Abstract
We report a case of complete DIEP flap survival, following venous congestion due to the excision of a local recurrence with main pedicle, 4 years after its transfer for breast reconstruction.
Introduction
Recent studies have shown equivocal results concerning free flap survival or necrosis following pedicle avulsion or thrombosis in the early or late post-operative period. It is still unclear whether free flaps remain dependent on blood supply from their vascular pedicle or if there is an autonomization process characterised by neoangiogenesis from the surrounding recipient bed. A complete flap survival of deep inferior epigastric perforator (DIEP) flap, following venous congestion due to the excision of a local recurrence with main pedicle, 4 years after its transfer for breast reconstruction is reported.
Case report
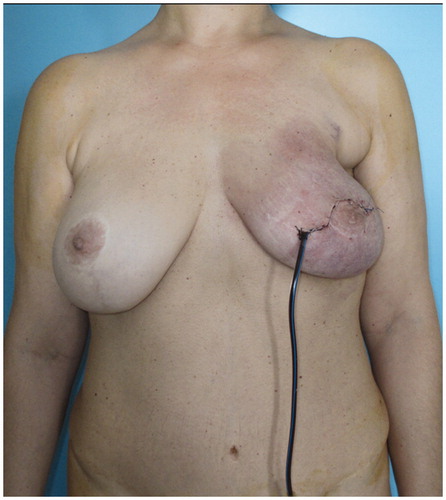
In 2011, a non-smoking 44-year-old patient with multifocal invasive ductal carcinoma to the left breast underwent superior lateral quadrantectomy and ipsilateral axillary lymph node dissection. The finding of positive margins of resection required a skin-sparing mastectomy (SSM), with immediate DIEP flap reconstruction and contralateral mastopexy () 1 month later. Flap’s weight was 425 g including zones 1–3 and was harvested on two perforators from the lateral raw. The superficial inferior epigastric vein (SIEV) was included in the flap also. The deep inferior epigastric artery and vein (DIEA and DIEV) were anastomosed to the circumflex scapular artery and one satellite vein, while the SIEV was anastomosed to the thoracodorsal vein. Nipple areola complex (NAC) was repositioned as a free graft after intraoperative confirmation of margins free from disease. Operative time lasted 5 h and 20 min and the patient was discharged on post-operative day 6 without complications. No adjuvant chemotherapy or radiotherapy was performed. In 2015, due to a local recurrence at the superior lateral quadrant from 1 to 2 o’clock, a wide excision was performed severing both the DIEV and SIEV. A slowly progressive vein congestion, involving the entire breast skin, was observed 2 h after the surgical procedure ().
Figure 1. Frontal view. Patient with a previous left supero-lateral quadrantectomy and lymphadenectomy underwent left skin sparing mastectomy (SSM) and immediate DIEP flap reconstruction and contralateral mastopexy.

Figure 2. Frontal view. After a wide excision of a local recurrence at the supero-lateral quadrant border of the flap 4 years after flap transfer, a progressive venous congestion involving the whole flap was observed during the immediate postop, because of the sacrifice of vein pedicle.
Since transcutaneous Doppler signals for artery and vein perforator were still present, it was decided not to take the patient back to the theatre for revision. During the following five postoperative days, vein congestion slowly recovered with breast skin to its normal aspect. No clinical or ultrasound presence of liponecrosis were found at 5 months follow-up, with an optimal aesthetic outcome ().
