in COVID-19 research face many challenges, such as noisy data, scarcity and unavailability of large training data, rumors, limited awareness in interdisciplinary studies (computer science and medicine), security and data privacy issues and many more. The following have been discussed here.
Regulation—As COVID-19 spreads and the number of confirmed cases grow, several measures, such as lockdown and social distancing, have been proposed to contain it. During a pandemic, authorities have a critical role in developing legislation and policies that can encourage citizens, researchers, scientists, business owners, medical centres, technology behemoths, and significant enterprises to participate in COVID-19 prevention.
Unavailability of large datasets—Many AI-based DL approaches rely on large-scale training data, such as medical imaging and other applications. However, due to the rapid growth of COVID-19, there are insufficient datasets accessible for AI. In practice, evaluating training samples takes time and may necessitate the use of qualified medical specialists.
Noisy datasets and rumors—The difficulties arise from relying on the internet with no significant adjustments. Thus, huge quantities of audio material and misleading reports regarding COVID-19 have been reported on various online sites. However, AI-based ML and DL algorithms appear to be slow when judging and filtering audio and erroneous data. Furthermore, when noisy data is used, the findings of AI-based ML and DL algorithms become skewed. This problem reduces the usefulness and performance of AI-based approaches, particularly in pandemic forecasting and spread assessment.
Lack of combined knowledge in medicine and computer fields—Most AI-based ML and DL researchers have a computer science background, but substantial specialization in medical imaging, bioinformatics, virology and many other relevant domains are also necessary for the COVID-19 fight. To deal with COVID-19, it is therefore necessary to organize the participation of experts from diverse sectors and to include data from multiple investigations.
Data Privacy—In the age of big data and AI, the cost of obtaining personal data is incredibly low. In response to public health challenges such as COVID-19, many governments intend to collect a variety of personal information, including ID numbers, contact numbers, personal data, and patient history. A concern that should be addressed is how to efficiently protect the privacy and human rights during AI-based research and analysis.
Unstructured Data (Numerical, text, image)—It might be difficult to work with confusing and inaccurate information in text descriptions. A large amount of information from various sources may be false. Furthermore, excess data makes it impossible to extract meaningful information.
9.2. Future directions
ML systems can be improved for the future in the war against the deadly COVID-19 in the following ways.
Non-contact virus detection—During COVID-19, the use of automated image classification in X-ray and CT imaging will drastically reduce the possibility of disease transmission from victims to radiologists.
Automated diagnosis and consultation—It is possible to create remote video diagnostic programs and robot systems using a combination of AI and Natural Language Processing (NLP) approaches to deliver COVID-19 patient visits and first group diagnoses.
Biological research—In the context of biological research, AI-based ML and DL systems can be used to discover protein composition and viral components using accurate biomedical expertise analysis, such as major protein structures, viral trajectories and genetic sequences.
Drug and Vaccine development—AI-based ML and DL algorithms may be used to not only discover potential medications and vaccines, but also to simulate drug-protein and vaccine-receptor interactions, predicting future drug and vaccine reactions for individuals with varied COVID-19 symptoms.
Fake information screening—To give genuine, factual and scientific information on the COVID-19 outbreak, AI-based ML and DL algorithms can be used to limit and erase misleading news and audio data on internet forums.
Impact assessment and evaluation—Different types of simulations may use AI-based ML and DL systems to analyse the influence of various social control techniques on disease transmission. They can then be used to evaluate trustworthy and scientific techniques for the prevention and management of the disease.
Contact Tracing—By establishing social networks and knowledge graphs, an AI-based ML and DL system can monitor and track the characteristics of people living around COVID-19 patients, effectively forecasting and tracking the disease’s potential spread.
SMART robots—Intelligent robots are expected to be deployed in programs such as public cleanliness, product delivery and medical treatment that do not require human resources. This will halt the transmission of the COVID-19 virus.
Future work with descriptive ML and DL techniques—The efficiency of deep learning techniques and the graphical properties that distinguish COVID-19 from other types of pneumonia must be defined. This will assist radiologists and physicians in becoming familiar with the virus and accurately analyzing probable coronavirus X-ray and CT images.
10. Conclusion
The COVID-19 outbreak has affected the safety and security of people all around the world. Technology continues to grow with great success, especially in the field of ML and DL. ML has contributed largely in supporting people in the fight against COVID-19. Promising data-driven solutions continue to help humanity to handle COVID-19. A brief overview of ML algorithms was discussed in the beginning. Various supervised, unsupervised and reinforcement algorithms were explained in brief and the use of them in battling COVID-19 was discussed as well Various datasets were also explored. These included CT images, XSR images, Twitter data, patient demographics, genetic sequences and many more. In the next section, ML methods to diagnose COVID-19 using CT-Scan, XSR images, sound analysis and routine blood tests were discussed in detail. All the above methods were compared to find out the advantages and disadvantages of those methods. The severity of COVID-19 progression using ML was also looked into Drug and vaccine development for COVID-19 using ML was also explored. Controlling and managing this pandemic using various ML applications were described later. This systematic review provides a detailed overview of existing state-of-the-art research methods and technologies for researchers and the broader health community. The paper concluded with challenges and future directions for subsequent researches.
List of abbreviations
Disclosure statement
The authors declare no competing interest.
Additional information
Funding
Notes on contributors

Srikanth Prabhu
Krishnaraj Chadaga received MTech degree in Computer Science and Engineering from Manipal Institute of Technology respectively. He is currently pursuing his Ph.D. degree in Manipal Institute of Technology.
Dr. Srikanth Prabhu received his Ph.D. degree in Computer Science and Engineering from Indian Institute of Technology, Kharagpur. He is currently working as a Senior Associate Professor in the Department of Computer Science and Engineering, Manipal Institute of Technology.
Dr. Vivekananda Bhat K received the Ph.D. degree in computer science and engineering from IIT Kharagpur, He is currently an Associate Professor with the Department of Computer Science and Engineering, Manipal Institute of Technology.
Dr. Niranjana S., PhD, is currently working as Associate Professor-Senior Scale in the Department of Biomedical Engineering, Manipal Institute of Technology.
Dr Shashikiran Umakanth is the Medical Superintendent of Dr TMA Pai Hospital, Udupi, India. He is also a Professor and HOD, Department of Medicine, Manipal Academy of Higher Education. He has been a nodal head during the COVID-19 pandemic.
References
- A. K, M. I. Y., & Routray, A. (2019). Automatic measurement of speech breathing rate. 2019 27th European Signal Processing Conference (EUSIPCO), 1–41, https://doi.org/10.23919/EUSIPCO.2019.8902730.
- Wikipedia database downloaod. 2020. [Online]. Retrieved https://en.wikipedia.org/wiki/Wikipedia:Database_download
- Abbaszadeh Shahri, A., Asheghi, R., & Khorsand Zak, M. (2021). A hybridized intelligence model to improve the predictability level of strength index parameters of rocks. Neural Computing and Applications, 33(8), 3841–3854. https://doi.org/10.1007/s00521-020-05223-9
- Abbaszadeh Shahri, A., Kheiri, A., & Hamzeh, A. (2021). Subsurface topographic modeling using geospatial and data driven algorithm. ISPRS International Journal of Geo-Information, 10(5), 341. https://doi.org/10.3390/ijgi10050341
- Abbaszadeh Shahri, A., & Maghsoudi Moud, F. (2020). Liquefaction potential analysis using hybrid multi-objective intelligence model. Environmental Earth Sciences, 79(19), 1–17. https://doi.org/10.1007/s12665-020-09173-2
- Abbaszadeh Shahri, A., & Maghsoudi Moud, F. (2021). Landslide susceptibility mapping using hybridized block modular intelligence model. Bulletin of Engineering Geology and the Environment, 80(1), 267–284. https://doi.org/10.1007/s10064-020-01922-8
- Abderrahim, E., Xavier, D., Zakaria, L., & Olivier, L. (2014). Nonlocal infinity Laplacian equation on graphs with applications in image processing and machine learning. Mathematics and Computers in Simulation, 102, 153–163. https://doi.org/10.1016/j.matcom.2014.01.007
- Ahmad, A., Garhwal, S., Ray, S. K., Kumar, G., Malebary, S. J., & Barukab, O. M. (2020). The number of confirmed cases of covid-19 by using machine learning: methods and challenges. Arch. Comput. Methods Eng, 0123456789. https://doi.org/10.1007/s11831-020-09472-8
- Ahuja, A. S., Reddy, V. P., & Marques, O. (2020). Artificial intelligence and COVID-19: A multidisciplinary approach. Integrative Medicine Research, 9(3), 100434. https://doi.org/10.1016/j.imr.2020.100434
- Al Hossain, F., Lover, A. A., Corey, G. A., Reich, N. G., & Rahman, T. (2020). FluSense: A contactless syndromic surveillance platform for influenza-like illness in hospital waiting areas. Proc. ACM Interactive, Mobile, Wearable Ubiquitous Technol, 4(1), 1–28. https://doi.org/10.1145/3381014
- Alafif, T., Tehame, A. M., Bajaba, S., Barnawi, A., & Zia, S. (2021). Machine and deep learning towards covid-19 diagnosis and treatment: Survey, challenges, and future directions. International Journal of Environmental Research and Public Health, 18(3), 1–24. https://doi.org/10.3390/ijerph18031117
- Allam, Z., & Jones, D. S. (2020). On the coronavirus (COVID-19) outbreak and the smart city network: universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management. Healthcare, 8(1), 1. https://doi.org/10.3390/healthcare8010046
- Allen-Institute. (March. 2020). CORD-19 research challenge. . [On- line]. Retrieved https://www.kaggle.com/allen-institute-for-ai/CORD-19-research-challeng%e
- Almeshal, M., Almazrouee, A. I., Alenizi, M. R., & Alhajeri, S. N. (2020). Forecasting the spread of COVID-19 in Kuwait using compartmental and logistic regression models. Applied Sciences, 10(10), 3402. https://doi.org/10.3390/app10103402
- Analytics, H. I. (2020). Deep learning models can detect COVID-19 in Chest CT Scans. Retrieved https://healthitanalytics.com/news/deep-learning-models-can-detect-covid-19-in-chest-ct-scans
- Anter, A. M., Oliva, D., Thakare, A., & Zhang, Z. (2021). AFCM-LSMA: New intelligent model based on Lévy slime mould algorithm and adaptive fuzzy C-means for identification of COVID-19 infection from chest X-ray images. Advanced Engineering Informatics, 49, 101317. https://doi.org/10.1016/j.aei.2021.101317
- Anwar, M. U., et al. (2020). Combined deep learning and molecular docking simulations approach identifies potentially effective FDA approved drugs for repurposing against SARS-CoV-2. ChemRxiv, 12227363.v1. https://doi.org/10.26434/chemrxiv.
