Abstract
We present a case in which a depot triamcinolone acetonide (Kenacort) was unintentionally injected intra-arterially into the ulnar artery, resulting in microembolic capillary occlusion in the digits supplied by the artery. Ischemic changes and subungual petechial hemorrhages were seen in the ulnar three digits. Angiography confirmed microembolic occlusion. The patient was treated with systemic vasodilative agents and a brachial plexus blockade. Tissue necrosis did not develop, however, the patient suffered lasting cold intolerance in the affected digits. Steroid suspension particles injected to treat CTS or other indications, can cause capillary occlusion and thereby microembolic tissue ischemia if injected intra-arterially. Choosing the right injection site and aspirating prior to injection is a simple though effective and indispensable measure to help prevent intra-arterial injection of steroid suspensions.
Introduction
Local steroid injection and surgical decompression have been shown to be highly effective in alleviating carpal tunnel syndrome (CTS) symptoms at three to twelve months follow-up [Citation1]. However, long-term results are better with surgical treatment [Citation1,Citation2]. Steroid injection is an attractive treatment option since it has very few adverse effects and does not require a recovery period as with surgical decompression.
We present a patient with digital ischemia and signs of micro-embolisms in the ulnar artery outflow area after steroid injection for CTS.
Case report
A 51-year old woman presented at the neurology department with typical but mild bilateral electromyography positive CTS. Immediately after injecting both carpal tunnels with 1 mL triamcinolone acetonide 10 mg/mL (Kenacort; Bristol-Myers Squibb, Netherlands), the left hand turned pale white. After 30–45 min the hand color returned close to normal. However, the ulnar three fingers stayed marbled and cold. Several hours later the patient was sent to the emergency room under suspicion of finger ischemia.
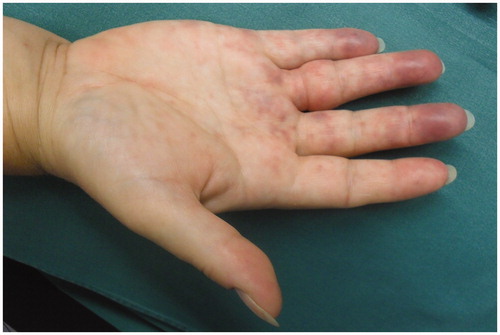
Physical examination showed a patchy blue discoloration, mainly of the ulnar digits (). The affected fingers were painless but cold and capillary refill was very slow compared to the other hand. Both the radial and ulnar artery had a normal pulse. The Allen-test revealed good patency of both arteries, although ulnar artery refill was mainly seen in the thumb and index finger. All fingers had normal sensibility.
Figure 1. Marbled ischemic aspect of ulnar three digits. Injection site visible proximal to wrist crease.
Considering possible vasospasm after intra-arterial injection of a steroid suspension, the patient was admitted and treated with a brachial plexus catheter containing bupivacain to achieve optimal vasodilatation. The following day neither increased ischemia, nor signs of tissue loss were seen. Since angiography was not expected to change the treatment at that stage, no further imaging was performed. The patient was discharged with oral acetylsalicylic acid.
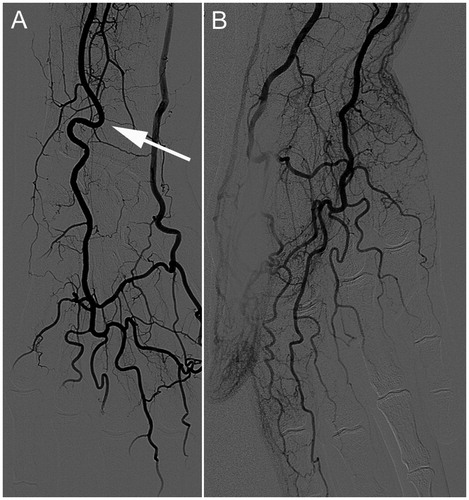
After two weeks the patient complained mainly of an intense cold-intolerance of the affected fingers. The marbled aspect of the fingers was unchanged. However, closer inspection of the nails showed massive splinter hemorrhages in the ulnar three digits (). An angiography was performed to rule out an active cause of micro-embolism. This showed a curved aspect of the ulnar artery at the level of the distal radio-ulnar joint (DRUJ) (). No aneurysmatic changes or vascular wall irregularities were identified, but decreased contrast filling of the digital arteries of the ulnar three fingers was obvious (). Some sudden stops distally in the digital arteries confirmed the assumption of microembolic occlusion by steroid particles. A carpal tunnel release was performed several months after the event. With cold intolerance as the only lasting complaint, the patient was discharged from further follow-up.
