Abstract
Dexterity is the coordination of hands and fingers with the eyes. Existing unilateral movements and dexterity tests use wearable devices for recording hand assessment. It is understandable that whenever some wired devices tag hands, the patient tends to be more conscious, which may not reflect the actual outcome. In this paper, using the finger-tap counter and loop-wire test, an attempt is made to evaluate unilateral movements and dexterity in adults of different age groups without using any wearable device. The test timings are recorded automatically with the help of the ATmega328p microcontroller and transferred to the clinician wirelessly via Bluetooth communication. Healthy 30 subjects between the age range (20–35, 36–50, 51–65, 66–80) were tested for finger-tap counter and loop-wire tests. The experiment is also tested for dominant and non-dominant hands for the same subjects. In this experiment, the result shows as the age increases, the trend in the assessment completion time and number of failures during the performance of the test increases. Female groups can perform both tests quicker than male groups with fewer errors irrespective of age group.
PUBLIC INTEREST STATEMENT
Loop & wire and Finger-tap counter tests are used to evaluate the human hand’s dexterity (fine motor and gross motor). In this study, we developed and standardized an indigenous, sensor-based automated test version. The test setup consists of Arduino Uno (ATmega328P microcontroller), HC-05 Bluetooth module, pushbuttons, piezo buzzer, clip handle, metal lock, and LED. The quantitative parameters, such as the number of failures and time (in seconds) required to complete Loop and Wire test for dominant and non-dominant hands, are captured and displayed. This work also calculates subject response time using the Finger-tap counter test. The developed device is tested with thirty healthy participants in the age range of 20–80 years. Assessment is made foolproof by avoiding stopwatch usage and reducing clinician supervision time.
1. Introduction
The human hand has various roles to play in day-to-day activities. Hands are used to express feelings, emotions, and love, communicate through sign language and gestures, self-defend and take care of others, maintain body temperature, and many more. In the present scenario, researchers and clinicians lack consensus on what functional measures should include in the hand evaluation. Some of the functional capabilities that can be evaluated in the Hand Function Test (HFT) are grip, coordination, pinch, range of motion, strength, and sensation test, as shown in . Activities of Daily Living (ADL) are tasks that mimic day-to-day activities and are included in the tests. The basic requirement of clinical evaluation techniques is that they should be relevant to a particular function test and reliable.
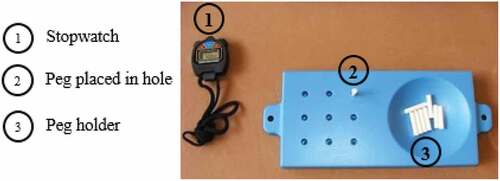
Dexterity is one component in the HFT and is commonly defined as skill and ease in using the hands. In dexterity tests, subjects perform various practical tasks such as pouring water into a glass, tying shoelaces, etc., related to Activity of Daily Living (ADL). Fine dexterity and gross dexterity are the two main types in it. Fine dexterity is the ability to make rapid, skillful, controlled, manipulative movements of small objects in which the fingers are primarily involved. shows the classic example for a fine motor test using the commercially available Nine Hole Pegboard Test (NHPT).
Gross dexterity can make skillful, controlled arm-hand manipulations of larger objects under speed conditions. Dexterity tests are essential for evaluating neurological diseases, checking work efficiency, comparing an individual’s right and left-hand performance, evaluating hand-related injuries, establishing a new therapy program, and establishing an outcome measurement (Yancosek & Howell, Citation2009). Applications of dexterity tests differ according to the individual need; hence it involves the role of different professional perspectives like physiotherapy, occupational hand therapy, neuroscience, and clinical psychology (James M. Hunter et al.,). However, the study of hand skills is not only for individual needs but also of interest in the fields of motor learning and control, developmental psychology, and, more recently, ergonomics and robotics.
Rehabilitation requirement is forecasted to increase over the next decade due to the increasing number of elderly Indians in agreement with the global trends (Cieza et al., Citation2021; S. H. Lee et al., Citation2021). Motion analyzing laboratories are specially designed and augmented by superior instruments for upper extremity analysis. However, they require expensive specialized instrumentation and engineering support. Furthermore, bringing patients to motion analysis laboratories is inconvenient for clinicians and caregivers. During one of our visits to the hospital’s physiotherapy department, it was full of patients waiting for their turn for the therapy. Clinicians were fully occupied and handled the cases sequentially as most of the associated measurements were manual and required one-to-one intervention. This was a big challenge for the therapist. Thus, in this research work, an instrumented hand dexterity assessment battery is developed, which reduces the clinician intervention time and assesses the upper limb with minimum infrastructure, as in the case of the home environment.
