Abstract
In a 21-year-old male with bilateral cleft lip who developed marked venous congestion of a lip switch flap, we returned the grafted flap to the donor site to improve blood circulation of the flap and then re-transplanted it, which prevented flap necrosis. Here, we report the procedure and case.
Introduction
A lip switch flap is an axial-pattern flap using the inferior labial artery as a feeding blood vessel. Its morphology is appropriate to improve the upper lip morphology in the presence of severe cleft lip and nose deformity. It is capable of simultaneously reconstructing the philtrum and extending the bridge of the nose, and was reported to be very useful and be associated with fewer complications in many cases.[Citation1–4] Cutting et al. [Citation5] described it was very important to proceed in secondary bilateral cleft lip reconstruction with lip switch flap only after the midface and nose repair done.
On the other hand, the vascular pedicle of this flap is very thin and circulatory disorder occurs due to 180° rotation of the pedicle, being a risk for flap necrosis.[Citation6] However, there has been no specific report on its rescue.
We treated a patient with severe venous congestion of a lip switch flap. The grafted flap was returned to the donor site to improve blood circulation of the flap, followed by its re-transplantation, which prevented necrosis of the flap. Here, we report the procedure by presenting the case.
Case report
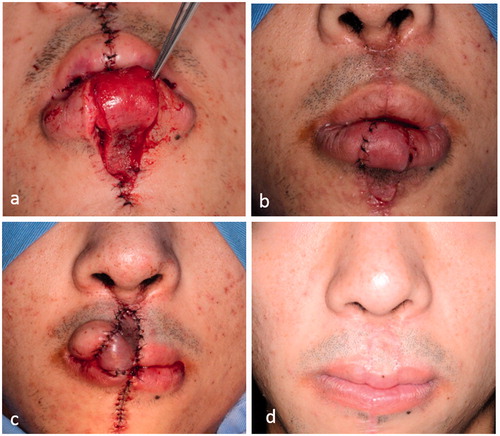
The patient was a 21-year-old male with bilateral cleft lip. Severe cleft lip nose deformity, i.e. a short bridge and flat apex of the nose, were observed. Under general anesthesia, the nasal morphology was improved using cartilage of the nasal septum, and the lip deformity was improved by forming a tubercle of the upper lip using a lip switch flap with left inferior labial arterial and venous pedicles, the philtrum and bridge of the nose. The lower lip flap was designed to have a ∼10-mm width and a ∼17-mm length and transplanted to the upper lip. Its color immediately after surgery was favorable (), but marked swelling of the flap and surrounding tissue was noted 6 h after surgery, with which the flap developed venous congestion (). To release pressure due to the swelling on the vascular pedicle, sutures around the pedicle were removed, but blood circulation of the flap did not improve and congestion aggravated. Since flap necrosis was predicted, the flap that had been transplanted to the upper lip was returned to the lower lip 8 h after surgery to improve its blood circulation and prevent necrosis. Under venous sedation, the flap transplanted to the upper lip was released to a free state so that the mouth could be opened, oropharyngeal intubation was applied and sedation was switched to general anesthesia. Hematoma around the flap was removed by washing well with saline. After confirming blood flow from the flap stump, the flap was returned to the lower lip and fixed by sutures, and the transplantation site was simply sutured ().
Figure 1. (a) At the completion of surgery, (b) 6 h after surgery and (c) the flap was returned to the lower lip.

After surgery, the flap was covered with heparinized saline-soaked gauze to further reduce congestion. Congestion was improved 7 h after surgery (), and the flap returned to the donor site had almost completely recovered 1 week after surgery (). The flap was re-transplanted with sufficient tissue around the pedicle under local anesthesia (). Flap engraftment was favorable, and it was transected after 9 days. As of 2 years after surgery (), the cleft lip nose deformity had improved with a favorable course.
