Abstract
We recently treated a patient who presented with a hyperpigmented longitudinal stripe of the thumb nailbed which was biopsied with a histopathologic diagnosis of onychopapilloma. We have not seen onychopapilloma reported in the hand surgery literature. Onychopapilloma is generally benign but a malignant variant has recently been reported.
Introduction
Plastic surgeons and hand surgeons may, from time to time, see patients with a longitudinal pigmented stripe (also called a band or streak) on the nailbed. Most of these lesions are benign – most, but not all. These lesions are often biopsied and often should be biopsied, to provide a pathologic diagnosis. Recently, a patient underwent a biopsy of a nail bed lesion which was reported as onychopapilloma. We have not seen a description of onychopapilloma in the hand surgery literature.
Case report
A 48-year-old male presented for evaluation of a hyperpigmented longitudinal stripe on his right thumb nailbed. The lesion had been present for about 5 years. He reported no recent change in appearance. He denied pain and denied previous trauma. He had been seen by a dermatologist who made a diagnosis of longitudinal melanonychia. There was a history of melanoma at the contralateral forearm, excised, without recurrence. On physical examination, there was an approximately two-millimeter-wide dark stripe beginning at about the distal edge of the lunula extending distally (). There was a slight ridge in the nail plate but no loss of adherence.
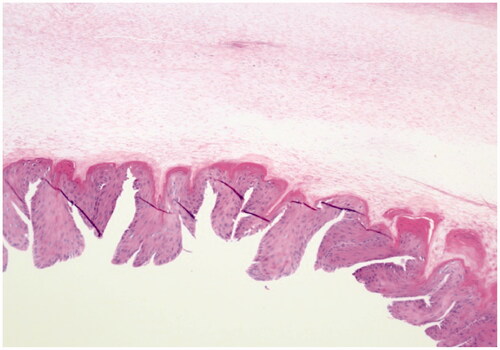
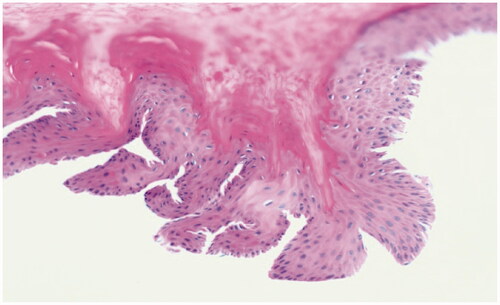
A punch biopsy was performed using a commercially available disposable biopsy punch (Integra York PA Inc. York PA, USA). A 3 mm diameter specimen was obtained from the proximal portion of the lesion, including the nail plate and underlying matrix. On microscopic examination, the tumor was characterized by papillomatous proliferation of epithelial cells characterized by ovoid bland nuclei showing smooth chromatin and eosinophilic cytoplasm, indicative of matrix metaplasia, arranged along with thickened fibrovascular cores with subungual layered hyperkeratosis ( and ). A diagnosis of onychopapilloma was made.
Discussion
In 1995 Baran & Perrin reported 4 cases in which they observed the presence of multi-nucleate cells in localized distal subungual keratosis [Citation1]. In 2000, the same authors presented additional cases with similar findings and recommended ‘onychopapilloma’ as the diagnostic term [Citation2].
Authors since then have noted that onychopapilloma is ‘uncommon’ [Citation3,Citation4] and ‘rare’ [Citation5]. Indeed, a recent pub med search for ‘onychopapilloma’ yielded 27 results, none in the orthopedic literature, all in dermatology journals. Onychopapilloma is a benign lesion of the nail bed, typically presenting as longitudinal chromonychia (abnormal color of the nail plate or underlying matrix), involving one digit [Citation5–7].
Most cases of onychopapilloma present with longitudinal erythronychia (red streak in the nail) [Citation8]. Halteh et al. noted that onychopapilloma is the most common cause of localized (single digit) longitudinal erythronychia [Citation9]. Onychopapilloma can also present as longitudinal leukonychia (white stripe) [Citation4] or longitudinal melanonychia (brown or black) [Citation6]. There is often a corresponding longitudinal groove in the nail plate. Tosti et al. reported that onychopapilloma can present with splinter hemorrhages without any obvious band or stripe. There may be a distal focal subungual keratotic mass and/or distal onycholysis (loss of nail plate adherence) [Citation7].
As recently as 2018 Kim et al. noted that the pathogenesis of onychopapilloma is not fully understood but that it appeared to involve the distal matrix and therefore they suggested that band sparing of the proximal nail (absence of the lesion proximally) is a characteristic feature of onychopapilloma [Citation10]. Differential diagnosis includes nevus, melanoma, lichen planus, traumatic subungual hematoma, glomus tumor, squamous cell carcinoma in situ basal cell carcinoma, wart [Citation5,Citation7,Citation11–13].