The present work aims to develop an indigenous portable device for assessing upper extremities to reduce clinician intervention time. The main focus of this research is to investigate the feasibility of using a low-cost non-wearable sensor that is easy to use and does not require any calibration. Without disturbing the hand’s natural movement, we wanted to acquire the hand’s functional parameters, which is the novelty of the work. Minimum infrastructure and easy-to-handle objects are targeted to make assessments suitable for home-based rehabilitation. In this research, we have incorporated two test items for assessing fine motor skills: The finger-tap counter as the first task and Loop and wire test as the second task. Description of the test items related to fine motor examination is discussed further in the methodology section. This paper is structured as follows: Section 2 discusses the related work in the hand dexterity test. Section 3 contains methodology, which explains the experimental procedure and algorithm implemented in developing the test set-up. In section 4, results obtained with our method are explained, followed by a discussion in section 5 and the concluding remarks in section 6.
2. Related work
Various traditional dexterity measurement tests are available in the database. The lists of different test instruments are based on electronic databases such as PubMed, Medline, EMBASE, Cochrane library, IEEE Xplore, Google Scholar, and CINAHL. Only those test instruments are considered which have standard procedures and norms. The keywords used in the search are upper extremity, upper limb or arm and assessment test, dexterity, hand function test, and outcome measure. Measures not specific to the upper limb are excluded from the search.
Purdue Pegboard Test (PPT) includes four subtests that measure the gross movement of the arm, hand, and fingertip dexterity (Tiffin & Asher, Citation1948). PPT is initially designed to evaluate employee performance at work, mainly in the packing and assembly industry. Tiny objects such as pins, washers, and collars are moved one at a time and placed on the pegboard as per the instruction. A total of four sub-tests, timed for 30 seconds, were included. PPT also tested with 147 Schizophrenia patients and found moderate test-retest reliability (Posen P. Lee et al., Citation2013). Though the test is well-established, it demands more cognitive speed and attention control than other dexterity tests (Lindstrom-Hazel & VanderVlies Veenstra, Citation2015).
Moberg (Citation1958) assessed hand dexterity and functional sensibility using Moberg Pick-Up Test (MPUT). The test includes a stopwatch, 12 small objects, a container, and a wooden surface. Time taken to complete the task includes picking up 12 small objects and placing them into a container. The effect of age on a subject’s performance during MPUT needs to be analyzed. Silva et al. (Citation2017) performed the clinical measurement with hand osteoarthritis patients and found the significance of MPUT. This test can be reproduced with the specifications but is not readily available. Drussell (Citation1959) and Desrosiers et al. (Citation1997) developed a test kit to examine the speed of gross arm and hand movement through the Minnesota Rate of Manipulation Test (MRMT). This is the first version of the Minnesota Manual Dexterity Test (MMDT), which uses two boards and 60 short, round blocks. MRMT device can be purchased online, which consists of five timed subtests. Manual dexterity can be calculated when patients turn 60 blocks from one board to another. Wang et al. (Citation2018) performed a cross-sectional study using a revised board of MRMT. The downside of MRMT is that test requires much space due to the size of the boards.
