?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
In recent years, Nigeria has experienced increased outbreaks of Monkeypox, Ebola, Lassa fever, and the latest Coronavirus disease (COVID-19) pandemic. As a result of the epidemics, highly infectious materials such as contaminated needles, syringes, soiled bandages, and contagious disposable personal protective equipment are on the rise. This has resulted in vast volumes of medical waste generation in Nigeria. This study employs relevant scientific works of literature in scholarly sites of Web of Science and Scopus, governments, and multilateral organizations regulatory guidelines for COVID-19. This is to conduct a critical analysis of COVID-19ʹs impact on medical waste management and disposal measures in Nigeria during the pandemic. Results show that, with over 143.01% increase in less than a year, Nigeria’s daily average COVID-related medical waste increased from 131.24 tons/day in August 2020 to 318.92 tons/day in January 2021, leading to environmental pollution and a high risk of infection among health workers. The paper further highlights the total daily estimates of PPE (facemasks) used during the COVID-19 pandemic as 171,908,091. Medical Waste Management (MWM) challenges persist in most developing and least developed nations as the global population and healthcare services rise. As it stands, Nigeria’s population is expected to exceed that of the United States by 2050, and with frequent outbreaks of an epidemic, there is a need for an effective MWM plan. Rapid revalidation and appraisal of the Sustainable Development Goals and the Water, Sanitation, and Hygiene (WASH) for health care facilities in most developing countries is required. The inclusion of epidemic and pandemic readiness, natural disasters preparedness, and climate change is critical in the global objectives of the Sustainable Development Goals.
PUBLIC INTEREST STATEMENT
The primary effects of COVID-19 on waste management are increased environmental pollution, a high risk of infection among public health workers, and large volumes of medical waste (personal protective equipment). Today, constant disease outbreaks such as Ebola, monkeypox, Lassa fever, and the most recent Coronavirus disease make medical waste management critical to public health. A robust inclusive policy response framework and pandemic readiness metrics should be entailed in the Sustainable Development Goal (SDG) and the Water, Sanitation, and Hygiene (WASH) services for health care facilities. As a result, an urgent call for more research into the environmental epidemiology of diseases caused by waste management is emphasized.
1. Introduction
Like other infrastructure, medical waste management (MWM) systems are challenged by the pandemic of Coronavirus disease (COVID-19). The highly contagious nature of the Severe Acute Respiratory Syndrome Coronavirus 2, also known as SARS-CoV-2 or COVID-19, causes an increase in the generation of infectious waste materials such as contaminated needles, syringes, soiled bandages, and disposable personal protective equipment (Etim, Academe et al., Citation2021; Oyedotun et al., Citation2020). The SARS-CoV-2 virus, responsible for Coronavirus disease (COVID-19), has progressed into several variants since its discovery. The situation seems critical with the advent of the Delta and Omicron variants of SARS-CoV-2—variants of concern (VOCs) as described by the World Health Organization (WHO, Citation2020b; UNICEF, Citation2021). The increasing virulence, transmissibility, and environmental epidemiology of COVID-19 require the careful handling of medical wastes.
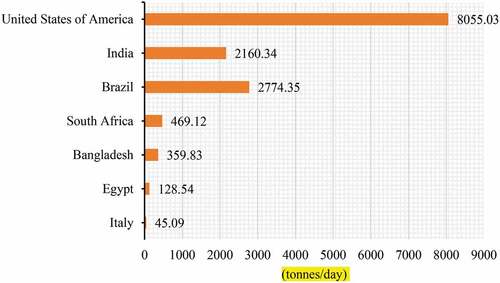
Since the identification of COVID-19, cities worldwide have experienced a rise in the volume of medical wastes generated. For instance, Wuhan, China’s COVID-19 epicentre, experienced a massive surge in medical waste from 40–50 tonnes/day prior to the epidemic to approximately 247 tonnes on 1 March 2020. Additionally, there were simultaneous spikes in cities like Bangkok, Kuala, Manila, Hanoi, and Kuala Lumpur, generating 154–280 tonnes/day more medical waste prior to the pandemic (Asian Development Bank, Citation2020; Si & Li, Citation2020; Sonne et al., Citation2020). In March 2020, medical waste in Malaysia grew by 30% (Agamuthu & Barasarathi, Citation2020). South Africa recorded 469.12 tonnes/day in the volume of biomedical wastes produced during the COVID-19 pandemic (Haque et al., Citation2021). In Canada, significant differences in the amount of waste disposal were reported between May and September 2020 as seasonal effects were observed in generation rates (Richter et al., Citation2021). The risk of COVID contractions, rapid testing kits, and single-use disposable facemasks has led to a surge in COVID-related wastes. For developing and least developed nations, the risk of COVID contractions from potentially hazardous waste is imminent as waste management systems are fragile (Oyedotun et al., Citation2020). For example, more health workers in Nigeria have tested positive for COVID-19 than any other African country except South Africa. Since healthcare professionals are at the forefront of the response to the COVID-19 pandemic, they are vulnerable to several health risks like exposure to SARS–CoV–2 and other infections, stigmatization, discrimination, prolonged workload, even death (WHO, Citation2021).
MWM is one of humanity’s diverse and daunting problems as the global population increases and the need for healthcare services rise (Windfeld & Brooks, Citation2015). For instance, Nigeria’s population is expected to exceed the United States by 2050 (United Nations, Citation2017), thereby creating severe concerns for its medical waste generation and management. Unsatisfactory segregation of waste at various points of generation, low compliance to healthcare regulations and guidelines, inadequate awareness among healthcare professionals, and the lack of infection control committees in medical facilities have stymied efficient and effective MWM in Nigeria (Oli et al., Citation2016). The recent global pandemic has identified weaknesses in our waste management and disposal chains, which could endanger public health and foster environmental contamination. The pandemic of COVID-19 has revealed how fragile MWM chains are and how this could lead to an increasing environmental pollution scenario (Sonne et al., Citation2020). During epidemics and pandemics, hospitals and healthcare facilities are prone to experience a surge in the number of medical or clinical wastes.
Globally, the challenge in the vocabulary of medical waste has given rise to the lack of strict definition and regulations among countries (Insa et al., Citation2010), resulting in disparate disposal and management practices. The emergence of COVID-19 calls for a prompt unification in guidelines and regulations on healthcare and medical wastes. Several terms describe medical waste, which is often used synonymously. They include; healthcare waste, regulated medical waste, infectious medical waste, pharmaceutical waste, treated biomedical waste, and hospital waste. All through this review, “medical waste” will be adopted and used. Therefore, to achieve this review’s objective, we searched for recent scientific works of literature in scholarly sites of Web of Science and Scopus journals, governments, and multilateral organizations documentation and regulatory guidelines for COVID-19. The keywords used are “medical waste,” “COVID-19”, “healthcare waste,” “SARS-CoV-2”, “pandemic,” and “medical waste management.” Obtained literature and guidelines were further screened for articles in the English language, and selected articles were analyzed vis a vis chosen keywords.
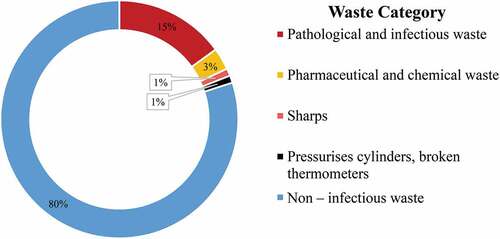
The World Health Organization (WHO) defines medical waste as all waste-type produced within a healthcare facility, laboratories related to medical procedures, and research centres. As estimated by WHO, about 75–90% of the total volume of waste produced by health care operations is domestic, non-hazardous, or general waste. The remaining 15–25% are hazardous, which could be radioactive, toxic, or infectious, and must be handled carefully to prevent contaminations, as presented in (Aung et al., Citation2019; Chartier et al., Citation2014). However, findings show that 70% of these wastes could have been reused, recycled, or segregated in a way that reduces cost. Also, hazardous waste disposal costs are ten times the cost of non-hazardous waste disposal, and the environmental impact is far worse (WHO, Citation2018; Wormer et al., Citation2013).