- Apostolopoulos, I. D., Aznaouridis, S. I., & Tzani, M. A. (2020). Extracting possibly representative COVID-19 biomarkers from X-ray images with deep learning approach and image data related to pulmonary diseases. Journal of Medical and Biological Engineering, 40(3), 462–469. https://doi.org/10.1007/s40846-020-00529-4
- Apostolopoulos, I. D., & Mpesiana, T. A. (2020). Covid-19: Automatic detection from X-ray images utilizing transfer learning with convolutional neural networks. Physical and Engineering Sciences in Medicine, 43(2), 635–640. https://doi.org/10.1007/s13246-020-00865-4
- Aramaki, E., Maskawa, S., & Morita, M. (2011). Twitter catches the flu: Detect-ing influenza epidemics using Twitter. In Proc. conf. empirical methods natural lang. process (pp. 1568–1576). Association for Computational Linguistics.
- Arpaci, I., Huang, S., Al-Emran, M., Al-Kabi, M. N., & Peng, M. Predicting the COVID-19 infection with fourteen clinical features using machine learning classification algorithms. (2019, December). Multimed. Tools Appl, 11943–11957. 2021, https://doi.org/10.1007/s11042-020-10340-7.
- Asheghi, R., Hosseini, S. A., Saneie, M., & Shahri, A. A. (2020). Updating the neural network sediment load models using different sensitivity analysis methods: A regional application. Journal of Hydroinformatics, 22(3), 562–577. https://doi.org/10.2166/hydro.2020.098
- Assery, N., Xiaohong, Y., Almalki, S., Kaushik, R., & Xiuli, Q. (2019). Comparing learning-based methods for identifying disaster-related tweets. 2019 18th IEEE international conference on machine learning and applications (ICMLA).
- B, C. et al. Coronasurveys: Monitoring COVID-19 incidence via open polls. Retrieved April 23, 2021. http://coronasurveys.com
- Bagad, P., et al. (2020). Cough against COVID: Evidence of COVID-19 signature in cough sounds. arXiv. (Ml).
- Bai, X., Fang, C., Zhou, Y., Bai, S., Liu, Z., Xia, L., Chen, Q., Xu, Y., Xia, T., Gong, S., Xie, X., Song, D., Du, R., Zhou, C., Chen, C., Nie, D., Qin, L., & Chen, W. (2020). Predicting COVID-19 malignant progression with AI techniques. SSRN Electronic Journal.
- Bandyopadhyay, S., & DUTTA, S. (2020, June). Detection of fraud transactions using recurrent neural network during COVID-19. Journal of Advanced Research in Medical Science & Technology, 07(3), 16–21. https://doi.org/10.20944/PREPRINTS202006.0368.V1
- Banerjee, A., et al. (2020). Use of machine learning and artificial intelligence to predict SARS-CoV-2 infection from full blood counts in a population. International Immunopharmacology, 86, 106705. https://doi.org/10.1016/j.intimp.2020.106705
- Barragán, D., & Manero, J. (2020). How big data and artificial intelligence can help against COVID-19. IE Bus. Sch, 4–11. Available, https://www.ie.edu/business-school/news-and-events/whats-going-on/big-data-artificial-intelligence-can-help-covid-19/
- Basu, S., & Mitra, S. (2020). Deep learning for screening COVID-19 using Chest X-ray Images. In arXiv (pp. 10507). arXiv:2004.
- COVID Chest-Xray Dataset. (March. 2020). Retrieved https://github.com/ieee8023/covid-chestxray-dataset
- Beck, B. R., Shin, B., Choi, Y., Park, S., & Kang, K. (2020). Predicting commercially available antiviral drugs that may act on the novel coronavirus (SARS-CoV-2) through a drug-target interaction deep learning model. Computational and Structural Biotechnology Journal, 18, 784–790. https://doi.org/10.1016/j.csbj.2020.03.025
- Bhandari, S., et al. (2020). Logistic regression analysis to predict mortality risk in COVID-19 patients from routine hematologic parameters. Ibnosina J. Med. Biomed. Sci, 12(2), 123.
- Brinati, D., Campagner, A., Ferrari, D., Locatelli, M., Banfi, G., & Cabitza, F. (2020). Detection of COVID-19 infection from routine blood exams with machine learning: A feasibility study. medRxiv. https://doi.org/10.1101/2020.04.22.20075143
- Brown, C., Chauhan, J., Grammenos, A., Han, J., Hasthanasombat, A., Spathis, D., Xia, T., Cicuta, P., & Mascolo, C. (2020). Exploring automatic diagnosis of COVID-19 from crowdsourced respiratory sound data. Proceedings of the 26th ACM SIGKDD international conference on knowledge discovery & data mining.
- Browning, L., Colling, R., Rakha, E., Rajpoot, N., Rittscher, J., James, J. A., Salto-Tellez, M., Snead, D. R. J., & Verrill, C. (2020). Digital pathology and artificial intelligence will be key to supporting clinical and academic cellular pathology through COVID-19 and future crises: The PathLAKE consortium perspective. Journal of Clinical Pathology.
- Brownlee, J. (n.d.) Sensitivity analysis of dataset size vs. Model performance. Retrieved https://machinelearningmastery.com/sensitivity-analysis-of-dataset-size-vs-model-performance
- Bullock, J., Luccioni, A., Pham, K. H., Lam, C. S. N., & Luengo-Oroz, M. (2020). Mapping the landscape of artificial intelligence applications against COVID-19. Journal of Artificial Intelligence Research, 69, 807–845. https://doi.org/10.1613/JAIR.1.12162
- Bung, N., Krishnan, S. R., Bulusu, G., & Roy, A. (2021). De novo design of new chemical entities for SARS-CoV-2 using artificial intelligence. Future Medicinal Chemistry, 13(6), 575–585. https://doi.org/10.4155/fmc-2020-0262
- Butt, C., Gill, J., Chun, D., & Babu, B. A. (2020, April). Deep learning system to screen coronavirus disease 2019 pneumonia. Appl. Intell, 1–7. https://doi.org/10.1007/s10489-020-01714-3
- Cadotte, M. (March. 2020). Early evidence that COVID-19 government policies reduce urban air pollution. [Online]. Retrieved eartharxiv.org/nhgj3
- Cascella, M., Rajnik, M., Cuomo, A., Dulebohn, S. C., & Di Napoli, R. (2020). Features, evaluation, and treatment of coronavirus (COVID-19). In references - scientific research publishing.
- Let’s beat covid-19 - take the survey to help one million doctors. Retrieved https://letsbeatcovid.net
- Chamola, V., Hassija, V., Gupta, S., Goyal, A., Guizani, M., & Sikdar, B. Disaster and pandemic management using machine learning: a survey. IEEE Internet of Things Journal. https://doi.org/10.1109/JIOT.2020.3044966
- Chamola, V., Hassija, V., Gupta, V., & Guizani, M. (2020). A comprehensive review of the COVID-19 pandemic and the role of iot, drones, ai, blockchain, and 5g in managing its impact. IEEE Access, 8, 90225–90265. https://doi.org/10.1109/ACCESS.2020.2992341
- Chen, E., Lerman, K., & Ferrara, E. (March, 2020). COVID-19: the first public coronavirus twitter dataset: semantic scholar. Retrieved April 23, 2021. https://www.semanticscholar.org/paper/COVID-19:-The-First-Public-Coronavirus-Twitter-Chen-Lerman/f03d2034bce849dcc4c4af5b5cbba0e1d2826b94. [Accessed].
- Chen, J., et al. (2020). Deep learning-based model for detecting 2019 novel coronavirus pneumonia on high-resolution computed tomography. Sci. Rep, 10(1), 1–11. https://doi.org/10.1038/s41598-020-76282-0
- Chen, J., Li, K., Zhang, Z., Li, K., & Yu, P. S. (2020b). arXiv:2007.02202. A survey on applications of artificial intelligence in fighting against covid-19.