Jebsen et al. (Citation1969) developed a Jebsen Taylor Hand Function Test (JHFT), which measures hand function and dexterity based on timing criteria. Using simulated ADL, both fine and gross motor hand function is tested in JHFT. The test includes unilateral activities designed to showcase various hand activities in daily life. Seven timed functional tasks, namely writing a short sentence, turning over 3 × 5 inch cards, picking up small objects and placing them in a container, stacking checkers, simulated eating, moving large empty cans on a table, and moving weighted large cans. Sığırtmaç and Öksüz (Citation2021) verified the psychometric properties the hand injured patients during dexterity assessment. JHFT is found to be a reliable instrument for the hand function test. Some of the test items in JHFT require cognitive ability, and writing tasks using a non-dominant hand are always challenging. Kellor et al. (Citation1971) developed a test to measure finger dexterity called Nine-Hole Pegboard Test (NHPT). The test consists of a pegboard and nine pegs. This timed measure of fine dexterity involves placing and removing nine pegs in a pegboard. Two hundred fifty subjects were taken as a sample, and normative data was prepared. The authors have not performed validity or reliability test. Fugl-Meyer et al. (Citation1975) prepared Fegl Meyer Assessment (FMA) for motor impairment assessment using 155 test items. A three-point ordinal scale was used as a Functional Ability Scale (FAS). However, administration consumes much time in FMA; otherwise, this test is used widely in the quantitative assessment of motor impairment. Mathiowetz et al. (Citation1985) developed the Box and Block Test (BBT), which measures unilateral gross manual dexterity. Manual dexterity is measured by repeatedly moving one-inch blocks from one side to another side of the box in 60 seconds. BBT deserves good clinical utility. It can be used with a wide range of populations, including clients with stroke. BBT is quick, simple test equipment but more expensive (USD 219.65) than other pegboard assessments. Ruff and Parker (Citation1993) have developed Grooved Pegboard Tests (GPT) for age and gender-specific 360 healthy subjects. This test slightly differs in comparison to the normal peg. The peg has to fit into a hole on the board when perfectly oriented and hence work as a lock & key feature. Al-Naami et al. (Citation2022) proposed an electronic version of GPT and tested it with forty healthy and six chronic condition patients. The authors claim that human errors while operating a stopwatch are reduced, and the device makes it to use in the home environment. This test only addresses fine motor and lacks the tests for gross motor function. The test requires accurate visual attention and thumb and index finger coordination. Hence, grooved pegboard assessment is suitable for testing the neuropsychological and psychometric properties of the subject. Aaron and Jansen (Citation2003) introduced the Functional Dexterity Test (FDT) and tested it with 46 hand-injured patients using sixteen wooden pegs. Time taken to turn wooden pegs and reinsert them into the pegboard calculated and validity established. Like many dexterity tests, FDT is also a time-based dexterity test and measures test performance based only on test speed. The FDT cannot find whether the participant can accomplish a task or not, which is the downside of most dexterity test set-ups.
From the literature on various traditional dexterity tests, it is observed that clinicians must continuously monitor the stopwatch during the test process. In addition to this, there may be variation in noting down the time. This is mainly due to the “reaction time” of the clinician. Clinicians need to wait continuously for the patient to start the test, holding the stopwatch ready in hand. On the other hand, computer-based hand dexterity measurement has better outcomes than paper and pencil measurements (Levanon, Citation2013). Many attempts have been made to automate the pegboard test in the literature. Jobbágy et al. (Citation2018); Ingram et al. (Citation2019) have developed a smart pegboard that reduces clinician burden during the pegboard-related test. Johansson and Häger (Citation2019) have developed a standardized NHPT set-up that consists of two pegboards. The limitation, or rather unavailability of the features in these test set-ups is the detection of the number of pegs held in hand during the test session. A patient can pick up more than one peg during the insertion or removal process and falsely improve the test score. Also, not following the specific pattern during the peg insertion and removal process may lead to unintentional delay and reduces test-retest reliability. These conditions are common and need to take care during development of the device for telerehabilitation. Thus, in our previous research work (Acharya et al., Citation2021), we developed a portable, cost-effective pegboard that is easy to administer and time-efficient. During the present pandemic, going clinic each time for outcome measurement is a tedious job. In this research work, the electronic model of the dexterity test kit is made to overcome manual errors, thereby making it a more reliable and accurate system for improving patients’ hand-eye coordination and motor skills. The first apparatus developed in this work is the reaction time testing system. Reaction time is calculated as the time taken for the subject to react to the Light Emitted Diode (LED) signal, which changes once the subject’s push button is pressed manually. The second apparatus is the Loop Wire testing system, wherein the total time to complete the navigation of a hand-held lock and key unit through a three-dimensional maze is calculated.
3. Methodology
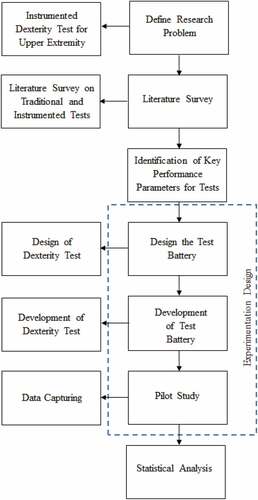
The research methodology adopted for developing hand dexterity tests is shown in . The research focuses on identifying problems in the existing scenario of dexterity tests in hospitals and defines the problem statement. The research work is carried out to design and develop a dexterity test for the upper extremity. The research problem’s definition is strengthened by extensive literature surveys in traditional and automated hand dexterity tests. Further, based on findings from the literature, key performance indicators such as time, number of failures, etc., are identified to capture the status of hand functions and to perform the analysis. The suitable dexterity test items are identified based on parameters, and experimentation is designed. Two test items, namely the Finger-tap counter, Loop and wire test, are designed and developed as a test battery and pilot study performed on normal subjects to capture the data for the key performance indicators. Further, the captured data is statistically analyzed to evaluate the effectiveness of the automated hand dexterity test.