Discussion
Complications of steroid injection for CTS are few and usually mild. The most common side effects are pain and irritation at the injection site, infection and skin changes. However, median nerve damage after intraneural injection and tendon ruptures have been reported as well [Citation3,Citation4]. Two cases have been published with similarities to our patient. Armstrong mentions a patient who developed ‘an acute sympathetic reaction after steroid injection, causing a cool, pale hand’. This reaction resolved completely after twenty minutes [Citation5]. Payne described a patient with coolness and loss of coloration of the entire hand after steroid injection for CTS. These symptoms resolved also within twenty minutes. At follow-up coolness of the hand, mild blotchiness, subungual petechial hemorrhages and subcutaneous ecchymoses were noted. The consulted vascular medicine specialist suggested the phenomenon to be secondary to showering of small steroid particles into the hand’s arterial circulation, the authors remain unsure about the cause of the symptoms [Citation5].
Steroid injections for diagnostic cervical nerve-root blockade have led to extremely serious complications. Brouwers and Rosenkranz both describe patients suffering cervical anterior spinal artery syndrome due to extensive spinal cord infarction following steroid injection [Citation6,Citation7]. Precautions were taken, including attempts to aspirate before injection.
The authors mention several possible causes of the symptoms, including arterial occlusion due to vascular wall dissection, vasospasm, mechanical compression by the injected fluid volume, or accidental intra-arterial injection.
Even though the package insert explicitly discourages intravascular use, injected steroid suspensions will always yield the risk of being injected into a vascular lumen. If so, the suspension particles will inevitably float downstream toward the capillary microcirculation. Capillary luminal diameter is 7–9 μm, which is close to the average erythrocyte diameter (7.2 μm). Particle size according to the Certificate of Analysis of triamcinolone acetonide (Kenacort-10/-40) varies between ≤10 μm (≥20%), ≤20 μm (≥75%), ≤40 μm (≥95%), and ≤60 μm (≥99%). In other words: 80% of the particles is larger than 10 μm. Similar sizes were found by Tiso (63%≥10 μm) and Benzon (66% 0–20 μm) [Citation8,Citation9].
Consequently, intra-arterial injection of suspensions containing particles of this size will cause occlusion of capillaries and arterioles with diameters up to 40–60 μm. The clinical course of our patient strongly suggests microembolic ischemia by intra-arterially injected steroid particles. The impaired blood flow to the ulnar artery microcirculation, the subungual petechial hemorrhages in the ulnar digits, and the angiographic findings, substantiate this.
Although the effect of microembolic ischemia in hands and fingers is less devastating than in spinal cords, increased awareness of this possible complication is important. Extravasal positioning of the needle can be assured by choosing the optimal injection site [Citation10] and by aspirating before injecting. Most anatomy books show a straight course of the ulnar artery at wrist level. However, a curved course as seen in this case is very common. This makes the ulnar artery in particular prone to intra-arterial injection at the injection site.
In case of sudden digital ischemia following steroid injection for CTS, maximal vasodilatation should be achieved to optimize circulation. Administration of vasodilative agents or brachial plexus nerve blockade can be considered.
In conclusion, intra-arterial injection with corticosteroid suspensions can cause serious side effects due to microembolic capillary occlusion by steroid particles. Injections for CTS should be administered at the optimal injection site, with specific assurance of extravasal positioning.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ly-Pen D, Andreu JL, de Blas G, et al. Surgical decompression versus local steroid injection in carpal tunnel syndrome: a one-year, prospective, randomized, open, controlled clinical trial. Arthritis Rheum. 2005;52(2):612–619.
- Verdugo RJ, Salinas RA, Castillo JL, et al. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev. 2008:Cd001552.
- Frederick HA, Carter PR, Littler JW. Injection injuries to the median and ulnar nerves at the wrist. J Hand Surg. 1992;17(4):645–647.
- Gottlieb NL, Riskin WG. Complications of local corticosteroid injections. JAMA. 1980;243(15):1547–1548.
- Armstrong T, Devor W, Borschel L, et al. Intracarpal steroid injection is safe and effective for short-term management of carpal tunnel syndrome. Muscle Nerve. 2004;29(1):82–88.
- Brouwers PJ, Kottink EJ, Simon MA, et al. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91(3):397–399.
- Rosenkranz M, Grzyska U, Niesen W, et al. Anterior spinal artery syndrome following periradicular cervical nerve root therapy. J Neurol. 2004;251(2):229–231.
- Benzon HT, Chew TL, McCarthy RJ, et al. Comparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroids. Anesthesiology. 2007;106(2):331–338.
- Tiso RL, Cutler T, Catania JA, et al. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004;4(4):468–474.
- Kay NR, Marshall PD. A safe, reliable method of carpal tunnel injection. J Hand Surg. 1992;17(6):1160–1161.