- Chen, N. C., Drouhard, M., Kocielnik, R., Suh, J., & Aragon, C. R. (2018). Using machine learning to support qualitative coding in social science: Shifting the focus to ambiguity. ACM Transactions on Interactive Intelligent Systems, 8(2), 1–20. https://doi.org/10.1145/3185515
- Chen, Q., Allot, A., & Lu, Z. (2020). Keep up with the latest coronavirus research. Nature, 579(7798), 193. https://doi.org/10.1038/d41586-020-00694-1
- Chen, T., Peng, L., Yin, X., Rong, J., Yang, J., & Cong, G. (2020). Analysis of user satisfaction with online education platforms in China during the COVID-19 pandemic. Healthcare, 8(3), 3. https://doi.org/10.3390/healthcare8030200
- Chen, Y., & Liu, Y. (2021). Which risk factors matter more for psychological distress during the COVID-19 pandemic? an application approach of gradient boosting decision trees. International Journal of Environmental Research and Public Health, 18(11), 5879. https://doi.org/10.3390/ijerph18115879
- Chhikara, P., Tekchandani, R., Kumar, N., Chamola, V., & Guizani, M. (2021). DCNN-GA: A deep neural net architecture for navigation of UAV in indoor environment. IEEE Internet of Things Journal, 8(6), 4448–4460. https://doi.org/10.1109/JIOT.2020.3027095
- CHIME. (2020). COVID-19 hospital impact model for epidemics. [Online]. Retrieved https://github.com/CodeForPhilly/chime
- Cho, S.-B. (2016). Exploiting machine learning techniques for location recognition and prediction with smartphone logs. Neurocomputing, 176, 98–106. https://doi.org/10.1016/j.neucom.2015.02.079
- Chowdhury, M. E. H., et al. (2020). Can AI help in screening viral and COVID-19 pneumonia? IEEE Access, 8, 132665–132676. https://doi.org/10.1109/ACCESS.2020.3010287
- Cohen, J. P., et al. (2020, July). Predicting COVID-19 pneumonia severity on Chest X-ray With Deep Learning. Cureus, 12 (7), e9448–e9448. https://doi.org/10.7759/cureus.9448.
- Cohen, J. P., Morrison, P., & Dao, L. (2020). COVID-19 image data collec- tion. arXiv 2003.11597. [Online]. Retrieved https://github.com/ieee8023/covid-chestxray-dataset
- Cosic, K., Popovic, S., Sarlija, M., & Kesedzic, I. (2020). Impact of human disasters and Covid-19 pandemic on mental health: potential of digital psychiatry. Psychiatria Danubina, 32(1), 25–31. https://doi.org/10.24869/psyd.2020.25
- Ćosić, K., Popović, S., Šarlija, M., Kesedžić, I., & Jovanovic, T. (2020). Artificial intelligence in prediction of mental health disorders induced by the COVID-19 pandemic among health care workers. Croatian Medical Journal, 61(3), 279–288. https://doi.org/10.3325/cmj.2020.61.279
- COVID-19 Korea Dataset with Patient Routes. (2020). [Online]. Retrieved https://github.com/ThisIsIsaac/Data-Science-for-COVID-19
- Cranfield University. (2020a). Using artificial intelligence to detect COVID-19 in X-rays. Retrieved https://medicalxpress.com/ne-ws/2020-05-artificial-intelligence-covid-x-rays.html
- Cranfield University. (2020b). Using machine learning to detect COVID-19 in X-rays. Retrieved https://tectales.com/ai/using-ai-to-detect-covid-19-in-x-rays.html
- Cranfield University. (2020c). Artificial intelligence spots COVID-19 in Chest X-rays. Retrieved https://pharmaphorum.com/news/artificialintelligence-spots-covid-19-from-chest-x-rays
- Cristobal.baeza. Artificial intelligence to detect COVID-19 in less than a second using x-rays. NEWS BBVA, Retrieved June 10, 2020. https://www.bbva.com/en/artificial-intelligence-to-detect-covid-19-in-less-than-a-second-using-x-rays
- CSSEGISandData. (March. 2020). CSSEGISandData/COVID-19. [Online]. Retrieved https://github.com/CSSEGISandData/COVID-19
- CSSEGISandData. CSSEGISandData/COVID-19. GitHub.-[Online]. Retrieved April 22, 2021. https://github.com/CSSEGISandData/COVID-19
- Culotta, A. (2010). Towards detecting influenza epidemics by analyzing Twit- ter messages. In Proc. 1st workshop social media analytics (pp. 115–122).
- Das, D., Santosh, K. C., & Pal, U. (2020). Truncated inception net: COVID-19 outbreak screening using chest X-rays. Physical and Engineering Sciences in Medicine, 43(3), 915–925. https://doi.org/10.1007/s13246-020-00888-x
- Dasgupta, A. et al. (2020). Epidemiological challenges in pandemic coronavirus disease (covid-19): role of artificial intelligence. Preprints, (May), n/a. https://doi.org/10.20944/preprints202005.0234.v1.
- Cov-clear | Citizen science to help track and clear covid. 2020. [Online]. Retrieved https://cov-clear.com
- de Freitas Barbosa, V. A., et al. (2021, December).Heg.IA: An intelligent system to support diagnosis of Covid-19 based on blood tests. Research on Biomedical Engineering, https://doi.org/10.1007/s42600-020-00112-5.
- de Souza, F. S. H., Hojo-Souza, N. S., dos Santos, E. B., Da Silva, C. M., & Guidoni, D. L. (2020). Predicting the disease outcome in COVID-19 positive patients through Machine Learning: A retrospective cohort study with Brazilian data. In medRxiv January.
- Decario, O. What can COVID-19 teach us about using AI in pandemics?. Retrieved December 1, 2020. https://www.wired.com/story/opinion-ai-can-help-find-scientists-find-a-covid-19-vaccine/ A. Senior, J. Jumper, D. Hassabis, and D. Kohli, “AlphaFold: Using AI for scientific discovery,” Deepmind.
- Deoras, S. How ML is assisting in development of covid-19 vaccines. [Online]. Retrieved https://analyticsindiamag.com/how-ml-is-assisting-in-development-of-covid-19-vaccines
- Deshpande, G., & Schuller, B. (2020). An overview on audio, signal, speech, & language processing for covid-19. In arXiv preprint arXiv:2005.08579.
- Dong, D., et al. (2021). The role of imaging in the detection and management of COVID-19: A Review. IEEE Reviews in Biomedical Engineering, 14, 16–29. https://doi.org/10.1109/RBME.2020.2990959
- ECDC. (2020). European centre for disease prevention and control (ECDC). [Online]. Retrieved: https://ourworldindata.org/coronavirus-source-data
- Echenique, A. (2020). Chest X-ray findings in 636 ambulatory patients with COVID-19 presenting to an urgent care center: A normal chest X-ray is no guarantee contrast reaction view project pancreatic IRE View project. Journal Urgent Care Med, (May), 13–18.
- Data world. 2020. [Online]. Retrieved https://data.world/datasets/mobile
- Ehrlich, J., & Ghimire, S. (2020). COVID-19 countermeasures, major league baseball, and the home field advantage: Simulating the 2020 season using logit regression and a neural network [version 1; peer review: Awaiting peer review]. F1000Research, 9(414), 414. https://doi.org/10.12688/f1000research.23694.1
- Ekum, M., & Ogunsanya, A. (2020). Application of hierarchical polynomial regression models to predict transmission of COVID-19 at global level. Int J Clin Biostat Biom, 6(1), 27.
- Elhoseny, M. (2019). Multi-object detection and tracking (MODT) machine learning model for real-time video surveillance systems. Circuits, Systems, and Signal Processing, 39(2), 611–630. https://doi.org/10.1007/s00034-019-01234-7
- Elsi, Z. R. S., et al. (2020). Utilization of data mining techniques in national food security during the Covid-19 pandemic in Indonesia,”. Journal of Physics. Conference Series, 1594(1), 12007.
- Estrada, M. A. R. (2020). The uses of drones in case of massive epidemics contagious diseases relief humanitarian aid: wuhan-COVID-19 Crisis. SSRN Electronic Journal.
- European Society of Medical Imaging Informatics. Automated diagnosis and quantitative analysis of COVID-19 on Imaging. [Online]. Retrieved https://imagingcovid19ai.eu
- Federico, C., et al. (2020, January). Development, evaluation, and validation of machine learning models for COVID-19 detection based on routine blood tests. medRxiv, 2020.10.02.20205070. https://doi.org/10.1101/2020.10.02.20205070.
- Artificial intelligence in radiology. [Online]. Retrieved: https://mosmed.ai/datasets/covid19_1110
- Flinders University. (2020). Microsoft’s AI for health supports COVID-19 vaccine. Retrieved https://medicalxpress.com/news/2020-08-microsoft-ai-health-covid-vaccine.html
- E. A. Foundation. (June. 2020). Covid19 impact survey. [Online]. Retrieved https://covid19impactsurvey.org
- G. Inc. (March. 2020). COVID-19 community mobility reports. [Online]. Retrieved https://www.google.com/covid19/mobility
- Gale, W. A. (1988). Artificial intelligence and statistics. Addison-Wesley.
- LitCovid - NCBI - NLM – NIH. National Center for Biotechnology Infmation. Retrieved:https://www.ncbi.nlm.nih.gov/research/coronavirus
- Ghamizi, S. et al. (2020). Data-driven simulation and optimization for Covid-19 exit strategies. In Proceedings of the 26th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, pp. 3434–3442, https://doi.org/10.1145/3394486.3412863.
- Ghoshal, B., & Tucker, A. (2020). Estimating uncertainty and interpretability in deep learning for coronavirus (COVID-19) detection. In arXiv (pp. 1–14).
- Ginantra, N. L. W. S. R., Indradewi, I. G. A. D., & Hartono, E. (2020). Machine learning approach for Acute Respiratory Infections (ISPA) prediction: Case study indonesia. Journal of Physics: Conference series, vol. 1469, p. 012044.