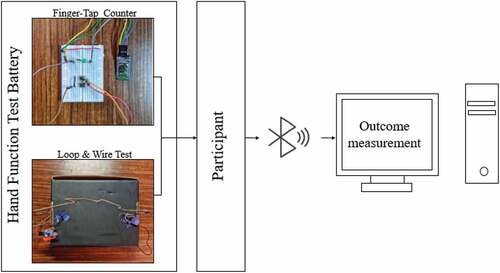
The two test items developed in this work are the finger-tap counter and Loop and wire test. Hardware components consist of Arduino Uno (ATmega328P microcontroller), HC-05 Bluetooth module, pushbuttons, piezo buzzer, clip handle, metal lock, and LED. The overall structure of the instrumented hand dexterity test unit conceptual model is shown in . The hardware design and test battery were developed with input from a physiotherapy expert at our medical college. During the test process, a participant should sit upright on a chair with no armrests. The height of the table is fixed to the subject’s waist level. Participant trunks during the performance of a test should always be in contact with the chair’s back. The reaction time and test completion time are recorded wirelessly via Bluetooth for improved system portability.
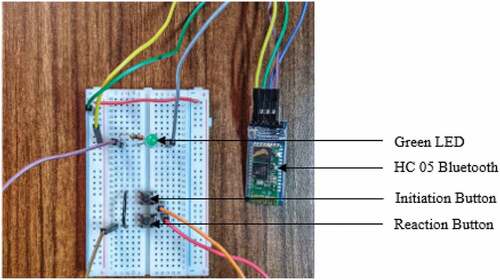
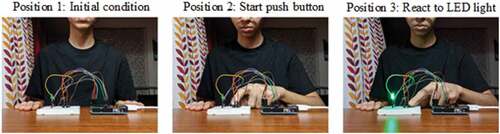
3.1. Finger-tap counter
The first apparatus developed in this work is the finger-tap counter, as shown in . This test set-up uses a push button and LED to observe and analyze the response time from the indication to the reply. It will randomly turn on a LED and measure the time delay the subject takes to press a button. The participant has to keep their hands on the table in sitting condition, as shown in . The participant can make the device ready by pressing the initiation push button with the help of a hand that is not under examination. The initiation button triggers the random delay function to illuminate the LED after a random interval as per the requirement. Reaction time is calculated as the time taken by the subject to react to the green LED signal. The developed test set-up logic is described in the flowchart (). To avoid unintentional delay, an upper limit on time to complete the activity has been fixed at one minute. Counter increment happens when the participant responds to the LED and gives the timing information as “reaction time”.
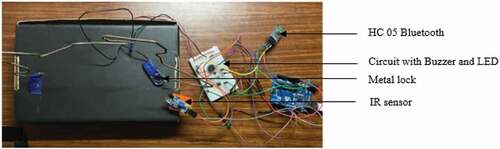
3.2. Loop and wire test
The loop and wire test apparatus uses a bent wire, a piezo buzzer, and an IR sensor. The maze structure is made out of a coat hanger attached to a cardboard base, as shown in . Participant navigates a hand-held metal lock through a three-dimensional maze, and the sequence in the test process is shown in .
Participant has to move the metal lock fast and as accurately as possible, i.e., without touching the wire structure. If the participant touches the metal lock to the wire structure, a piezo buzzer makes the alert sound. The total number of touches by the metal lock is recorded, and after each trial, the total time taken to perform the test is calculated. The IR sensor is connected to the D10 port of the Arduino. Completion of hand movement is recognized by the IR sensor, which is placed near the destination side of the loop wire structure. The electronic timer stops as soon as the IR sensor detects the metal lock near the destination site. The system also uses a piezo buzzer to provide acoustic feedback on failure. shows the flowchart of the Loop and wire test set-up working process. Counter value gives the number of failures i.e., count of metal lock touching the bent wire. Total time is also displayed, which is the time the metal lock takes from source to destination.
4. Results
In the developed two dexterity tests (), the dominant hand is considered the right hand, and the left hand is considered non-dominant. Healthy 30 subjects between the age range (20–35, 36–50, 51–65, and 66–80) were tested for both tests. In the reaction time tester experiment, the output is displayed on the clinician’s computer without any delay. The test was performed using the dominant hand and the non-dominant hand separately. The general characteristics of 30 healthy participants (for dominant-hand usage) and the timing information of each test item are listed in .