While medical waste represents a small portion of all municipal solid waste (MSW) sources, its management is enormously significant because of its potential environmental threats to public health (Jang, Citation2019). Inversely, the emergence of the COVID pandemic shows large volumes of mixed medical wastes, biomedical wastes and municipal solid wastes. In 2020, there seems to be a broader range of bimodality in daily mixed solid waste data (Richter et al., Citation2021). Indubitably, poor MWM is a significant cause of nosocomial infections like urinary tract infection, gastroenteritis (stomach flu), and staphylococcus aureus in Nigeria (Stanley & Okpara, Citation2011). Each year, around 5.2 million people worldwide (4 million infants inclusive) are reported dead from waste-related diseases (Abd El-Salam, Citation2010). Waste from hospitals is now identified as a significant issue that adversely affects humans and the environment either via direct or indirect contact.
The disruption by COVID-19 has caused severe setbacks in the activities of Water, Sanitation and Hygiene (WASH) in health care facilities for most developing countries (WHO & UNICEF, Citation2015) and a drawback in the 2030 Agenda for Sustainable Development (UN Department of Economic and Social Affairs, Citation2020). Hence, there is a need to revalidate and reassess global objectives for waste management systems with consideration into key events like epidemic and pandemic readiness, natural disasters, and climate change. This paper highlights the challenge of the COVID-19 pandemic on MWM and disposal practices. Also, the estimation of discarded facemasks is emphasized with an increase in the volume of medical waste prior to the COVID-19 pandemic. The study recommends developing a pandemic waste management plan to cater to surges in medical wastes and the strengthening of environmental epidemiology as a response to COVID-19, Ebola Fever, Lassa Fever, Monkey Pox, and other epidemics.
2. Global practices and medical waste management trend on COVID-19
The World Health Organization (WHO) pronounced the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), otherwise called COVID-19, a Public Health Emergency of International Concern—PHEIC in January 2020 and a pandemic in March 2020. COVID-19 is plaguing the world, and approximately a year after its pandemic status, there have been 233,503,524 confirmed cases of COVID-19, with 4,777,503 deaths resulting in a case fatality of 2.0 as of 1 October 2021(WHO, Citation2021). With over 1800% increase in less than a year, the total number of infected persons has risen from 5 million in March 2020, 22 million in August 2020, 95 million in January 2021 to over 234 million in October 2021 and increasing, which seems not to get its peak at this current stage (Van Fan et al., Citation2021; WHO, Citation2021). At this current phase of the pandemic, there are numerous challenges to managing medical waste, particularly regarding the generation, collection, and haphazard disposal of COVID-related waste, as highlighted in . The impacts include a change in waste volume (Ikiz et al., Citation2021), composition, handling, and treatment methods (Das et al., Citation2021; Van Fan et al., Citation2021). Other studies have highlighted the rise in plastic and food wastes during the pandemic (Behera, Citation2021; Hantoko et al., Citation2021). Due to this, waste treatment and disposal facilities are under immense pressure to ramp up processing capacity (Hantoko et al., Citation2021) and final disposal. We are now faced with the difficult task of eradicating COVID-19 in order to limit its spread while also preventing environmental risks and hazards to human health, including those of health and waste workers (Makoto et al., Citation2020).
During the COVID-19 pandemic, a surge in medical waste is seen across different nations, as presented in (Behera, Citation2021; Hantoko et al., Citation2021; Haque et al., Citation2021). In developing countries, the volume of medical waste increases exponentially due to enhanced access to medicare, single-use of medical supplies, and a growing population that aids more people access to technological advancement in medical care. These developments are the foremost causes of COVID-related waste in the United States. Medical waste is highly regulated in the US (Windfeld & Brooks, Citation2015). As the world’s largest producer of medical waste, the United States produces more than 3.5 million tonnes/year of medical waste (Lee et al., Citation2004), growing to over 6 million tonnes annually (Laura, Citation2020; Zamparas et al., Citation2019). The Occupational Health and Safety Administration (OSHA) has the duty to enact and regulate legislation regarding MWM in the US after it was substituted for the Medical Waste Tracking Act (MWTA) of 1988 (OSHA, Citation1991). OSHA (Citation1991) defines regulated waste as contaminated sharps, potentially infectious materials contaminated with liquid or semi-liquid blood, items caked with dried blood, and pathological and microbiological wastes containing blood, it’s further classified as;
Fluids from the human body such as cerebrospinal fluid, vaginal secretions, peritoneal fluid, synovial fluid, semen, pericardial fluid, saliva in dental procedures, pleural fluid, amniotic fluid, body fluids visibly contaminated with blood, and all body fluids in circumstances where it is challenging or impossible to distinguish between body fluids
human tissues or organs asides intact skin (living or dead)
HBV and HIV containing other culture solutions; HIV containing organ, tissue, and cell culture, tissues, blood, and organs from infected animals with HBV or HIV from research study (OSHA, Citation1991).
Figure 3. Medical wastes produced during COVID-19 pandemic in tonnes/day (Behera, Citation2021; Hantoko et al., Citation2021; Haque et al., Citation2021).
OSHA guidelines on COVID-related medical waste require its handling and management as biomedical waste. Furthermore, it highlights that SARS CoV-2 contaminated municipal waste is treated as non-contaminated general waste. This roots serious health risks to waste workers as SARS CoV-2 is active on different surfaces and mediums for days. The life span of SARS CoV-2 in stool is reported to be 17–31 days (Kampf et al., Citation2020; Zheng et al., Citation2020). Therefore, there is a need to strengthen the management of stool-related waste mixed with municipal waste to prevent and control SARS CoV-2 spread (Behera, Citation2021). Medical waste disposed of in the incinerator is the most common disposal method in the US. This has led to a clamour for a regulation to prevent its nuisance either via gases emission or wastewater to nearby areas (Windfeld & Brooks, Citation2015). COVID medical waste can be treated effectively with an industrial furnace, MSW incinerator, or cement kiln for emergency disposals (Hantoko et al., Citation2021).
In Europe, few member states have specific healthcare waste regulations. The European directives serve as a fundamental framework for member nations to develop and enact their national waste management regulations and standards. Consequently, the European regulations take precedence over any domestic legislation and set standards for its member nations. An example is the Hazardous Waste Directive, which governs the legislative framework for waste management in generation, segregation, collection, transport, sorting, recovery, treatment, disposal, and waste classification (Woolridge & Hoboy, Citation2019). In Europe, there is a single categorization framework for all waste depending on the characteristics of the waste; this is called the European Waste Catalogue (EWC). In the catalogue, health care waste comes within Chapter 18 (Environmental Protection Agency, Citation2002). In COVID waste management, European Union has directed that personal protective equipment like face masks with suspected or confirmed COVID-19 be handled and discarded with care and by waste professionals through designated COVID-19 waste collectors’ facilities.
Italy has the challenge of medical waste segregation. 57% of medical waste was improperly disposed of in a study carried out in several operating theatres (Amariglio & Depaoli, Citation2020). The mix-up or inadequate segregation of infectious wastes from non-infectious renders the entire waste stream dangerous, hence, exposing healthcare workers to biochemical risks and increasing waste disposal costs (Amariglio & Depaoli, Citation2020; Sengodan, Citation2014). In the management of COVID-19 waste, Italian authorities have categorized the collection of home-generated COVID waste as T1, which is considered infectious and T2, classified to be municipal. The handling and management of COVID wastes are restricted from elderly persons. As obtained globally, the growing ageing population in the nation is susceptible to chronic diseases, as observed in the COVID-19 pandemic scenario (WHO, Citation2021), which has resulted in an increasing number of deaths.