A definitive diagnosis is made via biopsy. When to biopsy and when to observe a longitudinal chromonychia can be influenced by several factors. A painful lesion merits the discovery of an underlying cause. Much longitudinal chromonychia is painless however, Jellinek, in a discussion of localized (single digit) longitudinal erythronychia, stated that biopsy ‘should be considered’ for any ‘evolving’ or ‘changing’ or new band [Citation13]. Good advice regardless of the color of the lesion and especially so for a brown or black band (melanonychia) where there is a risk of melanoma. If a biopsy of the lesion or surgical excision is deferred, then careful documentation of findings, including photographs, with regular follow-up is advised [Citation13]. Peri-ungual extension of pigment from a longitudinal melanonychia onto the proximal or lateral nail folds – Hutchinson sign – can indicate melanoma and would warrant a biopsy.
Recently, Haneke et al. reported a malignant variant of onychopapilloma in a 58-year-old male with a longitudinal erythronychia of the thumbnail, initially painless, who underwent biopsy after developing pain associated with the lesion. The authors were unable to determine whether their finding was the result of malignant degeneration of a previously benign onychopapilloma or a primary malignant onychopapilloma [Citation14].
Conclusion
Onychopapilloma is a cause of longitudinal chromonychia, generally involving one digit. It most often presents as erythronychia but can present as leukonychia, or as melanonychia, as was the case for our patient. While onychopapilloma is benign, a malignant variant has recently been reported. The differential diagnosis of longitudinal chromonychia includes malignancies so a biopsy is often warranted. To the best of our knowledge, onychopapilloma has not been reported in the plastic surgery or hand surgery literature. Since ‘the eye does not see what the mind does not know’, awareness of this entity may be helpful, especially given the recent description of a malignant variant.
Ethics approval
Informed consent was obtained from all patients for being included in the study. This article does not contain any studies with animal subjects.
Author contributions
SHK evaluated the patient, performed the surgery, and was major contributor in the writing of the manuscript. RD evaluated the patient and contributed in the writing of the manuscript. BB performed the histological examination and contributed to the writing of the manuscript.
Acknowledgment
The authors recognize the assistance of Haben Berihun B.S. who assisted in the review and preparation of this manuscript.
Disclosure statement
The authors declare that there is no conflict of interest regarding publication of this article.
References
- Baran R, Perrin C. Localized multinucleate distal subungual keratosis. Br J Dermatol. 1995;133(1):77–82.
- Baran R, Perrin C. Longitudinal erythronychia with distal subungual keratosis: onychopapilloma of the nail bed and Bowen's disease. Br J Dermatol. 2000;143(1):132–135.
- Tambe SA, Ansari SMM, Nayak CS, et al. Surgical management of onychopapilloma, onychomatricoma, and subungual osteochondroma: case series. J Cutan Aesthet Surg. 2018;11(3):143–147.
- Criscione V, Telang G, Jellinek NJ. Onychopapilloma presenting as longitudinal leukonychia. J Am Acad Dermatol. 2010;63(3):541–542.
- Schneider S, Ramirez M, Miteva M, et al. The many faces of onychopapilloma. J Am Acad Dermatol. 2015; 72(suppl 1):AB116.
- Miteva M, Fanti PA, Romanelli P, et al. Onychopapilloma presenting as longitudinal melanonychia. J Am Acad Dermatol. 2012;66(6):e242–e243.
- Tosti A, Schneider SL, Ramirez-Quizon MN, et al. Clinical, dermoscopic, and pathologic features of onychopapilloma: a review of 47 cases. J Am Acad Dermatol. 2016;74(3):521–526.
- de Berker DA, Perrin C, Baran R. Localized longitudinal erythronychia: diagnostic significance and physical explanation. Arch Dermatol. 2004;140(10):1253–1257.
- Halteh P, Magro C, Scher RK, et al. Onychopapilloma presenting as leukonychia: case report and review of the literature. Skin Appendage Disord. 2017;2(3-4):89–91.
- Kim M, Sun EY, Jung HY, et al. Onychopapilloma: a report of three cases presenting with various longitudinal chromonychia. Ann Dermatol. 2016;28(5):655–657.
- Elharrouni Alaoui A, Kh I, Gellouj S, et al. Subungual Bowen disease simulating onychopapilloma: case report. J Case Rep Clin Images. 2019; 2:1029.
- Cohen PR. Longitudinal erythronychia: individual or multiple linear red bands of the nail plate: a review of clinical features and associated conditions. Am J Clin Dermatol. 2011;12(4):217–231.
- Jellinek NJ. Longitudinal erythronychia: suggestions for evaluation and management. J Am Acad Dermatol. 2011;64(1):167.e1–167.11.
- Haneke E, Iorizzo M, Gabutti M, et al. Malignant onychopapilloma. J Cutan Pathol. 2021;48(1):174–179.