Table 1. General characteristics of the participants (for dominant-hand usage)
portrays the results obtained when each age group performs the Finger-tap counter test. The X-axis shows the age of the subjects tested (in years), and the Y-axis shows the reaction time observed during dominant and non-dominant hand (in seconds) usage. It is observed that reaction time is shortest for the 20–35 age group. The observation leads us to believe that the reaction time gradually increases in the age range of 36–50 years, and the rise continues in the age range of 66–80. Hand and eye coordination are very fast in the 20–35 age group compared to the other three age groups.
Figure 11. Plot showing the correlation between dominant and non-dominant hand during finger- tap counter test.
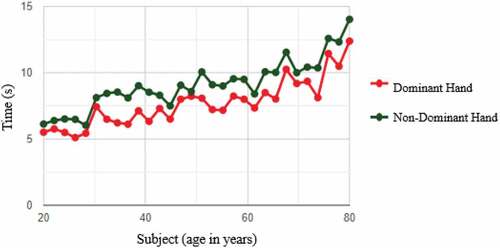
Unlike the dominant hand results for the subjects, the average time taken to complete the test using the non-dominant hand is much higher because the dominant hand is used more often every day. The neurons that carry messages between that hand and the brain are faster at transmitting electrochemical signals. The neural pathway involved in a reaction time experiment involves a series of neural processes. The time (in seconds) required to complete Finger tap counter test for dominant and non-dominant hands are captured for 30 samples. These time values are used to calculate the correlation and to plot the graph. As per the time values, the R-squared value calculated is 0.914406701. This shows a high correlation as the age interval changes.
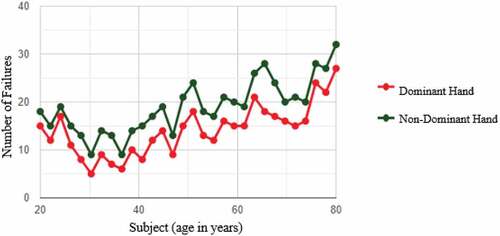
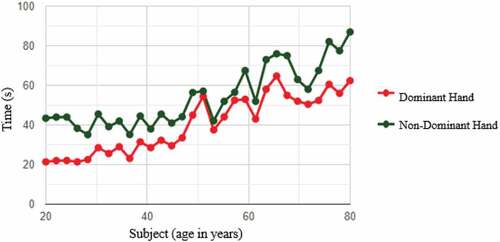
The second dexterity test set-up was the Loop and wire test. This was used to observe two main parameters: the number of failures while performing the test and the total time taken to perform the test. portrays the results obtained when each of the four age groups performed the Loop and wire test. In this, X-axis shows the age of the subjects tested (in years), and the Y-axis shows the reaction time observed during dominant and non-dominant hand (in seconds) usage. This observation leads to believe that the average time taken to complete the test increases with an increase in age, and the dominant hand is always quicker than the non-dominant hand. The observation also shows that the average number of failures increases with age when compared to subjects with the same dominance of hands. The time (in seconds) required to complete Loop and Wire test for dominant and non-dominant hand are captured for 30 samples. These time values are used to calculate the correlation and to plot the graph. As per the time values, the R-squared value calculated is 0.857856501. This shows correlation as the age interval changes.
Figure 12. Plot showing the correlation between dominant and non-dominant hand during loop and wire test.
portrays the results obtained when the four age groups performed the Loop and wire test. The X-axis shows the age of the subjects tested (in years), and the Y-axis shows the number of failures, i.e., the count of metal locks touching the bent wire during the test process. The average failures tend to increase in the case of non-dominant hand use, and the number of failures is greatest in the 66–80 age group due to involuntary movements of the hand due to aging.
5. Discussion
Human activity recognition using wearable sensors such as IMU or Kinect is an interesting topic (Hughes et al., Citation2019; Hussain et al., Citation2019; Werner et al., Citation2022; Zhuang et al., Citation2019). This work calculates subject response time using the finger-tap counter test. With the introduction of a Bluetooth module, obtaining the serial monitor output on a mobile device makes the system independent of a computer, thereby making the system easy to carry and operate in remote places. In the second system, the loop and wire testing mechanism, the results are obtained to determine the number of failures a subject face while moving the hand-held metal lock over the loop from the initial point to the final point of the maze structure. With a piezo buzzer, acoustic observations concerning the number of failures were recorded during the procedure and displayed for future analysis.