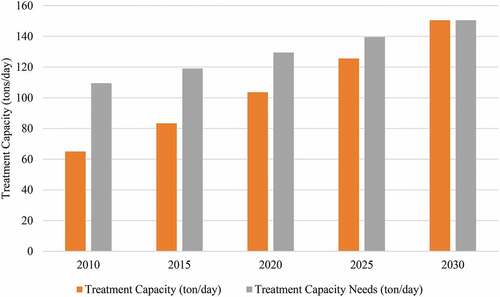
In Japan, the waste management practice is implemented according to the Waste Disposal and Public Cleansing Law of 1970 (Miyazaki & Une, Citation2005). In 1992, the country’s earliest law of infectious waste management was enacted. It defines infectious wastes as materials produced from medical facilities arising from the diagnosis, care, treatment, and research of illness capable of transmitting infectious diseases. Subsequently, a modified criterion for infectious waste management was instituted by Japan’s Ministry of Environment in 2004. In Japan, reducing infectious medical waste is attainable if segregation is categorized into the source of waste generation, the form of waste, and the type of infectious diseases (Miyazaki & Une, Citation2005). In Egypt, data from the Ministry of Health shows that the annual health care waste is about 371,776 kg/day, and the fraction of infectious waste is in the range of 25%—30% (Al Bazedi et al., Citation2013). Furthermore, a study by Abd El-Salam (Citation2010) in selected hospitals in El-Beheira Governorate showed that the quantity of medical waste produced was 1.249 tonnes/day. About 61.1% of waste was comparable to general or domestic waste estimated by WHO. The remainder portion (38.9%) was seen to be hazardous waste. The volume of waste was 1249 kg/day from the selected hospitals, and the average medical rate generation rate was 0.84 kg/bed/day. Research findings indicated poor segregation in the waste stream not according to applicable guidelines. For solid medical waste, incineration has become the most common form of treatment. It is growingly becoming unacceptable due to its linked environmental risks, but significant steps in properly managing infectious medical waste via on-site small–scale incinerators are reported (Al Bazedi et al., Citation2013). In China, it is estimated that the total MSW will grow from 159 MMT to 340 MMT by 2050 (Shapiro-Bengtsen et al., Citation2020). With the increase in treatment needs from health care facilities, as shown in , the challenge of released dioxins and gases from incineration becomes a concern to public health. Autoclaving is rarely used in some hospitals (Abdulla et al., Citation2008). For COVID-19 related wastes, incineration proves to be more effective because of its tremendous heat application. New treatment facilities are required if the projected treatment capacity increases beyond the existing capacity. Due to the abrupt emergence of the COVID-19 pandemic, treatment capacity is overwhelmed with medical wastes. For example, Wuhan utilized a cement kiln as an extra tool to treat medical wastes generated (Hantoko et al., Citation2021).
Figure 4. Projections of treatment capacity for an estimated population for 2010–2030 (Al Bazedi et al., Citation2013).
In Mauritius, access to the public health care system comes at no cost (Republic of Mauritius Ministry of Environment & National Development Unit, Citation2005). Hence, this is a causative factor in the high medical waste generation rate. The Ministry of Health and Quality of Life administers and regulate healthcare waste management practices in hospitals (Mohee, Citation2005). Mauritius is reported to have five regional hospitals which provide medical, surgical, and specialist services (Bokhoree et al., Citation2014). Various research has shown that the average amount of hazardous wastes per patient per day was found to be between 0.072–2 kg/bed (Bokhoree et al., Citation2014; Mohee, Citation2005). It further highlighted the amount of hazardous wastes incinerated per day ranges from 100–1050 kg (Bokhoree et al., Citation2014). This study further shows a good level of awareness of MWM in the private health sector of Mauritius than in the public hospitals (Bokhoree et al., Citation2014). Public hospitals experienced incessant dumping of hazardous medical wastes or burnt ash from the incinerator, contaminating groundwater. Research analysis revealed that the wastewater from medical facilities was polluted above permissible limits of its coliform content, chemical oxygen demand (COD), total suspended solids (TSS), and biological oxygen demand (BOD). As a threat to the environment, excessive heat from incinerators endangers plant and animal species, e.g., birds (Bokhoree et al., Citation2014; Mohee, Citation2005).
3. Medical waste management in Nigeria
The issue of waste management has significantly affected all sectors in Nigeria. In Nigeria, solid waste management has been a persisting challenge due to the ever-growing population (Etim, Babaremu et al., Citation2021; Omole & Isiorho, Citation2013). World Bank estimates that the Sub-Saharan Africa region generates approximately 174 million tonnes of waste per annum with prominent leaders from middle-income countries and tourist nations (Kaza et al., Citation2018). Studies in Nigeria have projected medical waste generation between 0.562–0.670 kg/bed/day with a peak rate of 1.68 kg/bed/day (Abah & Ohimain, Citation2011; Oli et al., Citation2016). Similarly, estimated rates of 0.631 kg/bed/day are for Lagos and Ikorodu metropolis (Ezechiel O. Longe, Citation2012). Like WHO’s categorization, all waste produced from any health care or medical facility in Nigeria is defined as Health Care Waste (HCW; National Environmental Standards and Regulations Enforcement Agency, Citation2009). There are 10 classifications of medical waste in Nigeria, which includes; general solid waste, infectious waste, heavy metals waste, genotoxic waste, microorganisms, pathological waste, pressurized containers, sharps, chemical waste, and pharmaceutical waste. The National Environmental Standards and Regulations Enforcement Agency (NESREA) assumes the regulation and classification of all medical wastes in Nigeria. The classification of these wastes does not entail its management from source to sink as there is no legislative monitoring or assessment compliance by health facilities within the country. Hence, Nigeria’s current position and classification of medical waste varies greatly among its regulatory agencies. This has resulted in inadequate monitoring, lack of strict compliance and disparate disposal activities by medical facilities. As of today, there is no legal framework or legislation on MWM in Nigeria. However, through its collaboration with other public health agencies, the Federal Ministry of Health has provided the following documents on health care waste management; National Healthcare Waste Management Guidelines, National Healthcare Waste Management Policy, and the National Healthcare Waste Management Plan (Federal Ministry of Health, Citation2018). Categories of Medical Waste in Nigeria is presented in .
Table 1. Categories of medical waste in Nigeria (National Environmental Standards and Regulations Enforcement Agency, Citation2009)
NESREA defines Health Care Waste (HCW) as waste
produced during the diagnosis, immunization or treatment of humans and animals, during medical research activities or in the manufacture or testing of biological experiments
produced in health and medical facilities (outpatient departments, pharmacies, hospitals, dental clinics, patent medical shops, dispensaries, veterinary stations, polyclinics, etc.), or materials contaminated during the diagnosis, treatment, and disease prevention in humans and animals.
For developing nations like Nigeria, the challenge of good health care and infrastructure are unyielding. Little priority and less urgency are directed to healthcare waste management (Abah & Ohimain, Citation2011). Regrettably, technical and realistic information on healthcare waste management is inadequate, and the study on public health consequences is insufficient and constraint in scope (Chuks et al., Citation2013). Although there are some accurate reports on the amount and nature of healthcare waste generated and the management strategies deployed for proper disposal, it is estimated that several hundred tons of unrecorded healthcare waste have been disposed of in open dumps and pits. Therefore, in many developing nations around the world, MWM remains an issue (Al Bazedi et al., Citation2013; Cheng et al., Citation2010; Mohee, Citation2005). In past years, there has been an almost complete lack of institutional structure and arrangements for health care facilities and their waste in Nigeria (Chuks et al., Citation2013). In recent times, relevant agencies have made a significant effort in this sense, as proper documentation of hospitals and clinics is now available in Nigeria (Federal Ministry of Health, Citation2021). highlights the heatmap distribution of all registered hospitals and clinics across Nigeria. With the proper institutional structure and operation, centralized management of all generated waste within these hospitals is achievable.