- GISAID. (2020). Genomic epidemiology of hCoV-19. [Online]. Retrieved https://www.gisaid.org/epiflu-applications/next-hcov-19-app
- Goodsell, D. S., et al. (2020). RCSB protein data bank: Enabling biomedical research and drug discovery. Protein Science, 29(1), 52–65. https://doi.org/10.1002/pro.3730
- Goodwin, B. D., Jaskolski, C., Zhong, C., & Asmani, H. (2020). Intra-model variability in COVID-19 classification using chest x-ray images. In arXiv.
- Gozes, O., Frid, M., Greenspan, H., & Patrick, D. (2020). arXiv:2003.05037. Rapid AI development cycle for the coronavirus (COVID-19) pandemic : Initial results for automated detection & patient monitoring using deep learning CT image analysis article type : Authors : Summary statement : Key results : List of abbreviati.
- Grimmer, J., Roberts, M. E., & Stewart, B. M. (2021). Machine learning for social science: an agnostic approach. Annual Review of Political Science, 24(1), 395–419. https://doi.org/10.1146/annurev-polisci-053119-015921
- Gutierrez, P. A., Perez-Ortiz, M., Sanchez-Monedero, J., Fernandez-Navarro, F., & Hervas-Martinez, C. (2016). Ordinal regression methods: survey and experimental study. IEEE Transactions on Knowledge and Data Engineering, 28(1), 127–146. https://doi.org/10.1109/TKDE.2015.2457911
- Hall, L. O., Paul, R., Goldgof, D. B., & Goldgof, G. M. (2020). Finding COVID-19 from Chest X-rays using Deep Learning on a Small Dataset. In arXiv (pp. 1–8).
- Hashem, I. A. T., et al. (2020 January). A machine learning solution framework for combatting COVID-19 in smart cities from multiple dimensions. medRxiv, 2020. 05.18.20105577. https://doi.org/10.1101/2020.05.18.20105577.
- He, T., Heidemeyer, M., Ban, F., Cherkasov, A., & Ester, M. (2017). SimBoost: A read-across approach for predicting drug-target binding affinities using gradient boosting machines. Journal of Cheminformatics, 9(1), 1–14. https://doi.org/10.1186/s13321-017-0209-z
- Health EUROPA. (2020). Using artificial intelligence to determine COVID-19 severity. Retrieved https://www.healtheuropa.eu/using-artificial-intelligence-to-determine-covid-19-severity/100501
- Heldt, F. S., et al. (2021). Early risk assessment for COVID-19 patients from emergency department data using machine learning. Scientific Reports, 11(1), 1–13. https://doi.org/10.1038/s41598-021-83784-y
- Hemdan, E. E. D., Shouman, M. A., & Karar, M. E. (2020). COVIDX-net: A framework of deep learning classifiers to diagnose COVID-19 in X-ray images. In arXiv.
- Herst, C. V., et al. (2020, June). An effective CTL peptide vaccine for ebola zaire based on survivors’ CD8+ targeting of a particular nucleocapsid protein epitope with potential implications for COVID-19 vaccine design. Vaccine, 38 (28), 4464–4475. https://doi.org/10.1016/j.vaccine.2020.04.034.
- Hindman, M. (2015, April). Building better models: prediction, replication, and machine learning in the social sciences. The ANNALS of the American Academy of Political and Social Science, 659(1), 48–62. https://doi.org/10.1177/0002716215570279
- Hofmarcher, M., Mayr, A., Rumetshofer, E., Ruch, P., Renz, P., Schimunek, J., Seidl, P., Vall, A., Widrich, M., Hochreiter, S., & Klambauer, G. (2020). Large-scale ligand-based virtual screening for SARS-CoV-2 inhibitors using deep neural networks. SSRN Electronic Journal.
- HospiMedica. (2020a). AI-powered COVID-19 cough analyzer app assesses respiratory health and associated risks. Retrieved https://www.hospimedica.com/covid-19/articles/294784217/ai-powered-covid-19-cough-analyzer-app-assesses-respiratory-health-and-associated-risks.html
- HospiMedica. (2020b). Scientists use cloud-based supercomputing and AI to develop COVID-19 treatments and vaccine models. Retrieved https://www.hospimedica.com/covid19/articles/294784537/scientists-use-cloud-based-supercomputingand-ai-to-develop-covid-19-treatments-and-vaccine-models.html
- Hossain, M. M., & McKyerand P. Ma, E. L. J. Applications of artificial intelligence technologies on mental health research during COVID-19. Retrieved June 23, 2020. osf.io/preprints/socarxiv/w6c9b
- Hu, F., Jiang, J., & Yin, P. (2020). Prediction of potential commercially inhibitors against SARS-CoV-2 by multi-task deep model. In arXiv (pp. 1–8).
- Huang, K., Fu, T., Glass, L. M., Zitnik, M., Xiao, C., & Sun, J. (2021). DeepPurpose: A deep learning library for drug–target interaction prediction. Bioinformatics, 36(22–23), 5545–5547. https://doi.org/10.1093/bioinformatics/btaa1005
- Huang, L., Han, R., Ai, T., Yu, P., Kang, H., Tao, Q., & Xia, L. (2020). Serial quantitative chest ct assessment of covid-19: Deep-learning approach. Radiology: Cardiothoracic Imaging, 2(2), e200075. https://doi.org/10.1148/ryct.2020200075
- Ilyas, M., Rehman, H., & Nait-ali, A. (2020). Detection of Covid-19 From chest x-ray images using artificial intelligence: An early review. In arXiv (pp. 1–8).
- Imran, A., et al. (2020). AI4COVID-19: AI enabled preliminary diagnosis for COVID-19 from cough samples via an app. Informatics in Medicine Unlocked, 20, 100378. https://doi.org/10.1016/j.imu.2020.100378
- Institute for Protein Design. 2020. Rosetta’s Role in Fighting Covid-19. Retrieved https://www.ipd.uw.edu/2020/02/rosettas-role-in-fighting-coronavirus
- Iqbal, M. Z., & Faiz, M. F. I. (2020). Active surveillance for COVID-19 through artificial intelligence using real-time speech-recognition mobile application. 2020 IEEE International Conference on Consumer Electronics - Taiwan (ICCE-Taiwan), pp. 1–2, https://doi.org/10.1109/ICCE-Taiwan49838.2020.9258276.
- Iwendi, C., et al. (2020). COVID-19 patient health prediction using boosted random forest algorithm. Frontiers in Public Health, 8, 357. https://doi.org/10.3389/fpubh.2020.00357
- Jin, C., Chen, W., Cao, Y., Xu, Z., Tan, Z., Zhang, X., Deng, L., Zheng, C., Zhou, J., Shi, H., & Feng, J. (2020). Development and evaluation of an artificial intelligence system for COVID-19 diagnosis. Nature Communications, 11(1). https://doi.org/10.1038/s41467-020-18685-1
- Jin, S., et al. (2020). AI-assisted CT imaging analysis for COVID-19 screening: Building and deploying a medical AI system in four weeks. medRxiv, 1–22. https://doi.org/10.1101/2020.03.19.20039354.
- Johnstone, S. (2020). A viral warning for change. the wuhan coronavirus versus the red cross: better solutions via blockchain and artificial intelligence. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3530756
- Kadioglu, O., Saeed, M., Greten, H. J., & Efferth, T. (2021). Identification of novel compounds against three targets of SARS CoV-2 coronavirus by combined virtual screening and supervised machine learning. Computers in Biology and Medicine, 133(March), 104359. https://doi.org/10.1016/j.compbiomed.2021.104359
- Kan, A. (2017). Machine learning applications in cell image analysis. Immunology & Cell Biology, 95(6), 525–530. https://doi.org/10.1038/icb.2017.16
- Kang, J., Chen, T., Luo, H., Luo, Y., & Du, G. (2021). Machine learning predictive model for severe COVID-19. Infection, Genetics and Evolution, 90(December 2020), 104737. https://doi.org/10.1016/j.meegid.2021.104737
- Kannan, S., Subbaram, K., Ali, S., & Kannan, H. (2020). The role of artificial intelligence and machine learning techniques: Race for COVID-19 vaccine. Archives of Clinical Infectious Diseases, 15(2). https://doi.org/10.5812/archcid.103232
- Kantardzic, M. (2020). Data mining: Concepts, models, methods, and algorithms. Amazon. Available https://www.amazon.com/Data-Mining-Concepts-Methods-Algorithms/dp/0470890452
- Kazancioglu, S., Bastug, A., Ozbay, B. O., Kemirtlek, N., & Bodur, H. (2020). The role of haematological parameters in patients with COVID-19 and influenza virus infection. Epidemiology and Infection, 148, e272. https://doi.org/10.1017/S095026882000271X
- Khandelwal, P., Khandelwal, A., Agarwal, S., Thomas, D., Xavier, N., & Raghuraman, A. (2020). Using computer vision to enhance safety of workforce in manufacturing in a post COVID world. In arXiv (pp. 1–7).
- Khattar, A., Jain, P. R., & Quadri, S. M. K. (2020). Effects of the disastrous pandemic COVID 19 on learning styles, activities and mental health of young indian students - a machine learning approach. 2020 4th International Conference on Intelligent Computing and Control Systems (ICICCS), pp. 1190–1195, https://doi.org/10.1109/ICICCS48265.2020.9120955.