As discussed in the result section, the observations show an increasing trend in the average time taken to complete the test as the age increases. This study remained the same throughout the testing of the 30 subjects, which were observed within three weeks. The boxplot helps us to understand the pattern in the data set in a better way. shows that the median time taken to perform the task is increasing over the different age groups. One can also observe that the age group of 66–80 takes longer to complete the experiment, followed by 51–65 age group. Also, the participants in the age group 20–35 take the least time to complete all four experiments.
Figure 14. Box plot shown for the four age groups (a) Finger-tap counter-dominant hand (b) Finger-tap counter-non-dominant hand (c) Loop and wire test-dominant hand (d) Loop and wire test-non-dominant hand.
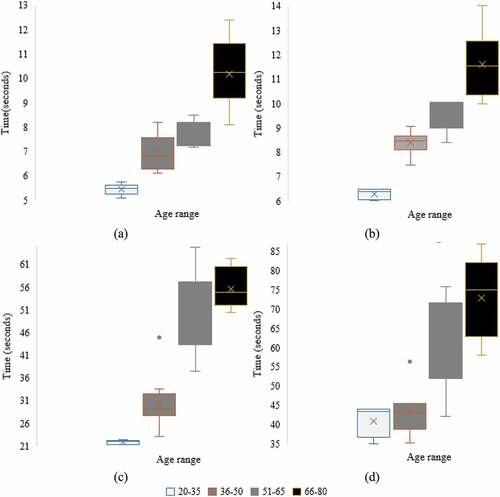
In the finger-tap counter test, the average time taken by the female age group (7.40 seconds) is less than that of the male group (8.07 seconds). In the loop and wire test, the average time taken to perform the test (42.36 seconds) in the male group is greater than the female (38.93 seconds) group. Interestingly, the average time taken and the number of failures are more for male groups. Female groups can perform loop and wire tests with fewer errors irrespective of age group. The fine dexterity of the female participant is well developed as most of the participants are house makers, and their day-to-day household activity helped them develop this skill set. However, this observation cannot be generalized as these two tests are conducted with a sample size of 30 participants.
Although numerous studies have shown a link between increasing age and decreased hand dexterity, few studies have attempted to investigate the causes of the link. Martin et al. (Citation2015) offer a usual clarification, indicating that the association between rising age and decreased hand dexterity is most likely explained by a deterioration in musculoskeletal strength and mass. The steadiness and line tracking hand dexterity tests both require stable arm and hand control and eye-hand synchronization with visual steering. The variance of steadiness and line tracking hand dexterity had minimal predictive value for strength, implying that other factors may have influenced the outcome. The future scope conjointly includes creating a much more portable and compact version of the dexterity set-up. This could be by utilizing a pre-wired soldered PCB to fuse the circuit and create it simple to incorporate with the setup to make the system compact and increase its shelf life by having the elements soldered. Android App or web-based simple Electronic Medical Records (EMR) system needs to be developed and that has to be linked with the cloud.
6. Conclusions
Assessing dexterity is critical as dexterity is a central component of hand function. An automated version of the finger-tap counter and loop and wire tests is designed and experimented on 30 subjects. There are several advantages of implemented tests over traditional test methods, such as less clinician interference, uniformity in scoring, and maintaining the database of complete test sessions for future analysis. This study is further essential to understanding humans’ relationships between age and dexterity. The motor tests were chosen to reflect factors contributing to the evaluation of hand dexterity. Increased age is significantly associated with decreased hand dexterity. During the COVID-19 pandemic, the developed system aims to provide a home-based assessment that benefits patients with lower extremity dysfunctions. This automated version of the test battery increases the reliability of outcomes and certainly helps clinicians in guiding further action on therapeutic aspects. The end result can help us understand how the hand’s movement changes during the test and if any neurological conditions are present in the patient.
The research work is further extended with the patient data related to hand rehabilitation activities. There is a need to maintain test data in Electronic Medical Records (EMR) for the subjects during each rehabilitation session. This will help to analyze the performance improvement. In future work, quantitative parameters related to improvements during rehabilitation should be extracted from the old data, and auto-comparison features need to be incorporated based on the requirement. Cloud-based mobile apps or web apps will be developed for better visualization, which can be provided to the clinician and subject.