Figure 5. Distribution of hospitals and clinics in Nigeria (Federal Ministry of Health, Citation2021).

Generally, diverse techniques are used to assess, examine and quantify medical waste. Such methods include modelling, questionnaire administration, interviews, observation, characterization and quantification (Amariglio & Depaoli, Citation2020; Hong et al., Citation2018; Longe, Citation2012; Makajic-Nikolic et al., Citation2016; Zhang et al., Citation2013). highlights the various studies, regulation adherence, failures, and gaps associated with the safe management of healthcare waste as obtainable in Nigeria. In Jos metropolis, an assessment conducted in six major hospitals showed below par in their healthcare waste management practices as measured with WHO’s guidelines and other regulatory agencies. Similarly, in Ikorodu and Lagos metropolis, a survey on 20 health care centres revealed the lack of appropriate treatment systems for health care wastes in most hospitals (Longe, Citation2012). Health workers stated inadequate funding, low level of awareness and lack of highly trained waste operators among healthcare workers as factors hindering effective waste management. Also, a study in Port-Harcourt ascertained the vital need for an effective waste management system and the pertinency for multi-sectoral collaboration in the health care sector in Nigeria (Stanley & Okpara, Citation2011). Hence, an understudy of the healthcare facilities’ modus operandi and its relation to effective and sustainable waste management practices within and outside the country could be the foremost realistic measure in executing a standard waste management policy (Ndidi et al., Citation2009). An appropriate waste management team should be set up to formulate strategies, plans, policies, documents, technical recommendations and best practices in handling healthcare waste (Ndidi et al., Citation2009). Segregation of medical waste has been highlighted to aid effective MWM (WHO, Citation2005), but several medical facilities in Nigeria has flawed this viewpoint. Bassey et al. assessed five hospitals in Abuja through an observational study and highlighted segregation of waste to be zero in all selected hospitals (Bassey et al., Citation2006). A similar analysis conducted in Jos and Lagos Metropolis highlighted waste segregation as zero in all hospitals (Ndidi et al., Citation2009) and 3 out of 4 hospitals practising segregation, respectively (Longe & Williams, Citation2006). A pilot study of MWM in Lagos metropolis indicates a high priority for segregating hazardous waste streams (Longe & Williams, Citation2006), but the awareness for proper colour coding and classification remains very low in most reviewed studies.
Table 2. Examples of MWM evaluation in Nigeria
For instance, most surveyed hospitals from a study in Port Harcourt do not characterize and segregate wastes into coloured or marked bins for each waste stream and fail to document waste generation and disposal (Ogbonna, Citation2011). As a pace to successful segregation within Lagos metropolis, the Lagos State Waste Management Authority (LAWMA) in 2008 disbursed waste disposal supplies to over 500 medical facilities in the state, which includes 6000 injection safety boxes for sharps and syringes, 9000 red-coloured bags for the collection of highly infectious waste, 3000 brown-coloured bags for pharmaceutical and chemical wastes, 8000 yellow-coloured bags for infectious waste materials, yellow-coloured bags with radioactive labels are for any liquid or solid pathological wastes contaminated with radioactive isotopes of any kind (Longe, Citation2012). But the question today is, what roles do government agencies play in an active MWM system? One of the advantages of waste labelling and segregation is identifying waste sources, type and nature of waste, quantity generated and the back-trace of infection that may arise (Chartier et al., Citation2014). An easy solution is to apply a label to each waste container with a description of the source area, time and date of closure of the container, and the name of the person who fills the label. It is also advisable to use a global or local-based regulation hazard symbol on each waste container. The practice of burning medical waste is predominately common in Nigeria (Longe & Williams, Citation2006). Another common tradition is the disposal of the placenta from a newborn baby. The placenta is widely trusted to be given to the parents for disposal for fear of not losing their child’s destiny (Bazuaye & Enabudoso, Citation2011). The disposal is either by burning, burying, or even eating it (ICRC, Citation2011). For most hospitals, a routine tradition is to dispose of hazardous or infectious regulated waste types into a fallow land within the health facility premises (Longe & Williams, Citation2006).
4. Effect of COVID-19 on medical waste management in Nigeria
The spread of COVID-19 is over 200 nations and territories with 233,503,524 confirmed cases and 4,777,503 deaths globally as of 1 October 2021(WHO, Citation2021). There had been 204,459 confirmed cases for Nigeria, with 2,677 deaths resulting in a case fatality rate (CFR) of 1.3% as of 26 September 2021 (NCDC, Citation2021a). The pandemic has influenced human activity, particularly the health, environmental, social, educational, economic, and tourism sectors. Severe Acute Respiratory Syndrome Coronavirus 2, often denoted as SARS-CoV-2 or COVID-19, is a highly contagious single-stranded RNA virus enveloped and zoonotic in origin. They are responsible for causing flu-like symptoms, which often lead to diarrhoea, severe acute respiratory symptoms (SARS), sore throat, loss of taste or smell, and high mortality and morbidity (Ejeh et al., Citation2020; Rothan & Byrareddy, Citation2020). Given the basis of its microstructure and host matter, SARS-CoV-2 has different lifespans. In the air, the virus has a 3-hours lifespan as part of aerosols, 4 hours on copper surfaces, 24 hours on paper currency and cardboards, and 2–4 days on sewage, plastics, stainless materials, and solid faeces (Oyedotun et al., Citation2020; Van Doremalen et al., Citation2020; Ye et al., Citation2016). The spread of COVID-19 is facilitated by the longer lifespan of SARS-CoV-2 on sewage and waste materials, which makes its control of tremendous concerns to public health considering how fragile our waste management stream is.
In the last decade, Nigeria has recorded epidemics of several deadly diseases such as the Ebola outbreak in 2014, Monkeypox in 2017, Yellow fever in 2017, Lassa fever in 2018, Acute hepatitis E, Cholera, Meningococcal disease, and COVID-19 in 2019 (WHO, Citation2020a). Hence, the country seems to experience a proliferation in the amount of waste produced from the healthcare industries with respect to diagnosis, care, and treatment of affected patients. The volume of medical waste produced in various hospitals is comparable to the average generation rate per bed and infected persons. An estimation from WHO shows the generation rate of medical waste in Nigeria as 2.43kg/bed/day (Federal Government of Nigeria, Citation2013). The approximation of medical waste in tons/day is provided and analyzed as follow (Oyedotun et al., Citation2020);
where:
MWGR = Medical Waste Generation Rate, 2.43 kg/bed/day
MW = Medical Waste (tons/day)
The country’s rate of medical waste has increased from 131.24 tons/day in August 2020 to approximately 318.92 tons/day in January 2021 during the COVID-19 pandemic (Oyedotun et al., Citation2020). Undoubtedly, this waste increase is due to the increasing infection rate. For example, China’s COVID-19 epicentre, Wuhan, experienced a considerable rise in medical waste from 40–50 tonnes/day prior to the epidemic to approximately 247 tonnes on 1 March 2020. In the light of the COVID-19 pandemic, a more significant than usual percentage of medical waste is attributable to hospital diagnosis and patients’ treatment.