- Kinsa Health. U.S. health weather map. (March. 2020). [Online]. Retrieved https://healthweather.us/?mode=Atypical
- Kojima, R., Ishida, S., Ohta, M., Iwata, H., Honma, T., & Okuno, Y. (2020). KGCN: A graph-based deep learning framework for chemical structures. Journal of Cheminformatics, 12(1), 1–10. https://doi.org/10.1186/s13321-020-00435-6
- Koubaa, A. Understanding the COVID19 outbreak: A comparative data analytics and study. arXiv.org. 29-Mar-2020. Retrieved April 23, 2021. https://arxiv.org/abs/2003.14150
- Kumar, A., Gupta, P., & Srivastava, A. (2020). A review of modern technologies for tackling COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 569–573. https://doi.org/10.1016/j.dsx.2020.05.008. Available
- Kumar, S. N., Ahilan, A., Fred, A. L., & Kumar, H. A. (2021). ROI extraction in CT lung images of COVID-19 using Fast Fuzzy C means clustering. In Biomedical engineering tools for management for patients with COVID-19 (pp. 103–119). Elsevier.
- Lalmuanawma, S., Hussain, J., & Chhakchhuak, L. (2020). Applications of machine learning and artificial intelligence for Covid-19 (SARS-CoV-2) pandemic: A review. Chaos, Solitons, and Fractals, 139, 110059. https://doi.org/10.1016/j.chaos.2020.110059
- Lampos, V., De Bie, T., & Cristianini, N. (2010). Flu detector-tracking epi- demics on Twitter. In Proc. Joint Eur. Conf. Mach. Learn. Knowl. Discovery Databases (pp. 599–602).
- Larson, E. C., Lee, T., Liu, S., Rosenfeld, M., & Patel, S. N. (2011). Accurate and privacy preserving cough sensing using a low-cost microphone. Proceedings of the 13th international conference on Ubiquitous computing - UbiComp 11.
- Latif, S., et al. (2020, August). Leveraging data science to combat COVID-19: A comprehensive review. IEEE Transactions on Artificial Intelligence, 1 (1), 85–103. https://doi.org/10.1109/TAI.2020.3020521.
- Le, D.-N., Parvathy, V. S., Gupta, D., Khanna, A., Rodrigues, J. J. P. C., & Shankar, K. (2021). IoT enabled depthwise separable convolution neural network with deep support vector machine for COVID-19 diagnosis and classification. International Journal of Machine Learning and Cybernetics. https://doi.org/10.1007/s13042-020-01248-7
- Lee, S. W., et al. (2020). CareCall: A call-based active monitoring dialog agent for managing COVID-19 pandemic. arXiv.
- Li, L., et al. (2020, August). Using artificial intelligence to detect COVID-19 and community-acquired pneumonia based on pulmonary ct: evaluation of the diagnostic accuracy. Radiology, 296 (2), E65–E71. https://doi.org/10.1148/radiol.2020200905.
- Li, S., Wang, Y., Xue, J., Zhao, N., & Zhu, T. (2020). The impact of COVID-19 epidemic declaration on psychological consequences: A study on active weibo users. International Journal of Environmental Research and Public Health, 17, 6. https://doi.org/10.3390/ijerph17062032
- Loey, M., Manogaran, G., Taha, M. H. N., & Khalifa, N. E. M. (2021). A hybrid deep transfer learning model with machine learning methods for face mask detection in the era of the COVID-19 pandemic. Measurement, 167, 108288. https://doi.org/10.1016/j.measurement.2020.108288
- Loey, M., Smarandache, F., & Khalifa, N. E. M. (2020). Within the lack of chest COVID-19 X-ray dataset: A novel detection model based on GAN and deep transfer learning. Symmetry, 12(4), 4. https://doi.org/10.3390/sym12040651
- Luengo-Oroz, M., et al. (2020). Artificial intelligence cooperation to support the global response to COVID-19. Nature Machine Intelligence, 2(6), 295–297. https://doi.org/10.1038/s42256-020-0184-3
- Luoh, L. (2013). ZigBee-based intelligent indoor positioning system soft computing. Soft Computing, 18(3), 443–456. https://doi.org/10.1007/s00500-013-1067-x
- Maghdid, H. S., Asaad, A. T., Ghafoor, K. Z., Sadiq, A. S., & Khan, M. K. (2021). Diagnosing COVID-19 pneumonia from x-ray and ct images using deep learning and transfer learning algorithms. In Multimodal Image Exploitation and Learning (Vol. 11734, pp. 117340E). International Society for Optics and Photonics.
- Maia, M., Pimentel, J. S., Pereira, I. S., Gondim, J., Barreto, M. E., & Ara, A. (2020). Convolutional support vector models: Prediction of coronavirus disease using chest x-rays. Inf, 11(12), 1–19. https://doi.org/10.3390/info11120548
- Mangal, A., et al. (2020). CovidAID: COVID-19 detection using chest X-ray. arXiv (pp. 1–10).
- Manning, C. (2016). Understanding human language: Can NLP and deep learning help? In Proc. 39th Int. ACM SIGIR Conf. Res. Develop. Inf. Retrieval (pp. 1).
- Martinez-Alvarez, M., et al. (2020). COVID-19 pandemic in west Africa. The Lancet Global Health, 8(5), e631–e632. https://doi.org/10.1016/S2214-109X(20)30123-6
- Mashamba-Thompson, T. P., & Crayton, E. D. (2020). Blockchain and Artificial Intelligence Technology for Novel Coronavirus Disease 2019 Self-Testing. Diagnostics, 10(4), 4. https://doi.org/10.3390/diagnostics10040198
- May Tzuc, O., Bassam, A., Ricalde, L. J., & Cruz May, E., (2019). Chapter 10 - sensitivity analysis with artificial neural networks for operation of photovoltaic systems, A. Y. Alanis, N. Arana-Daniel, & C. B. T.-A. N. N. F. E.-A. López-Franco Eds, Academic Press. 127–138.
- MegSeg. (March, 2020). COVID-19 CT segmentation dataset. [Online]. Retrieved http://medicalsegmentation.com/covid19
- Mei, X., et al. (2020). Artificial intelligence–enabled rapid diagnosis of patients with COVID-19. Nature Medicine, 26(8), 1224–1228. https://doi.org/10.1038/s41591-020-0931-3
- Mery, D. (2015). Computer Vision for X-Ray Testing (Vol. 10, pp. 978–3). Springer.
- Minaee, S., Kafieh, R., Sonka, M., Yazdani, S., & Jamalipour Soufi, G. (2020, October). Deep-COVID: Predicting COVID-19 from chest X-ray images using deep transfer learning. Medical Image Analysis, 65, 101794. https://doi.org/10.1016/j.media.2020.101794
- Minetto, R., Segundo, M. P., Rotich, G., & Sarkar, S. (2021). Measuring human and economic activity from satellite imagery to support city-scale decision-making during COVID-19 pandemic. IEEE Transactions on Big Data, 7(1), 56–68. https://doi.org/10.1109/TBDATA.2020.3032839
- Miralles-Pechuán, L., Jiménez, F., Ponce, H., & Martínez-Villaseñor, L. (2020). A deep Q-learning/genetic algorithms based novel methodology for optimizing Covid-19 pandemic government actions. In arXiv Prepr. arXiv2005.07656.
- Miranda, I. D. S., Diacon, A. H., & Niesler, T. R. (2019). A comparative study of features for acoustic cough detection using deep architectures*. 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp. 2601–2605, https://doi.org/10.1109/EMBC.2019.8856412.
- Mohamadou, Y., Halidou, A., & Kapen, P. T. (2020). A review of mathematical modeling, artificial intelligence and datasets used in the study, prediction and management of COVID-19. Applied Intelligence, 50(11), 3913–3925. https://doi.org/10.1007/s10489-020-01770-9
- Mohammadi, F., et al. (2021). Artificial neural network and logistic regression modelling to characterize COVID-19 infected patients in local areas of Iran. Biomedical Journal, (March).https://doi.org/10.1016/j.bj.2021.02.006.
- Mohanty, S., Harun AI Rashid, M., Mridul, M., Mohanty, C., & Swayamsiddha, S. (2020). Application of Artificial Intelligence in COVID-19 drug repurposing. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), 1027–1031. https://doi.org/10.1016/j.dsx.2020.06.068
- More, S., et al. (2020). Security assured CNN-based model for reconstruction of medical images on the internet of healthcare things. IEEE Access, 8, 126333–126346. https://doi.org/10.1109/ACCESS.2020.3006346
- Mori, K., Wada, T., & Ohtsuki, K. (2016). A new disaster recognition algorithm based on SVM for ERESS: Buffering and bagging-SVM. 2016 45th International Conference on Parallel Processing Workshops (ICPPW).
- Moskal, M., et al. (2020). Suggestions for second-pass anti-COVID-19 drugs based on the Artificial Intelligence measures of molecular similarity, shape and pharmacophore distribution. ChemRxiv, 1–22. https://doi.org/10.26434/chemrxiv.12084690.v2.
- Mowery, C. T., Marson, A., song, Y. S., & Ye, C. J. Improved COVID-19 serology test performance by integrating multiple lateral flow assays using machine learning. (2020, January). medRxiv, 2020. 07.15.20154773, https://doi.org/10.1101/2020.07.15.20154773.
- Muthya, S., Nair, R. S., Arokiaswamy, T. P., & Prakash, A. Using machine learning to assess Covid-19 risks. (2020, January). medRxiv, 2020. 06.23.20137950, https://doi.org/10.1101/2020.06.23.20137950.
- Mvd, A. (June, 2020). Covid-19 x rays. [Online]. Retrieved https://www.kaggle.com/andrewmvd/convid19-X-rays
- Nallanthighal, V. S., Härmä, A., & Strik, H. (2019). Deep sensing of breathing signal during conversational speech. Interspeech, 2019.