Acknowledgements
The authors are thankful to Dr. Bhamini Krishna Rao, Department of Physiotherapy, Manipal College of Health Professions, MAHE, for the necessary support and guidance in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Sarthak Cheema
Sarthak Cheema completed B. Tech in Instrumentation and Control Engineering from Manipal Institute of Technology, Manipal. He completed this research under Prof. Aneesha Acharya K. This research was mainly divided into four main parts per each author’s contribution. Conceptualization and Supervision are by Aneesha Acharya K. Methodology and implementation by Sarthak Cheema. The investigation, writing original Draft by Dr. Somashekara Bhat and Dr. Kanthi M. Writing – Review & Editing By Dr. Sucheta V Kolekar. Professor Aneesha Acharya K submitted his thesis synopsis to the university titled “Upper Extremity Assessment Using an Instrumented Hand Function Test,” He is continuing his research in upper extremity assessment and wearable devices.
References
- Aaron, D. H., & Jansen, C. W. (2003). Development of the Functional Dexterity Test (FDT): Construction, validity, reliability, and normative data. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 16(1), 12–16. https://doi.org/10.1016/s0894-1130(03)80019-4
- Acharya, K. A., Bhat, S., Kanthi, M., & Rao, B. K. (2021). Fine motor assessment in upper extremity using custom-made electronic pegboard test. Journal of Medical Signals and Sensors, 12(1), 76–83. https://doi.org/10.4103/jmss.JMSS_58_20
- Al-Naami, B., Al-Naimat, F., Almalty, A.-M. R.-M., Visconti, P., & Al-Hinnawi, A.-R. (2022). A prototype of an electronic pegboard test to measure hand-time dexterity with impaired hand functionality. Applied System Innovation, 5(1), 2. https://doi.org/10.3390/asi5010002
- Cieza, A., Causey, K., Kamenov, K., Hanson, S. W., Chatterji, S., & Vos, T. (2021). Global estimates of the need for rehabilitation based on the global burden of disease study 2019: A systematic analysis for the global burden of disease study 2019. Lancet (London, England), 396(10267), 2006–2017. https://doi.org/10.1016/S0140-6736(20)32340-0
- Desrosiers, J., Rochette, A., Hébert, R., & Bravo, G. (1997). The Minnesota manual dexterity test: reliability, validity and reference values studies with healthy elderly people. Canadian Journal of Occupational Therapy, 64(5), 270–276. https://doi.org/10.1177/000841749706400504
- Drussell, R. D. (1959). Relationship of Minnesota rate of manipulation test with the industrial work performance of the adult cerebral palsied. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association, 13(2), Part 2. https://pubmed.ncbi.nlm.nih.gov/13637161/
- Fugl-Meyer, A. R., Jääskö, L., Leyman, I., Olsson, S., & Steglind, S. (1975). The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scandinavian Journal of Rehabilitation Medicine, 7(1), 13–31. https://pubmed.ncbi.nlm.nih.gov/1135616/
- Hughes, C., Baye, M., Gordon-Murer, C., Louie, A., Sun, S., Belay, G. J., & Zhang, X. (2019). Quantitative assessment of upper limb motor function in Ethiopian acquired brain injured patients using a low-cost wearable sensor. Frontiers in Neurology, 10, 1323. https://doi.org/10.3389/fneur.2019.01323
- Hunter, J. M., Schneider, L. H., Mackin, E. J., & Callahan, A. D., Harrison, D. H. (1985). Rehabilitation of the Hand, 2. https://doi.org/10.1002/bjs.1800720647
- Hussain, T., Maqbool, H. F., Iqbal, N., Khan, M., Salman, N. A., & Sanij, A. A. D. (2019). Computational model for the recognition of lower limb movement using wearable gyroscope sensor. International Journal of Sensor Networks, 30(1), 35–45. https://doi.org/10.1504/ijsnet.2019.099230
- Ingram, L. A., Butler, A. A., Walsh, L. D., Brodie, M. A., Lord, S. R., & Gandevia, S. C. (2019). The upper limb physiological profile assessment: Description, reliability, normative values and criterion validity. PloS one, 14(6), e0218553. https://doi.org/10.1371/journal.pone.0218553
- Jebsen, R. H., Taylor, N., Trieschmann, R. B., Trotter, M. J., & Howard, L. A. (1969). An objective and standardized test of hand function. Archives of Physical Medicine and Rehabilitation, 50(6), 311–319. https://pubmed.ncbi.nlm.nih.gov/5788487/
- Jobbágy, Á., Marik, A. R., & Fazekas, G. (2018). Quantification of the upper extremity motor functions of stroke patients using a smart nine-hole peg tester. Journal of Healthcare Engineering, 2018, 7425858. https://doi.org/10.1155/2018/7425858