Another crucial concern of MWM in Nigeria during the COVID-19 pandemic is the significant use of disposable PPE such as face masks, gloves, and face shields. In January 2021, the Nigerian government signed into law the COVID-19 Health Protection Regulations Policy ensuing the mandatory usage of face masks in public places. As a result of this regulation and enforcement, millions of potentially hazardous face masks are disposed of indiscriminately every day. Frontline health workers and waste handlers use PPE daily to treat, handle, and manage COVID-19 cases. Previous research estimates that 129 billion facemasks are required monthly for COVID-19 containment (Prata et al., Citation2020). With a population of 206 million, the total daily estimated PPE used in Nigeria is 171,908,091 as obtainable in Equationequation 2(2)
(2) (Nzediegwu & Chang, Citation2020);
A large amount of discarded PPE that could be infected with respiratory contaminants ends up as waste, posing significant environmental and health risks (Nzediegwu & Chang, Citation2020; Oyedotun et al., Citation2020). A study carried out in Nigeria and Guyana suggested the possibilities of viral transmission from animals exposed to COVID-19 waste to humans. The study showed visuals of household pets such as dogs, cats, and hens in landfills with contaminated PPE and wastes. Hence, there is a need for strong legislation on waste disposal and animal control (Oyedotun et al., Citation2020). For countries and international agencies, the COVID-19 pandemic has instituted new regulations and guidelines in managing associated wastes from the care and treatment of COVID-19 patients. summarises waste management guidelines during the COVID-19 pandemic by different organizations and countries.
Table 3. Waste management guidelines during the COVID-19 pandemic by different organizations and countries
Nigeria’s healthcare infrastructure has been under tremendous pressure since the outbreak of COVID-19, Ebola and Lassa fever (Oruonye & Ahmed, Citation2020). For instance, during the COVID Pandemic, established national health systems in Nigeria could not adequately adapt to the increasing needs of diagnosed patients requiring treatment for SARS–COV–2 and acute respiratory diseases in intensive care units (ICU; Ohia et al., Citation2020); as a result, there was a creation of additional isolation centres around the country (Federal Ministry of Health, Citation2020; Government of Akwa Ibom State, Citation2020; Lagos State Government Ministry of Health, Citation2020). In Nigeria, measures were directed at establishing testing laboratories, isolation centres, and treatment facilities to curb coronavirus outbreaks. There are little or no much-said protocols in the safe handling and disposal of waste produced from the management and treatment of COVID-19 (Oruonye & Ahmed, Citation2020). While reported cases may be increasing minimally compared to other regions, Africa is estimated to be severely affected by the pandemic. For Nigeria, this has significant repercussions, particularly in light of the rising number of infected cases that need critical care. In Africa, the supply of isolation facilities and the accessibility of diagnostic sets for quick and accurate diagnosis may also be a problem (Ohia et al., Citation2020). This virus can be present in a person with little to no symptoms, causing it to spread vastly. For instance, the index case in Nigeria from an Italian was only detected 48 hours later after entering the country (NCDC, Citation2021b). The advent of COVID-19 has proved the need for a more proactive, resilient, and sustainable health structure in Nigeria. This is seen in the number of diagnostic centres in the country before the index case. Nigeria had only four laboratories that could diagnose COVID-19. Consequently, as of January 2021, the NCDC had created more than 70 public health laboratories and asserted the initiation of thirty-six private laboratories in the country (NCDC, Citation2021b). At least one public health laboratory for COVID-19 diagnosis is now available in every state in Nigeria. Indubitably, the creation of additional diagnostic centres would result in a higher generation of potentially infectious wastes, which is of great worry if not adequately managed. According to the NCDC, all medical wastes created during the treatment of patients with a confirmed or suspected case of COVID-19 should be deemed infectious and must be collected securely in clearly labeled containers. Thus, there is a need for facilities to be provided with the appropriate human and material infrastructures to handle, characterize and then properly dispose of its waste in order to achieve good health care waste management safely. The use of appropriate PPE such as long-sleeved gown, mask, goggles, face shield, heavy-duty gloves, and boots in the management and transportation of infectious healthcare waste is crucial to a waste manager. The emergence of the COVID-19 pandemic has further led to the introduction of a new healthcare waste management law in Ogun State, Nigeria. The new law approach aims to end poor handling of healthcare wastes that harbour diseases, thus posing risks to health professionals, patients, and the general public. Pressure from the menace of medical wastes produced from the diagnosis and treatment of COVID-related cases gave the urgency for the enactment. Additionally, the new healthcare waste management law will provide training prospects for health workers by the Ogun State Waste Management Authority (OGWAMA; Ogun State Government Ministry of Environment, Citation2020).
5. Conclusion
This paper provides an understanding of the inadequacies of a fragile MWM system, especially in a Pandemic. Based on this review, a more inclusive and comprehensive strategy for a pandemic waste management plan is required in Nigeria. The challenge of an effective MWM System in Nigeria is linked to poor or inadequate understanding of the waste management processes amongst health care workers and waste handlers. Since MWM is a cycle of ordered processes originating from source production, waste generation, segregation and labelling, collection, storage, transportation, recovery, reuse, recycling, treatment, and final disposal, it is pertinent that each process is handled effectively and efficiently. The interwovenness of these processes makes “a flaw in one—a flaw in all.” Despite various governmental, regulatory, private, and public stakeholders’ efforts, a lot of targeted actions need to be done to strengthen existing policies on MWM. Furthermore, the advent of COVID-19 has developed an interest in understanding the interrelations between MWM and pandemics. Hence, additional research findings are required to strengthen environmental epidemiology following COVID-19 and other related epidemics (Ebola, Lassa Fever, Monkey Pox, etc.) in Nigeria as it affects waste management. Therefore, to eliminate waste management problems and SARS–COV–2 spread, a joint effort is needed from the government, communal and private agencies, healthcare institutions, and the general populace, with the majority of the populace showing readiness to cooperate with policies designed to enhance waste management structures in Nigeria.
Additional information
No additional information is available for this paper.
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Highlights
A review of COVID-19 impact on medical waste management practices.
Estimation of discarded PPE (facemasks) during the COVID-19 pandemic.
Health workers and waste handlers are at high risk of COVID-19 infection.
Increase in the volume of medical waste prior to COVID-19 pandemic.
Acknowledgements
The authors appreciate the Chancellor and Management of Covenant University for supporting the article publication charge and making this medium available for research publications.
Data availability statement
No available data .
Disclosure statement
The authors hereby declare that there are no relevant financial or non-financial competing interests to report.
Additional information
Funding
Notes on contributors
Mmemek-Abasi Etim
Mmemek-Abasi Etim is a graduate of Water Resources and Environmental Engineering, Civil Engineering at Covenant University.
His research interests include public health, environmental pollution and health risks (air, water, noise), risk assessment, quantitative and qualitative methods, waste management and decision-making techniques, environmental epidemiology and community-based research for policy implementation.
His previous research includes Health Risk and Environmental Assessment of Cement Production in Nigeria and Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria.