- Narin, A., Kaya, C., & Pamuk, Z. (2020). Department of biomedical engineering, Zonguldak Bulent Ecevit University, 67100, Zonguldak, Turkey. arXiv Prepr. arXiv2003.10849, Retrieved https://arxiv.org/abs/2003.10849
- Naudé, W. (2020a). Artificial intelligence vs COVID-19: Limitations, constraints and pitfalls. Ai & Society, 35(3), 761–765. https://doi.org/10.1007/s00146-020-00978-0
- Naudé, W. (2020b). Artificial intelligence versus COVID-19 in developing countries. no. May. .https://www.wider.unu.edu/sites/default/files/Publications/Background-note/PDF/bn2020-4-ai-vs-covid-19-developing-countries.pdf
- Nawaz, N., Gomes, A. M., & Saldeen, M. A. (2020). Artificial intelligence (AI) applications for library services and resources in COVID-19 pandemic. Journal Crit. Rev, 7(18), 1951–1955. https://doi.org/10.31838/jcr.07.18.244. Available
- NCBI. (2020). LitCovid. [Online]. Retrieved https://www.ncbi.nlm.nih/gov/research/coronavirus
- nCoV2019Data. ncov2019 epidemiological data. Coronavirus Dashboard. Retrieved April 23, 2021. https://github.com/beoutbreakprepared/nCoV2019
- New York University. (2020). App determines COVID-19 disease severity using artificial intelligence, biomarkers. Retrieved https://www.sciencedaily.com/releases/2020/06/200603132529.html
- Nguyen, D. C., Ding, M., Pathirana, P. N., & Seneviratne, A. (2020). Blockchain and AI-based solutions to combat Coronavirus (COVID-19)-like epidemics: A survey. no. April, 1–15. https://doi.org/10.36227/techrxiv.12121962.v1.
- Nhsx. (June, 2020). Covid-19 x rays. . [Online]. Retrieved https://nhsx.github.io/covid-chest-imaging-database/
- Ni, Q., et al. (2020). A deep learning approach to characterize 2019 coronavirus disease (COVID-19) pneumonia in chest CT images. European Radiology, 30(12), 6517–6527. https://doi.org/10.1007/s00330-020-07044-9
- NPGEO. (2020). Dataset of infections in germany. [Online]. Retrieved https://npgeo-corona-npgeo-de.hub.arcgis.com/datasets/dd4580c810204019a%7b8eb3e0b329dd6_0/data
- Nytimes. nytimes/covid-19-data. GitHub. Retrieved April 23, 2021. https://github.com/nytimes/covid-19-data
- Ogundokun, R. O., Lukman, A. F., Kibria, G. B. M., Awotunde, J. B., & Aladeitan, B. B. (2020). Predictive modelling of COVID-19 confirmed cases in Nigeria. Infect. Dis. Model, 5, 543–548.
- Ong, E., Wong, M. U., Huffman, A., & He, Y. (2020). COVID-19 coronavirus vaccine design using reverse vaccinology and machine learning. Frontiers in Immunology, 11(July), 1581. https://doi.org/10.3389/fimmu.2020.01581
- Orrù, G., Monaro, M., Conversano, C., Gemignani, A., & Sartori, G. (2020). Machine learning in psychometrics and psychological research. Frontiers in Psychology, 10(January), 1–10. https://doi.org/10.3389/fpsyg.2019.02970
- Öztürk, H., Özgür, A., & Ozkirimli, E. (2018). DeepDTA: Deep drug-target binding affinity prediction. Bioinformatics, 34(17), i821–i829. https://doi.org/10.1093/bioinformatics/bty593
- Ozturk, T., Talo, M., Yildirim, E. A., Baloglu, U. B., Yildirim, O., & Acharya, U. R. (2020). Automated detection of COVID-19 cases using deep neural networks with X-ray images. Computers in Biology and Medicine, 121, 103792. https://doi.org/10.1016/j.compbiomed.2020.103792
- Pahikkala, T., et al. (2015, March). Toward more realistic drug–target interaction predictions. Briefings in Bioinformatics, 16 (2), 325–337. https://doi.org/10.1093/bib/bbu010.
- Panday, A. (2020). A complete survey on automatically diagnosing COVID-19 In the field of computer vision and a collection of medical images
- Pandey, G., Chaudhary, P., Gupta, R., & Pal, S. (2020). SEIR and regression model based COVID-19 outbreak predictions in India. In arXiv Prepr. arXiv2004.00958.
- Pandey, R. et al. (2020). A machine learning application for raising WASH awareness in the times of COVID-19 Pandemic (Preprint). In arXiv preprint arXiv:2003.07074.
- Pandit, M. K., & Banday, S. A. (2020). SARS n-CoV2-19 detection from chest X-ray images using deep neural networks. International Journal of Pervasive Computing and Communications, 16(5), 419–427. https://doi.org/10.1108/IJPCC-06-2020-0060
- Partila, P., Tovarek, J., Rozhon, J., & Jalowiczor, J. (2019, May). Human stress detection from the speech in danger situation. Proc.SPIE, 10993. https://doi.org/10.1117/12.2521405.
- Peiffer-Smadja, N., Maatoug, R., Lescure, F.-X., D’Ortenzio, E., Pineau, J., & King, J.-R. (2020). Machine learning for COVID-19 needs global collaboration and data-sharing. Nature Machine Intelligence, 2(6), 293–294. https://doi.org/10.1038/s42256-020-0181-6
- Pham, V., Nguyen, D. C., Huynh-The, T., Hwang, W.-J., & Pathirana, P. N. (2020). Artificial Intelligence (AI) and Big Data for Coronavirus (COVID-19) Pandemic: A Survey on the State-of-the-Arts.
- PhysicsWorld. AI checks CT Scans for COVID-19. 2020. Retrieved https://physicsworld.com/a/ai-checks-ct-scans-forcovid-19
- Pirouz, B., Nejad, H. J., Violini, G., & Pirouz, B. The role of swab tests to decrease the stress by COVID-19 on the health system using AI, MLR & statistical analysis. (2020, January). medRxiv, 2020. 06.02.20120394, https://doi.org/10.1101/2020.06.02.20120394.
- Polese, M., Jana, R., Kounev, V., Zhang, K., Deb, S., & Zorzi, M. (2020). Machine learning at the edge: A data-driven architecture with applications to 5g cellular networks. IEEE Transactions on Mobile Computing, 1. https://doi.org/10.1109/TMC.2020.2999852
- Prachar, M., et al. (2020 January). COVID-19 vaccine candidates: prediction and validation of 174 SARS-CoV-2 Epitopes. bioRxiv, 2020. 03.20.000794. https://doi.org/10.1101/2020.03.20.000794.
- Prakash Jha, I., Awasthi, R., Kumar, A., Kumar, V., & Sethi, T. (2020). Explainable-Machine-Learning to discover drivers and to predict mental illness during COVID-19. medRxiv, 2020. 07.19.20157164. https://doi.org/10.1101/2020.07.19.20157164.
- Punn, N. S., Sonbhadra, S. K., & Agarwal, S. (2020). Monitoring COVID-19 social distancing with person detection and tracking via fine-tuned YOLO v3 and Deepsort techniques. In arXiv (pp. 1–10).
- Qi, X., et al. (2020). Machine learning-based CT radiomics model for predicting hospital stay in patients with pneumonia associated with SARS-CoV-2 infection: A multicentre study. medRxiv.
- Qin, B., & Li, D. (2020). Identifying facemask-wearing condition using image super-resolution with classification network to prevent COVID-19. Sensors, 20(18), 18. https://doi.org/10.3390/s20185236
- RadBoudumc. (2020). Evaluation of an AI System for detection of COVID-19 on Chest X-ray Images. Retrieved https://www.radboudumc.nl/en/news/2020/evaluation-of-an-ai-system-for-detection-of-covid-19-on-chest-x-ray-images
- Rahman, M. A., Zaman, N., Asyhari, A. T., Al-Turjman, F., Alam Bhuiyan, M. Z., & Zolkipli, M. F. (2020). Data-driven dynamic clustering framework for mitigating the adverse economic impact of Covid-19 lockdown practices. Sustainable Cities and Society, 62, 102372. https://doi.org/10.1016/j.scs.2020.102372
- Rahman, M. S., et al. (2020). Epitope-based chimeric peptide vaccine design against S, M and E proteins of SARS-CoV-2, the etiologic agent of COVID-19 pandemic: An in silico approach. Peer Journal, 8, e9572. https://doi.org/10.7717/peerj.9572
- Rahmatizadeh, S., Valizadeh-Haghi, S., & Dabbagh, A. (2020). The role of artificial intelligence in management of critical COVID-19 patients. J. Cell. Mol. Anesth, 5(1), 16–22. https://doi.org/10.22037/jcma.v5i1.29752
- Ramsundar, B., Eastman, P., Walters, P., & Pande, V. (2019). Deep learning for the life sciences: Applying deep learning to genomics, microscopy, drug discovery, and more. OReilly.