- Johansson, G. M., & Häger, C. K. (2019). A modified standardized nine hole peg test for valid and reliable kinematic assessment of dexterity post-stroke. Journal of Neuroengineering and Rehabilitation, 16(1), 8. https://doi.org/10.1186/s12984-019-0479-y
- Kellor, M., Frost, J., Silberberg, N., Iversen, I., & Cummings, R. (1971). Hand strength and dexterity. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association, 25(2), 77–83. https://pubmed.ncbi.nlm.nih.gov/5551515/
- Lee, S. H., Hwang, Y. J., Lee, H. J., Kim, Y. H., Ogrinc, M., Burdet, E., & Kim, J. H. (2021). Proof-of-concept of a sensor-based evaluation method for better sensitivity of upper-extremity motor function assessment. Sensors (Basel, Switzerland), 21(17), 5926. https://doi.org/10.3390/s21175926
- Lee, P., Liu, C. H., Fan, C. W., Lu, C. P., Lu, W. S., & Hsieh, C. L. (2013). The test-retest reliability and the minimal detectable change of the Purdue pegboard test in schizophrenia. Journal of the Formosan Medical Association = Taiwan Yi Zhi, 112(6), 332–337. https://doi.org/10.1016/j.jfma.2012.02.023
- Levanon, Y. (2013). The advantages and disadvantages of using high technology in hand rehabilitation. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 26(2), 179–183. https://doi.org/10.1016/j.jht.2013.02.002
- Lindstrom-Hazel, D. K., & VanderVlies Veenstra, N. (2015). Examining the Purdue pegboard test for occupational therapy practice. The Open Journal of Occupational Therapy, 3(3). https://doi.org/10.15453/2168-6408.1178
- Martin, J. A., Ramsay, J., Hughes, C., Peters, D. M., & Edwards, M. G. (2015). Age and grip strength predict hand dexterity in adults. PloS one, 10(2), e0117598. https://doi.org/10.1371/journal.pone.0117598
- Mathiowetz, V., Volland, G., Kashman, N., & Weber, K. (1985). Adult norms for the box and block test of manual dexterity. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association, 39(6), 386–391. https://doi.org/10.5014/ajot.39.6.386
- Moberg, E. (1958). Objective methods for determining the functional value of sensibility in the hand. The Journal of Bone and Joint Surgery. British Volume, 40-B(3), 454–476. https://doi.org/10.1302/0301-620X.40B3.454
- Ruff, R. M., & Parker, S. B. (1993). Gender- and age-specific changes in motor speed and eye-hand coordination in adults: Normative values for the finger tapping and grooved pegboard tests. Perceptual and Motor Skills, 76(3 Pt 2), 1219–1230. https://doi.org/10.2466/pms.1993.76.3c.1219
- Sığırtmaç, İ. C., & Öksüz, Ç. (2021). Investigation of reliability, validity, and cutoff value of the Jebsen-Taylor hand function test. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 34(3), 396–403. https://doi.org/10.1016/j.jht.2020.01.004
- Silva, P. G., Jones, A., Fernandes, A., & Natour, J. (2017). Moberg picking-up test in patients with hand osteoarthritis. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 30(4), 522–528. https://doi.org/10.1016/j.jht.2016.10.005
- Tiffin, J., & Asher, E. J. (1948). The Purdue pegboard; norms and studies of reliability and validity. The Journal of Applied Psychology, 32(3), 234–247. https://doi.org/10.1037/h0061266
- Wang, Y. C., Wickstrom, R., Yen, S. C., Kapellusch, J., & Grogan, K. A. (2018). Assessing manual dexterity: Comparing the workability rate of manipulation test with the Minnesota manual dexterity test. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 31(3), 339–347. https://doi.org/10.1016/j.jht.2017.03.009
- Werner, C., Schönhammer, J. G., Steitz, M. K., Lambercy, O., Luft, A. R., Demkó, L., & Easthope, C. A. (2022). Using wearable inertial sensors to estimate clinical scores of upper limb movement quality in stroke. Frontiers in Physiology, 13, 877563. https://doi.org/10.3389/fphys.2022.877563
- Yancosek, K. E., & Howell, D. (2009). A narrative review of dexterity assessments. Journal of Hand Therapy: Official Journal of the American Society of Hand Therapists, 22(3), 258–270. https://doi.org/10.1016/j.jht.2008.11.004
- Zhuang, W., Chen, Y., Su, J., Wang, B., & Gao, C. (2019). Design of human activity recognition algorithms based on a single wearable IMU sensor. International Journal of Sensor Networks, 30(3), 193. https://doi.org/10.1504/IJSNET.2019.100218