References
- Abah, S. O., & Ohimain, E. I. (2011). Healthcare waste management in Nigeria: A case study. Journal of Public Health and Epidemiology, 3(3), 99–27. https://academicjournals.org/journal/JPHE/article-full-text-pdf/D86D4ED1148.pdf
- Abd El-Salam, M. M. (2010). Hospital waste management in El-Beheira governorate, Egypt. Journal of Environmental Management, 91(3), 618–629. https://doi.org/10.1016/j.jenvman.2009.08.012
- Abdulla, F., Abu Qdais, H., & Rabi, A. (2008). Site investigation on medical waste management practices in northern Jordan. Waste Management, 28(2), 450–458. https://doi.org/10.1016/j.wasman.2007.02.035
- Agamuthu, P., & Barasarathi, J. (2020). Clinical waste management under COVID-19 scenario in Malaysia. Waste Management and Research 39 1_suppl 18–26 . https://doi.org/10.1177/0734242X20959701
- Al Bazedi, G., Shouman, E., Sorour, M. H., & Abulnour, A. G. (2013). Management of hazardous medical waste treatment in Egypt. World Applied Sciences Journal, 28(6), 804–808. https://doi.org/10.5829/idosi.wasj.2013.28.06.13847
- Amariglio, A., & Depaoli, D. (2020). Waste management in an Italian Hospital’s operating theatres: An observational study. American Journal of Infection Control, 49(2), 184–187. https://doi.org/10.1016/j.ajic.2020.07.013
- Asian Development Bank. (2020). Managine Infectious Medical Waste during the COVID-19 Pandemic. https://www.adb.org/publications/managing-medical-waste-covid19
- Aung, T. S., Luan, S., & Xu, Q. (2019). Application of multi-criteria-decision approach for the analysis of medical waste management systems in Myanmar. Journal of Cleaner Production, 222, 733–745. https://doi.org/10.1016/j.jclepro.2019.03.049
- Bassey, B. E., Benka-Coker, M. O., & Aluyi, H. S. A. (2006). Characterization and management of solid medical wastes in the Federal Capital Territory, Abuja Nigeria. African Health Sciences, 6(1 58–63). https://www.ajol.info/index.php/ahs/article/view/6927
- Bazuaye, G., & Enabudoso, E. (2011). Willingness of pregnant women in Benin city Nigeria to donate placenta cord blood for stem cell transplantation. Annals of Biomedical Sciences, 10(1). https://doi.org/10.4314/abs.v10i1.69202
- Behera, B. C. (2021). Challenges in handling COVID-19 waste and its management mechanism: A review. Environmental Nanotechnology, Monitoring & Management, 15, 100432. https://doi.org/10.1016/j.enmm.2021.100432
- Bokhoree, C., Beeharry, Y., Makoondlall-Chadee, T., Doobah, T., & Soomary, N. (2014). Assessment of environmental and health risks associated with the management of medical waste in mauritius. APCBEE Procedia, 9, 36–41. https://doi.org/10.1016/j.apcbee.2014.01.007
- Chartier, Y., Emmanuel, J., Pieper, U., Prüss, A., Rushbrook, P., Stringer, R., Townend, W., Wilburn, S., & Zghondi, R. (2014). Safe management of wastes from health-care activities Second edition. https://www.uab.cat/doc/wastes_healthcare_activities_bioseguretat_OMA
- Cheng, Y. W., Li, K. C., & Sung, F. C. (2010). Medical waste generation in selected clinical facilities in Taiwan. Waste Management, 30(8–9), 1690–1695. https://doi.org/10.1016/j.wasman.2010.04.006
- Chuks, N., Anayo, F., & Ugbogu, O. C. (2013). Health care waste management – Public health benefits, and the need for effective environmental regulatory surveillance in federal republic of Nigeria. Current Topics in Public Health, InTech. https://doi.org/10.5772/53196
- Coker, A., Sangodoyin, A., Sridhar, M., Booth, C., Olomolaiye, P., & Hammond, F. (2009). Medical waste management in Ibadan, Nigeria: Obstacles and prospects. Waste Management, 29(2), 804–811. https://doi.org/10.1016/j.wasman.2008.06.040
- Das, A. K., Islam, M. N., Billah, M. M., & Sarker, A. (2021). COVID-19 pandemic and healthcare solid waste management strategy – A mini-review. Science of the Total Environment, 778, 146220. https://doi.org/10.1016/j.scitotenv.2021.146220
- DEFRA. (2020). Guidance on prioritising waste collection services during coronavirus (COVID-19) pandemic - GOV.UK. https://www.gov.uk/government/publications/coronavirus-covid-19-advice-to-local-authorities-on-prioritising-waste-collections/guidance-on-prioritising-waste-collection-services-during-coronavirus-covid-19-pandemic
- Ejeh, F. E., Saidu, A. S., Owoicho, S., Maurice, N. A., Jauro, S., Madukaji, L., & Okon, K. O. (2020). Knowledge, attitude, and practice among healthcare workers towards COVID-19 outbreak in Nigeria. Heliyon, 6(11), e05557. https://doi.org/10.1016/j.heliyon.2020.e05557
- Environmental Protection Agency. (2002). EUROPEAN WASTE CATALOGUE AND HAZARDOUS WASTE LIST VALID FROM JANUARY 1 2002. http://www.epa.ie
- Etim, M.-A., Academe, S., Emenike, P., & Omole, D. (2021). Application of multi-criteria decision approach in the assessment of medical waste management systems in Nigeria. Sustainability, 13(19), 10914. https://doi.org/10.3390/su131910914
- Etim, M.-A., Babaremu, K., Lazarus, J., & Omole, D. (2021). Health risk and environmental assessment of cement production in Nigeria. Atmosphere, 12(9), 1111. https://doi.org/10.3390/atmos12091111
- Faiza, I. (2019, October 6). Medical waste being dumped around Abbasi Shaheed Hospital in Karachi - Pakistan - DAWN.COM. https://www.dawn.com/news/1503723
- Federal Government of Nigeria. (2013). National Healthcare Waste Management Guideline. https://doi.org/documents.worldbank.org/curated/en/164291468110649200/E16340NHCWMP10Sophie0version0170April.doc
- Federal Ministry of Health. (2018). HEALTH CARE WASTE MANAGEMENT PLAN (HCWMP) FOR NIGERIAN POLIO ERADICATION SUPPORT PROJECT ADDITIONAL FINANCING 3 DRAFT REPORT. https://documents1.worldbank.org/curated/pt/448401525781824503/text/Health-care-waste-management-plan.txt
- Federal Ministry of Health. (2020). Dr. Osagie Ehanire Inspects Thisday Dome Isolation Centre. https://www.health.gov.ng/index.php?option=com_k2&view=item&id=657:dr-osagie-ehanire-inspects-thisday-dome-isolation-centre&Itemid=470
- Federal Ministry of Health. (2021). Nigeria Health Facility Registry. https://hfr.health.gov.ng/
- Garba, H. S., & Zagga, A. D. (2007). Survey of the health facilities available for handling cases of tuberculosis in the rural areas around Sokoto metropolis. Trends in Medical Research, 2(4), 199–203. https://doi.org/10.3923/tmr.2007.199.203
- Government of Akwa Ibom State. (2020). Commissioning Of State-Of-The-Art 300 Bed Space Isolation Center At Methodist General Hospital, Ituk Mbang, Uruan, LGA | Akwa Ibom State Government. https://akwaibomstate.gov.ng/commissioning-of-state-of-the-art-300-bed-space-isolation-center-at-methodist-general-hospital-ituk-mbang-uruan-lga/