- Ranjan, R. (n.d.). “Callibration in machine learning” Retrieved https://medium.com/analytics-vidhya/calibration-in-machine-learning-e7972ac93555
- Rao, A. S. R. S., & Vazquez, J. A. (2020). Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infection Control & Hospital Epidemiology, 41(7), 826–830. https://doi.org/10.1017/ice.2020.61
- Rath, S., Tripathy, A., & Tripathy, A. R. (2020). Prediction of new active cases of coronavirus disease (COVID-19) pandemic using multiple linear regression model. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), 1467–1474. https://doi.org/10.1016/j.dsx.2020.07.045
- Ravelo, J. (2020). This nonprofit needs your cough sounds to detect COVID-1. Retrieved https://www.devex.com/news/this-nonprofit-needs-your-cough-sounds-to-detect-covid-19-97141
- Razai, M. S., Doerholt, K., Ladhani, S., & Oakeshott, P. (2020). Coronavirus disease 2019 (covid-19): A guide for uk gps. BMJ, 368.
- Réda, C., Kaufmann, E., & Delahaye-Duriez, A. (2020). Machine learning applications in drug development. Computational and Structural Biotechnology Journal, 18, 241–252. https://doi.org/10.1016/j.csbj.2019.12.006
- Rees, V. AI and cloud computing used to develop COVID-19 vaccine. Drug Target Review, Retrieved April 8, 2020. https://www.drugtargetreview.com/news/59650/ai-and-cloud-computing-used-to-develop-covid-19-vaccine
- Ribeiro, M. H. D. M., Da Silva, R. G., Mariani, V. C., & Coelho, L. D. S. (2020). Short-term forecasting COVID-19 cumulative confirmed cases: Perspectives for Brazil. Chaos, Solitons, and Fractals, 135, 109853. https://doi.org/10.1016/j.chaos.2020.109853
- Ridley, E. (2020). AI can assess COVID-19 severity on Chest X-rays. Retrieved https://www.auntminnie.com/index.aspx?sec=ser&sub=def&pag=dis&ItemID=129674
- Rosenbusch, H., Soldner, F., Evans, A. M., & Zeelenberg, M. (2021). Supervised machine learning methods in psychology: A practical introduction with annotated R code. Social and Personality Psychology Compass, 15(2). https://doi.org/10.1111/spc3.12579
- Sadhukhan, S., Banerjee, S., Das, P., & Sangaiah, A. K. (2018). Producing better disaster management plan in post-disaster situation using social media mining. In Computational Intelligence for multimedia big data on the cloud with engineering applications (pp. 171–183).
- Sahu, B., Das, P. K., Kabat, M. R., & Kumar, R. (2021). Prevention of Covid-19 affected patient using multi robot cooperation and Q-learning approach: A solution. In Qual. Quant. (pp. 1–29).
- Sangiorgio, V., & Parisi, F. (2020, October). A multicriteria approach for risk assessment of Covid-19 in urban district lockdown. Safety Science, 130, 104862. https://doi.org/10.1016/j.ssci.2020.104862
- Saqib, M. (2021). Forecasting COVID-19 outbreak progression using hybrid polynomial-Bayesian ridge regression model. Applied Intelligence, 51(5), 2703–2713. https://doi.org/10.1007/s10489-020-01942-7
- Sarkar, B., Ullah, M. A., Johora, F. T., Taniya, M. A., & Araf, Y. (2020, January). The essential facts of wuhan novel coronavirus outbreak in china and epitope-based vaccine designing against 2019-nCoV. bioRxiv 02.05.935072. (pp. 2020).
- Schuller, B. W., Schuller, D. M., Qian, K., Liu, J., Zheng, H., & Li, X. (2020). COVID-19 and computer audition: An overview on what speech & sound analysis could contribute in the SARS-COV-2 corona crisis. arXiv, (March). https://doi.org/10.3389/fdgth.2021.564906
- Scudellari, M. (2020). Hospitals deploy AI tools to detect COVID-19 on chest scans. Retrieved https://spectrum.ieee.org/the-human-os/biomedical/imaging/hospitals-deploy-ai-tools-detect-covid19-chest-scans
- Sesagiri Raamkumar, A., Tan, S. G., & Wee, H. L. (2020). Use of health belief model–based deep learning classifiers for covid-19 social media content to examine public perceptions of physical distancing: model development and case study. JMIR Public Health and Surveillance, 6(3), e20493. https://doi.org/10.2196/20493
- Sethy, P. K., Behera, S. K., Ratha, P. K., & Biswas, P. (2020, April 22). Detection of coronavirus disease (COVID-19) based on deep features and support vector machine. In Preprints (pp. 202003. 0300.v1).
- Shaikh, F., Andersen, M. B., Sohail, M. R., Mulero, F., Awan, O., Dupont-Roettger, D., Kubassova, O., Dehmeshki, J., & Bisdas, S. (2021). Current landscape of imaging and the potential role for artificial intelligence in the management of COVID-19. Current Problems in Diagnostic Radiology, 50(3), 430–435. https://doi.org/10.1067/j.cpradiol.2020.06.009
- Sharma, K., Seo, S., Meng, C., Rambhatla, S., Dua, A., & Liu, Y. (2020). arXiv:2003.12309. Coronavirus on social media: Analyzing misinformation in Twitter conversations.
- Sharma, N., et al. (2020). Coswara - A database of breathing, cough, and voice sounds for COVID-19 diagnosis. Proc. Annu. Conf. Int. Speech Commun. Assoc. INTERSPEECH, 2020-October, 4811–4815. https://doi.org/10.21437/Interspeech.2020-2768
- Sharma, S., & Gupta, Y. K. (2021, January). Predictive analysis and survey of COVID-19 using machine learning and big data. Journal of Interdisciplinary Mathematics, 24(1), 175–195. https://doi.org/10.1080/09720502.2020.1833445
- Shi, F. et al. (2020). Review of artificial intelligence techniques in imaging data acquisition, segmentation and diagnosis for COVID-19. In IEEE reviews in biomedical engineering.
- Shi, F., et al. (2021). Large-scale screening to distinguish between COVID-19 and community-acquired pneumonia using infection size-aware classification. Physics in Medicine and Biology, 66(6), 065031. https://doi.org/10.1088/1361-6560/abe838
- Shi, Y., et al. (2020). D3Targets-2019-nCoV: A webserver for predicting drug targets and for multi-target and multi-site based virtual screening against COVID-19. Acta Pharmaceutica Sinica B, 10(7), 1239–1248. https://doi.org/10.1016/j.apsb.2020.04.006
- Shinde, G. R., Kalamkar, A. B., Mahalle, P. N., Dey, N., Chaki, J., & Hassanien, A. E. (2020). Forecasting models for coronavirus disease (COVID-19): A survey of the state-of-the-art. SN Computer Science, 1(4), 1–15. https://doi.org/10.1007/s42979-020-00209-9
- Simply, R. M., Dafna, E., & Zigel, Y. (2018). Obstructive sleep apnea (OSA) classification using analysis of breathing sounds during speech,” 2018 26th European Signal Processing Conference (EUSIPCO), pp. 1132–1136.
- Simsek, M., & Kantarci, B. (2020). Artificial intelligence-empowered mobilization of assessments in COVID-19-like pandemics: A case study for early flattening of the curve. International Journal of Environmental Research and Public Health, 17(10), 10. https://doi.org/10.3390/ijerph17103437
- SIRM. (2020a). Covid-19-BSTI imaging database. [Online]. Retrieved https://www.bsti.org.uk/training-and-education/covid-19-bsti-imaging-da%tabase/
- SIRM. (2020b). COVID-19 DATABASE. [Online]. Retrieved https://www.sirm.org/category/senza-categoria/covid-19
- Smith, S. (March, 2020). Coronavirus (covid19) tweets. [Online]. Retrieved www.kaggle.com/smid80/coronavirus-covid19-tweets
- Soares, F., Villavicencio, A., José Anzanello, M., Fogliatto, F. S., Idiart, M. A. P., & Stevenson, M. A novel high specificity COVID-19 screening method based on simple blood exams and artificial intelligence. (2020, January). medRxiv, 2020. 04.10.20061036, https://doi.org/10.1101/2020.04.10.20061036.
- Soofi, A., & Awan, A. (2017). Classification Techniques in Machine Learning: Applications and Issues. Journal of Basic & Applied Sciences, 13, 459–465. https://doi.org/10.6000/1927-5129.2017.13.76
- Stevens, S. S., Volkmann, J., & Newman, E. B. (1937). A scale for the measurement of the psychological magnitude pitch. The Journal of the Acoustical Society of America, 8(3), 185–190. https://doi.org/10.1121/1.1915893
- sudalairajkumar Data. Novel corona-virus dataset. GitHub. [Online]. Retrieved April 23, 2021. https://github.com/SudalaiRajkumar
- Sufian, A., Ghosh, A., Sadiq, A. S., & Smarandache, F. (2020). A survey on deep transfer learning to edge computing for mitigating the COVID-19 pandemic. Journal of Systems Architecture, 108, 101830. https://doi.org/10.1016/j.sysarc.2020.101830
- Sun, -N.-N., et al. (2020, January).A prediction model based on machine learning for diagnosing the early COVID-19 patients. medRxiv, https://doi.org/10.1101/2020.06.03.20120881.
- TABIP. (2020). Coronavirus vaccine candidate developed in adelaide lab to start human trials. Retrieved https://covid19.tabipacademy.com/2020/07/03/coronavirus-vaccine-candidate-developed-in-adelaide-lab-to-start-human-trials
- Tang, B., He, F., Liu, D., Fang, M., Wu, Z., & Xu, D. (2020, January). AI-aided design of novel targeted covalent inhibitors against SARS-CoV-2. bioRxiv 03.03.972133. (pp. 2020).