Discussion
In cleft lip patients with upper lip tissue defects, a complication of a lip switch flap, flap necrosis, results in failure of upper lip reconstruction. Thus, methods to prevent this complication are very important.
The feeding artery of a lip switch flap, the inferior labial artery, is distributed within 15 mm from the upper end of the lower lip.[Citation7] It is very thin, and 180° rotation of the vascular pedicle is likely to cause ischemia due to twisting and pressure. Since the vein distributing along with the inferior labial artery is unclear, venous perfusion by the surrounding oral mucosa is considered very important.[Citation8] But, when oral mucosa is too thick, there is the problem that the shape of upper lip comes to worse. Similarly, when pressure is loaded on the vascular pedicle and surrounding tissue by tension induced by flap rotation and swelling after surgery, venous congestion readily occurs, being a risk for partial or total necrosis. Since the vascular pedicle of the flap is very thin, the risk should be fully considered, and we encountered it in 2 of 32 patients treated over the last 10 years.
In the present patients, venous congestion was treated by removing sutures around the vascular pedicle to release tension loaded by the surrounding tissue, such as mucosa and muscle, and phlebotomy was also applied, but these were ineffective, and congestion of the flap rapidly progressed, being likely to result in total necrosis. We considered the application of medical leeches to improve congestion,[Citation9] but this was abandoned because the patient rejected it and the progression of congestion was rapid due to the small size of the flap. When severe venous congestion develops in a lip switch flap, like this case, it is likely to rapidly progress and result in total necrosis. Thus, the early discovery of congestion by careful observation of the flap after surgery and rapid treatment upon suspecting congestion are very important. The flap could be re-transplanted after it was returned to the donor site to sufficiently recover circulation in tissue around the vascular pedicle, and it engrafted and achieved a favorable upper lip morphology, reconfirming that, when congestion is suspected, the flap should be treated without hesitation.
Various modifications have recently been added to the previous lip switch flap, and the vascular pedicle was further thinned to improve mobility in some modifications.[Citation10,Citation11] In these two cases, we should have thickened the oral mucosa a little more intraoperatively to avoid congestion. Attention should be paid to venous congestion, and preparation for its treatment may be important.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- McGregor IA. The ABBE flap its use in single and double lip clefts. Br J Plast Surg. 1963;16:46–58.
- Erol OO, Pence M, Agaoglu G, et al. The Abbé island flap for the reconstruction of severe secondary cleft lip deformities. J Craniofac Surg. 2007;18:766–772.
- Koshy JC, Ellsworth WA, Sharabi SE, et al. Bilateral cleft lip revisions: the Abbe flap. Plast Reconstr Surg. 2010;126:221–227.
- Larsson J, Becker M, Svensson H. The Abbé flap in cleft lip and palate repair. J Plast Surg Hand Surg. 2013;47:524–527.
- Cutting CB, Warren SM. Extended Abbe flap for secondary correction of the bilateral cleft lip. J Craniofac Surg. 2013;24:75–78.
- Eskeland G, Borchgrevink H, Abyholm FE. Columella lengthening in bilateral cleft lip patients. Experience with the forked flap procedure. Scand J Plast Reconstr Surg. 1979;13:429–436.
- Schulte DL, Sherris DA, Kasperbauer JL. The anatomical basis of the Abbé flap. Laryngoscope. 2001;111:382–386.
- Ohtsuka H. One-stage lip-switch operation. Plast Reconstr Surg. 1985;76:613–615.
- Utley DS, Koch RJ, Goode RL. The failing flap in facial plastic and reconstructive surgery: role of the medicinal leech. Laryngoscope. 1998;108:1129–1135.
- Hu H, Song R, Sun G. One-stage inferior labial flap and its pertinent anatomic study. Plast Reconstr Surg. 1993;91:618–623.
- Wu D, Song T, Li H, et al. An innovative cross-lip flap with a musculomucosal pedicle based on the vascular network of the lower lip. Plast Reconstr Surg. 2013;131:265–269.