- Hantoko, D., Li, X., Pariatamby, A., Yoshikawa, K., Horttanainen, M., & Yan, M. (2021). Challenges and practices on waste management and disposal during COVID-19 pandemic. Journal of Environmental Management, 286, 112140. https://doi.org/10.1016/j.jenvman.2021.112140
- Haque, M. S., Uddin, S., Sayem, S. M., & Mohib, K. M. (2021). Coronavirus disease 2019 (COVID-19) induced waste scenario: A short overview. Journal of Environmental Chemical Engineering, 9(1), 104660. https://doi.org/10.1016/j.jece.2020.104660
- Hong, J., Zhan, S., Yu, Z., Hong, J., & Qi, C. (2018). Life-cycle environmental and economic assessment of medical waste treatment. Journal of Cleaner Production, 174, 65–73. https://doi.org/10.1016/j.jclepro.2017.10.206
- ICRC. (2011). MEDICAL WASTE MANAGEMENT. https://www.icrc.org/en/doc/assets/files/publications/icrc-002-4032.pdf
- Ikiz, E., Maclaren, V. W., Alfred, E., & Sivanesan, S. (2021). Impact of COVID-19 on household waste flows, diversion and reuse: The case of multi-residential buildings in Toronto, Canada. Resources, Conservation and Recycling, 164, 105111. https://doi.org/10.1016/j.resconrec.2020.105111
- Insa, E., Zamorano, M., & López, R. (2010). Critical review of medical waste legislation in Spain. Resources, Conservation and Recycling, 54(12), 1048–1059. Elsevier B.V. https://doi.org/10.1016/j.resconrec.2010.06.005
- Jang, Y. C. (2019). Infectious/medical/hospital waste: General characteristics. In Encyclopedia of environmental health (pp. 661–665). Elsevier.https://doi.org/10.1016/B978-0-444-63951-6.00508-8
- Kampf, G., Todt, D., Pfaender, S., & Steinmann, E. (2020). Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection, 104(3), 246–251. https://doi.org/10.1016/j.jhin.2020.01.022
- Kaza, S., Yao, L. C., Bhada-Tata, P., & Van Woerden, F. (2018). What a waste 2.0: A global snapshot of solid waste management to 2050. In What a waste 2.0: A global snapshot of solid waste management to 2050. https://doi.org/10.1596/978-1-4648-1329-0
- Lagos State Government Ministry of Health. (2020). LAGOS TO BUILD INTERNATIONAL INFECTIOUS DISEASE RESEARCH CENTRE AT YABA – SANWO-OLU – Ministry of Health. https://health.lagosstate.gov.ng/2020/06/29/lagos-to-build-international-infectious-disease-research-centre-at-yaba-sanwo-olu/
- Laura, W. (2020). United States Market for Medical Waste Management 2020-2027: Market Landscape, Dynamics and Competitive Landscape. ResearchAndMarkets. https://www.prnewswire.com/news-releases/united-states-market-for-medical-waste-management-2020-2027-market-landscape-dynamics-and-competitive-landscape-301067806.html
- Lee, B. K., Ellenbecker, M. J., & Moure-Ersaso, R. (2004). Alternatives for treatment and disposal cost reduction of regulated medical wastes. Waste Management, 24(2), 143–151. https://doi.org/10.1016/j.wasman.2003.10.008
- Longe, E. O. (2012). Healthcare waste management status in Lagos State, Nigeria: A case study from selected healthcare facilities in Ikorodu and Lagos metropolis. Waste Management and Research, 30(6), 562–571. https://doi.org/10.1177/0734242X11412109
- Longe, E. O., & Williams, A. (2006). A preliminary study of medical waste management in Lagos metropolis, Nigeria. Journal of Environmental Health Science & Engineering, 3(2). https://ijehse.tums.ac.ir/index.php/jehse/article/view/82
- Makajic-Nikolic, D., Petrovic, N., Belic, A., Rokvic, M., Radakovic, J. A., & Tubic, V. (2016). The fault tree analysis of infectious medical waste management. Journal of Cleaner Production, 113, 365–373. https://doi.org/10.1016/j.jclepro.2015.11.022
- Makoto, T., Premakumara, J. D. G., Isnanto, S. Y. P., Kazunobu, O., Keith, A., Shunichi, H., Daniel, T., Misato, D., Junko, F., & Dyota, C. (2020). Waste Management during the COVID-19 Pandemic Title: Waste Management during the COVID-19 Pandemic From Response to Recovery. United Nations Environment Programme. www.un.org/Depts/Cartographic/english/htmain.htm
- MEE. (2020). Guidelines for Emergency Management and Technical Management of Medical Waste in the Outbreak of Pneumonia with New Coronavirus Infection (Trial). http://www.gov.cn/xinwen/2020-01/29/content_5472997.htm
- Miyazaki, M., & Une, H. (2005). Infectious waste management in Japan: A revised regulation and a management process in medical institutions. Waste Management, 25( 6 SPEC. ISSuppl.), 616–621. https://doi.org/10.1016/j.wasman.2005.01.003
- Mohee, R. (2005). Medical wastes characterisation in healthcare institutions in Mauritius. Waste Management, 25( 6 SPEC. ISSuppl.), 575–581. https://doi.org/10.1016/j.wasman.2004.10.003
- National Environmental Standards and Regulations Enforcement Agency. (2009). National Environmental (Sanitation and Wastes Control) Regulations 2009. https://www.nesrea.gov.ng/wp-content/uploads/2020/02/Sanitation_and_Wastes_Control_Regulations-2009.pdf
- NCDC. (2020). NCDC Coronavirus COVID-19 Guidelines. https://covid19.ncdc.gov.ng/guideline/
- NCDC. (2021a). NCDC Coronavirus COVID-19 Microsite. https://covid19.ncdc.gov.ng/
- NCDC. (2021b). One Year After: Nigeria’s COVID-19 Public Health Response. https://covid19.ncdc.gov.ng/media/files/COVIDResponseMarch1.pdf
- Ndidi, N., Nelson, O., Patricia, O., & Sunday, J. A. (2009). Waste management in healthcare establishments within Jos Metropolis, Nigeria. African Journal of Environmental Science and Technology, 3(12), 459–465. https://doi.org/10.5897/AJEST09.119
- Ngouakam, H., Umo Aniekan, U., & Onojeta, A. F. (2010). Management of solid clinical wastes in some hospitals in Akwa Ibom state, Nigeria. International Journal of Natural and Applied Sciences. https://www.ajol.info/index.php/ijonas/article/view/76818
- Nzediegwu, C., & Chang, S. X. (2020). Improper solid waste management increases potential for COVID-19 spread in developing countries. Resources, Conservation and Recycling, 161, 104947. https://doi.org/10.1016/j.resconrec.2020.104947
- Ochonma, O. G., & Nwatu, S. I. (2018). Assessing the predictors for training in management amongst hospital managers and chief executive officers: A cross-sectional study of hospitals in Abuja, Nigeria. BMC Medical Education, 18(1), 138. https://doi.org/10.1186/s12909-018-1230-2
- Ogbonna, D. N. (2011). Characteristics and waste management practices of medical wastes in healthcare institutions in Port Harcourt, Nigeria. Journal of Soil Science and Environmental Management, 2(5), 132–141. http://www.academicjournals.org/JSSEM
- Ogun State Government Ministry of Environment. (2020). WASTE: OGUN MANDATES HEALTH FACILITIES TO ADOPT ENVIRONMENTAL-FRIENDLY MANAGEMENT.