- Tarrataca, L., Dias, C. M., Haddad, D. B., & De Arruda, E. F. (2021). Flattening the curves: On-off lock-down strategies for COVID-19 with an application to Brazil. J. Math. Ind, 11(1). https://doi.org/10.1186/s13362-020-00098-w
- Tayarani N, M. H. (2021). Applications of artificial intelligence in battling against covid-19: A literature review. Chaos, Solitons, and Fractals, 142, 110338. https://doi.org/10.1016/j.chaos.2020.110338
- Tschoellitsch, T., Dünser, M., Böck, C., Schwarzbauer, K., & Meier, J. (2020). Machine learning prediction of SARS-CoV-2 polymerase chain reaction results with routine blood tests. Laboratory Medicine. https://doi.org/10.1093/labmed/lmaa111
- Tsikala Vafea, M., et al. (2020). Emerging technologies for use in the study, diagnosis, and treatment of patients with COVID-19. Cellular and Molecular Bioengineering, 13(4), 249–257. https://doi.org/10.1007/s12195-020-00629-w
- Uddin, M. I., Shah, S. A. A., & Al-Khasawneh, M. A. (2020). A novel deep convolutional neural network model to monitor people following guidelines to avoid COVID-19. Journal of Sensors, 2020, 1–15. https://doi.org/10.1155/2020/8856801
- Ulhaq, A., Khan, A., Gomes, D., & Paul, M. (2020). Computer vision for COVID-19 control: A survey. In arXiv (pp. 1–24).
- Unberath, M., Ghobadi, K., Levin, S., Hinson, J., & Hager, G. D. (2020). Artificial intelligence-based clinical decision support for COVID-19 – Where Art Thou? Advanced Intelligent Systems, 2(9), 2000104. https://doi.org/10.1002/aisy.202000104
- Vadyala, S. R., Betgeri, S. N., Sherer, E. A., & Amritphale, A. (2020). Prediction of the number of covid-19 confirmed cases based on k-means-lstm. In arXiv Prepr. arXiv2006.14752.
- Vaishya, R., Javaid, M., Khan, I. H., & Haleem, A. (2020). Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(4), 337–339. https://doi.org/10.1016/j.dsx.2020.04.012
- Vamathevan, J., et al. (2019). Applications of machine learning in drug discovery and development. Nature Reviews Drug Discovery, 18(6), 463–477. https://doi.org/10.1038/s41573-019-0024-5
- van der Schaar, M., et al. (2021). How artificial intelligence and machine learning can help healthcare systems respond to COVID-19. Machine Learning, 110(1), 1–14. https://doi.org/10.1007/s10994-020-05928-x
- VIDA. LungPrint Clinical Solutions. 2020. Retrieved https://vidalung.ai/clinical_solutions
- W. Inc. 2020. World’s air pollution: Real-time air quality index. [Online]. Retrieved https://waqi.info
- Wang, B., Sun, Y., Duong, T. Q., Nguyen, L. D., & Hanzo, L. (2020). Risk-aware identification of highly suspected COVID-19 Cases in Social IoT: A joint graph theory and reinforcement learning approach. In IEEE Access, 8, 115655–115661. https://doi.org/10.1109/ACCESS.2020.3003750
- Wang, D., et al. (2020). Agent-based simulation model and deep learning techniques to evaluate and predict transportation trends around COVID-19 arXiv Prepr. arXiv2010.09648.
- Wang, L., Lin, Z. Q., & Wong, A. (2020). COVID-Net: A tailored deep convolutional neural network design for detection of COVID-19 cases from chest X-ray images. Sci. Rep, 10(1), 1–12. https://doi.org/10.1038/s41598-020-76550-z
- Wang, L., & Wong, A. (2020). COVID-Net: A tailored deep convolutional neural network design for detection of COVID-19 cases from chest radiography images. Scientific Reports, 10(1), 1–12.
- Wang, S., et al., (2021a). A deep learning algorithm using CT images to screen for Corona virus disease (COVID-19). European Radiology, 31(8), 6096–6104. https://doi.org/10.1007/s00330-021-07715-1
- Wang, S., et al. (2021b). A deep learning algorithm using CT images to screen for Corona Virus Disease (COVID-19). European Radiology, 1–9.
- Wang, Y., et al. (2020). Unobtrusive and automatic classification of multiple people’s abnormal respiratory patterns in real time using deep neural network and depth camera. IEEE Internet of Things Journal, 7(9), 8559–8571. https://doi.org/10.1109/JIOT.2020.2991456
- WHO. 2020. Global research on novel coronavirus-2019. [Online]. Retrieved https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-%research-on-novel-coronavirus-2019/ncov
- Wu, J., et al. (2020). Rapid and accurate identification of COVID-19 infection through machine learning based on clinical available blood test results. medRxiv, https://doi.org/10.1101/2020.04.02.20051136.
- Wurtzer, S., Marechal, V., Mouchel, J.-M., & Moulin, L. (2020). Time course quantitative detection of sars-cov-2 in parisian wastewaters correlates with covid-19 confirmed cases. medRxiv.
- Xu, W., Sun, -N.-N., Gao, H.-N., Chen, Z.-Y., Yang, Y., & Tang, -L.-L. Risk factors analysis of COVID-19 patients with ARDS and prediction based on machine learning. Sci. Reports |, 11, 2933. 123AD. https://doi.org/10.1038/s41598-021-82492-x
- Xue, H., Li, J., Xie, H., & Wang, Y. (2018, July). Review of drug repositioning approaches and resources. International Journal of Biological Sciences, 14(10), 1232–1244. https://doi.org/10.7150/ijbs.24612
- Yadav, S., Keerthana, M., Gope, D., Maheswari K, U., & Ghosh, P. K. (2020). Analysis of acoustic features for speech sound based classification of asthmatic and healthy subjects. ICASSP 2020-2020 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), pp. 6789–6793, https://doi.org/10.1109/ICASSP40776.2020.9054062.
- Yan, L., et al. (2020). A machine learning-based model for survival prediction in patients with severe COVID-19 infection. medRxiv, https://doi.org/10.1101/2020.02.27.20028027.
- Yang, D., Yurtsever, E., Renganathan, V., Redmill, K. A., & Özgüner, Ü. (2020). A vision-based social distancing and critical density detection system for COVID-19. In arXiv.
- Yang, H. S., et al. (2020, November). Routine laboratory blood tests predict SARS-CoV-2 infection using machine learning. Clinical Chemistry, 66 (11), 1396–1404. https://doi.org/10.1093/clinchem/hvaa200.
- Yeşilkanat, C. M. (2020). Spatio-temporal estimation of the daily cases of COVID-19 in worldwide using random forest machine learning algorithm. Chaos, Solitons, and Fractals, 140, 110210. https://doi.org/10.1016/j.chaos.2020.110210
- Yin, R., Tran, V. H., Zhou, X., Zheng, J., & Kwoh, C. K. (2018). Predicting antigenic variants of H1N1 influenza virus based on epidemics and pandemics using a stacking model. Plos One, 13(12), e0207777. https://doi.org/10.1371/journal.pone.0207777
- Yoo, S. H., et al. (2020). Deep learning-based decision-tree classifier for COVID-19 Diagnosis From Chest X-ray Imaging. Frontiers in Medicine, 7, 427. https://doi.org/10.3389/fmed.2020.00427
- Zarei, K., Farahbakhsh, R., Crespi, N., & Tyson, G. (2020). arXiv:2004.12226. A first instagram dataset on covid-19.
- Zeng, X., Zhu, S., Liu, X., Zhou, Y., Nussinov, R., & Cheng, F. (2019, December). deepDR: A network-based deep learning approach to in silico drug repositioning. Bioinformatics, 35(24), 5191–5198. https://doi.org/10.1093/bioinformatics/btz418
- Zhang, K., et al. (2020, June). Clinically applicable AI system for accurate diagnosis, quantitative measurements, and prognosis of COVID-19 pneumonia using computed tomography. Cell, 181 (6), 1423–1433.e11. https://doi.org/10.1016/j.cell.2020.04.045.
- Zhang, T., & Lin, G. (2021). Generalized k -means in GLMs with applications to the outbreak of COVID-19 in the United States. Computational Statistics & Data Analysis, 159, 107217. https://doi.org/10.1016/j.csda.2021.107217
- Zhang, W., et al. (2021). Analysis of COVID-19 epidemic and clinical risk factors of patients under epidemiological Markov model. Results in Physics, 22, 103881. https://doi.org/10.1016/j.rinp.2021.103881
- Zhao, D., et al. (2020). A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clinical Infectious Diseases, 71(15), 756–761. https://doi.org/10.1093/cid/ciaa247
- Zhao, J., Zhang, Y., He, X., & Xie, P. (2020). arXiv:2003.13865. COVID-CT-Dataset: A CT scan dataset about COVID-19.
- Zhao, Z., Li, X., Liu, F., Zhu, G., Ma, C., & Wang, L. (2020). Prediction of the covid-19 spread in african countries and implications for prevention and controls: A case study in south africa, egypt, algeria, nigeria, senegal and kenya. Science of the Total Environment, 729, 138959. https://doi.org/10.1016/j.scitotenv.2020.138959. Art.
- Zhavoronkov, A., et al. (2020a). Potential COVID-2019 3c-like protease in- hibitors designed using generative deep learning approaches. Insilico Medicine Hong Kong Ltd A, 307, E1.
- Zhavoronkov, A., et al. (2020b). Potential 2019-nCoV 3C-like protease inhibitors designed using generative deep learning approaches. ChemRxiv, (2).https://doi.org/10.26434/chemrxiv.11829102.v2.
- Zheng, C., et al. (2020). Deep Learning-based Detection for COVID-19 from Chest CT using Weak Label. medRxiv, 1–13. https://doi.org/10.1101/2020.03.12.20027185.