Discussion
Free flaps rarely survive completely to post-operative resection of its vascular pedicle, while favourable outcomes are mainly reported in early post-op [Citation1–5] (). A TRAM flap lost after 100 d was reported by Salgado,[Citation1] while the division of the vascular pedicle 3 years after the transfer of a DIEP flap in a smoker, resulted in subtotal necrosis to Moolenburgh.[Citation5] As far as we know, this is the first report of a positive outcome following local recurrence excision with interruption of the vein outflow in a DIEP flap, 4 years after its transfer for breast reconstruction. As reported in the literature, it has been shown that infection, tumour and radiotherapy at wound beds may delay the process of neovascularisation,[Citation6,Citation7] as well as tobacco use [Citation5] and vascular insufficiency. In our patient, the non-smoking habit and lack of post-operative radiotherapy following quadrantectomy may have participated to the complete flap survival. Moreover, it has been demonstrated that the time lap necessary for neoangiogenesis is influenced by other factors, generally categorised as flap type and size.[Citation1,Citation3,Citation6] Perforator free flaps, such as DIEP, are more likely to survive pedicle injuries than those with a high metabolic rate, like muscolocutaneous flaps, depending also on the volume of transferred tissue.[Citation3] In our case, on one hand, the high contact surface between the flap and the recipient area, being almost totally buried under a SSM, may partially explain the flap survival by veins neoangiogenesis with the overlying breast skin. On the other hand, the mechanism of progressive venous congestion in DIEP flap remains unclear. As reported in the literature, the absence of venous connection across the midline, size of SIEV and small satellite veins perforators have been all implicated in the cause of venous outflow difficulties.[Citation8] However, in the clinical scenario of pedicle avulsion during secondary surgery, different considerations should be made. In our report, the local recurrence excision might lead to the followings vein outflow patterns. It may have damaged the SIEV and both the two DIEV comitantes in the pedicle or after the joining into a single DIEV, hence with complete interruption of the main pedicle venous outflow; or it may have been severed the SIEV and only one of the two DIEV comitantes, and vein flow could still occur by communicating branches between the comitantes before joining into a single DIEV. The 5 d lasting severe venous congestion of the overlying breast skin may orientate towards a complete vein drainage interruption followed by a slowly but complete flap recovery, most likely due to vein shunts opening with the recipient bed. Even if some instrumental reports have shown no reliable indication of sufficient perfusion from the surrounding tissue,[Citation9,Citation10] our case suggests that after a long-term total vein outflow interruption, a buried DIEP flap may undergo to complete survival thanks to a reliable process of neoangiogenesis.
Table 1. Literature review of vascular pedicle avulsion in autologous free flaps breast reconstruction (without anastomosis salvage procedure).
Disclosure statement
The authors declare that they have no conflict of interest.
References
- Salgado CJ, Smith A, Kim S, et al. Effects of late loss of arterial inflow on free flap survival. J Reconstr Microsurg. 2002;18:579–584.
- Heymans O, Lemaire V, Preud'Homme L, et al. Free flap pedicle loss: clinical study on 8 cases]. Ann Chir Plast Esthet. 2003;48:205–210.
- Moolenburgh SE, van Huizum MA, Hofer SO. DIEP-flap failure after pedicle division three years following transfer. Br J Plast Surg. 2005;58:1000–1003.
- Chubb D, Rozen WM, Ashton MW. Early survival of a compromised fasciocutaneous flap without pedicle revision: monitoring with photoplethysmography. Microsurgery. 2010;30:462–465.
- Enajat M, Rozen WM, Whitaker IS, et al. How long are fasciocutaneous flaps dependant on their vascular pedicle: a unique case of SIEA flap survival. J Plast Re-constr Aesthet Surg. 2010;63:e347–e350.
- Mucke T, Wolff KD, Rau A, et al. Autonomization of free flaps in the oral cavity: a prospective clinical study. Microsurgery. 2012;32:201–206.
- Kumar K, Jaffe W, London NJM, et al. Free flap neovascularization: myth or reality? J Reconstr Microsurg. 2004;20:1.
- Figus A, Wade RG, Gorton L, et al. Venous perforators in DIEAP flaps: an observational anatomical study using duplex ultrasonography. J Plast Reconstr Aesthet Surg. 2012;65:1051–1059.
- Heitland AS, Markowicz MP, Koellensperger E, et al. Early and long-term evaluation of perfusion changes in free DIEP-flaps for breast reconstruction via IC-view and duplex ultrasound: autonomous or peripheral perfusion? J Reconstr Microsurg. 2009;25:139–146.
- Machens HG, Mailänder P, Pasel J, et al. Flap perfusion after free musculocutaneous tissue transfer: the impact of postoperative complications. Plast Reconstr Surg. 2000;105:2395–2399.