- Ohia, C., Bakarey, A. S., & Ahmad, T. (2020). COVID-19 and Nigeria: Putting the realities in context. International Journal of Infectious Diseases, 95, 279–281. Elsevier B.V. https://doi.org/10.1016/j.ijid.2020.04.062
- Oke, I. A. (2008). Management of immunization solid wastes in Kano State, Nigeria. Waste Management, 28(12), 2512–2521. https://doi.org/10.1016/j.wasman.2007.11.008
- Oli, A. N., Ekejindu, C. C., Adje, D. U., Ezeobi, I., Ejiofor, O. S., Ibeh, C. C., & Ubajaka, C. F. (2016). Healthcare waste management in selected government and private hospitals in Southeast Nigeria. Asian Pacific Journal of Tropical Biomedicine, 6(1), 84–89. https://doi.org/10.1016/j.apjtb.2015.09.019
- Olukanni, D. O., Azuh, D. E., Toogun, T. O., & Okorie, U. E. (2014). Medical waste management practices among selected health-care facilities in Nigeria: A case study. 9(10), 431–439. https://doi.org/10.5897/SRE2014.5863
- Omole, D. O., & Isiorho, S. A. (2013). Municipal Solid Wastes And Water Quality Issues in Nigeria. https://gsa.confex.com/gsa/2013AM/webprogram/Paper225375.html
- Oruonye, E. D., & Ahmed, Y. A. (2020). Covid-19 and challenges of management of infectious medical waste in Nigeria: A case of Taraba State. https://doi.org/10.35248/2252-5211.20.10.381
- OSHA. (1991). 1910.1030 - Bloodborne pathogens. | Occupational Safety and Health Administration. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1030
- OSHA. (2020). COVID-19 - Control and Prevention | Occupational Safety and Health Administration. https://www.osha.gov/coronavirus/control-prevention#solidwaste
- Oteri, J., Bawa, S., Christopher, E., Nsubuga, P., Dieng, B., Braka, F., & Shuaib, F. (2021). Potential for improving routine immunisation waste management using measles vaccination campaign 2017 in Kebbi State, Nigeria. Vaccine, 39, C60–C65. https://doi.org/10.1016/j.vaccine.2020.12.060
- Oyedotun, T. D., Kasim, O. F., Famewo, A., Oyedotun, T. D., Moonsammy, S., Ally, N., & Renn-Moonsammy, D.-M. (2020). Municipal waste management in the era of COVID-19: Perceptions, practices, and potentials for research in developing countries. Research in Globalization, 2, 100033. https://doi.org/10.1016/j.resglo.2020.100033
- Prata, J. C., Silva, A. L. P., Walker, T. R., Duarte, A. C., & Rocha-Santos, T. (2020). COVID-19 pandemic repercussions on the use and management of plastics. Environmental Science & Technology, 54(13), 7760–7765. https://doi.org/10.1021/acs.est.0c02178
- Republic of Mauritius Ministry of Environment & National Development Unit. (2005). National Implementation Plan For The Stockholm Convention On Persistent Organic Pollutants | InforMEA. https://www.informea.org/en/action-plan/republic-mauritius-ministry-environment-national-development-unit-national-0
- Richter, A., Ng, K. T. W., Vu, H. L., & Kabir, G. (2021). Waste disposal characteristics and data variability in a mid-sized Canadian city during COVID-19. Waste Management, 122, 49–54. https://doi.org/10.1016/j.wasman.2021.01.004
- Rothan, H. A., & Byrareddy, S. N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity, 109, 102433. https://doi.org/10.1016/j.jaut.2020.102433
- Samuel Oyekale, A., & Oyekale, T. O. (2017). Healthcare waste management practices and safety indicators in Nigeria. BMC Public Health. https://doi.org/10.1186/s12889-017-4794-6
- Sengodan, V. C. (2014). Segregation of biomedical waste in an South Indian tertiary care hospital. Journal of Natural Science, Biology and Medicine, 5(2), 378–382. https://doi.org/10.4103/0976-9668.136194
- Shapiro-Bengtsen, S., Andersen, F. M., Münster, M., & Zou, L. (2020). Municipal solid waste available to the Chinese energy sector – Provincial projections to 2050. Waste Management, 112, 52–65. https://doi.org/10.1016/j.wasman.2020.05.014
- Si, Z. H., & Li, Y. (2020). Medical waste treatment in Wuhan from emergency to stability. http://www.xinhuanet.com/local/2020-04/01/c_1125796126.htm
- Sonne, C., You, S., & Ok, Y. S. (2020). Covid-19’s unsustainable waste management. In Science (Vol. 368, Issue 6498, p. 1438). American Association for the Advancement of Science. https://doi.org/10.1126/science.abc7778
- Stanley, H., & Okpara, K. (2011). Health care waste management in Port Harcourt Metropolis. American Journal of Scientific and Industrial Research, 2(5), 769–773. https://doi.org/10.5251/ajsir.2011.2.5.769.773
- Ugwu, E. I., Ekeleme, A. C., Okolie, S. T. A., Ibe, O. P., Chieke, C. F., Ibearugbulem, H. O., Omeje, M., Ede, A. N., Awoyera, P. O., & Ugwu, E. C. (2019). Characterization of medical wastes from selected hospitals in Umuahia, Nigeria. Journal of Physics: Conference Series. https://iopscience.iop.org/article/10.1088/1742-6596/1378/4/042058/pdf
- UN Department of Economic and Social Affairs. (2020). Impact of COVID-19 on SDG progress: a statistical perspective. https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-81-impact-of-covid-19-on-sdg-progress-a-statistical-perspective/
- UNICEF. (2021, August 19). What you need to know about the Delta variant. https://www.unicef.org/coronavirus/what-you-need-know-about-delta-variant
- United Nations. (2017). World population projected to reach 9.8 billion in 2050, and 11.2 billion in 2100. https://www.un.org/en/development/desa/population/events/pdf/other/21/21June_FINAL-PRESS-RELEASE_WPP17.pdf
- US EPA. (2020). Recycling and Sustainable Management of Food During the Coronavirus (COVID-19) Public Health Emergency | US EPA. https://www.epa.gov/coronavirus/recycling-and-sustainable-management-food-during-coronavirus-covid-19-public-health
- van Doremalen, N., Bushmaker, T., Morris, D. H., Holbrook, M. G., Gamble, A., Williamson, B. N., Tamin, A., Harcourt, J. L., Thornburg, N. J., Gerber, S. I., Lloyd-Smith, J. O., de Wit, E., & Munster, V. J. (2020). Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine, 382(16), 1564–1567. https://doi.org/10.1056/NEJMc2004973
- Van Fan, Y., Jiang, P., Hemzal, M., & Klemeš, J. J. (2021). An update of COVID-19 influence on waste management. Science of the Total Environment, 754, 142014. https://doi.org/10.1016/j.scitotenv.2020.142014
- WHO. (2005). Management of Solid Health-Care Waste at Primary Health-Care Centres - A Decision-Making Guide.
- WHO. (2018). Health-care waste. https://www.who.int/news-room/fact-sheets/detail/health-care-waste
- WHO. (2020a). Emergencies preparedness, response. In WHO. World Health Organization. http://www.who.int/csr/don/archive/country/nga/en/.
- WHO. (2020b). Water, sanitation, hygiene, and waste management for SARS-CoV-2, the virus that causes COVID-19. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-WASH-2020.4
- WHO. (2021). COVID-19: Occupational health and safety for health workers. https://www.who.int/publications/i/item/WHO-2019-nCoV-HCW_advice-2021.1
- WHO, & UNICEF. (2015). HEALTH CARE FACILITIES WASH in for better health care services. www.washinhcf.org
- Windfeld, E. S., & Brooks, M. S. L. (2015). Medical waste management - A review. Journal of Environmental Management, 163, 98–108. Academic Press. https://doi.org/10.1016/j.jenvman.2015.08.013
- Woolridge, A., & Hoboy, S. (2019). Medical waste. Waste, 517–530. Elsevier. https://doi.org/10.1016/B978-0-12-815060-3.00027-X
- World Health Organization. (2020). WHO Coronavirus Disease (COVID-19) Report. https://covid19.who.int/table
- Wormer, B. A., Augenstein, V. A., Carpenter, C. L., Burton, P. V., Yokeley, W. T., Prabhu, A. S., Harris, B., Norton, S., Klima, D. A., Lincourt, A. E., & Heniford, B. T. (2013). The green operating room: Simple changes to reduce cost and our carbon footprint. The American Surgeon, 79(7), 666–671. https://doi.org/10.1177/000313481307900708
- Ye, Y., Ellenberg, R. M., Graham, K. E., & Wigginton, K. R. (2016). Survivability, partitioning, and recovery of enveloped viruses in untreated municipal wastewater. Environmental Science and Technology, 50(10), 5077–5085. https://doi.org/10.1021/acs.est.6b00876
- Zamparas, M., Kapsalis, V. C., Kyriakopoulos, G. L., Aravossis, K. G., Kanteraki, A. E., Vantarakis, A., & Kalavrouziotis, I. K. (2019). Medical waste management and environmental assessment in the Rio University Hospital, Western Greece. Sustainable Chemistry and Pharmacy, 13, 100163. https://doi.org/10.1016/j.scp.2019.100163
- Zhang, H. J., Zhang, Y. H., Wang, Y., Yang, Y. H., Zhang, J., Wang, Y. L., & Wang, J. L. (2013). Investigation of medical waste management in Gansu province, China. Waste Management and Research, 31(6), 655–659. https://doi.org/10.1177/0734242X13482161
- Zheng, S., Fan, J., Yu, F., Feng, B., Lou, B., Zou, Q., Xie, G., Lin, S., Wang, R., Yang, X., Chen, W., Wang, Q., Zhang, D., Liu, Y., Gong, R., Ma, Z., Lu, S., Xiao, Y., Gu, Y., … Liang, T. (2020). Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: Retrospective cohort study. The BMJ, 369. https://doi.org/10.1136/bmj.m1443