Abstract
Two cases are presented that demonstrate normal wound healing following bilateral reduction mammoplasty, in young female patients taking therapeutic doses of Isotretinoin (Roaccutane). Review of the literature does not provide evidence that Isotretinoin impairs would healing, nor that it promotes hypertrophic or keloid scarring in surgical patients.
Introduction/background
Conventional surgical dictum warns against surgical procedures while a patient is taking Roaccutane (Isotretinoin), and for a period after it is ceased. The authors experience is that advice varies greatly from the prescribing Dermatologists, regarding what this period should be. This caution is due to the fear of the adverse effect Roaccutane may have upon connective tissue metabolism, and subsequently wound healing. Retinoids have been shown to suppress collagenase activity [Citation1], which may lead to excess collagen accumulation and hence produce hypertrophic and keloid scarring.
An extensive review of the literature fails to identify support for this approach, with a lack of clinical series that prove an adverse effect of Roaccutane upon healing in surgery relevant to Plastic Surgery, i.e. incisional open surgery. Similarly, there are no high quality studies definitively proving its safe use.
We present two cases of bilateral reduction mammoplasty in young females, performed on therapeutic doses of Roaccutane, who went onto healing without issue. These cases represent very valuable experience that open surgery can be performed safely with satisfactory scar outcomes, while the patient is taking Roaccutane, if clinical circumstances dictate a need for timely surgery. The available limited relevant literature will be reviewed.
Case presentation
Patient 1
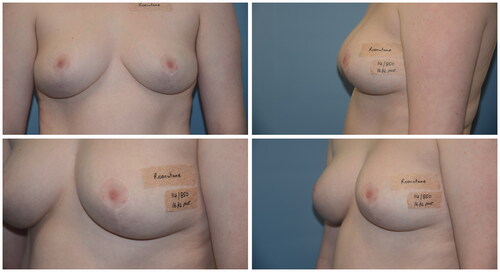
A 19-year-old female trainee nurse wished to have breast reduction surgery due to neck and shoulder pain. She suffered polycystic ovarian syndrome and cystic acne but was otherwise healthy. She had no personal or family history of keloid and hypertrophic scarring. Her breasts were disproportionate for her general body habitus (12 F, 167 cm, 72 kg). The patient began therapeutic Roaccutane 2 months prior to her bilateral reduction mammoplasty, and continued until four and a half months after her surgery. Her scars healed well with minimal hypertrophic scarring on the right areola. At 9 months follow up, her scars had softened and the patient was pleased with their outcome (see ).
Patient 2
A 17-year-old female wished to have breast reduction surgery as she complained of neck and shoulder pain, recurrent cysts in her cleavage and difficulty exercising. She was very self conscious of her appearance. She suffered cystic acne but was otherwise healthy. She had no personal or family history of keloid and hypertrophic scarring. Her breasts were disproportionate for her general body habitus (12 F, 178 cm, 75 kg). The patient was under psychiatric care, and had attempted self harm due to poor self esteem. The patient began Roaccutane two and a half months prior to her bilateral reduction mammoplasty which continued at follow up 16 months post operatively. Her scars healed normally and the patient was pleased with their outcome. Her mother believed the surgery had ‘saved her life’ (see ).
Literature review
We searched PubMed from inception until 14 March 2019 using the terms ‘isotretinoin’ AND ‘surgery’ AND ‘wound healing’. This review focuses on open/incisional procedures rather than dermatological procedures (dermabrasion, laser therapy, etc.) which account for the majority of the literature on this topic, and have recently been well covered elsewhere [Citation2,Citation3]. To summarise these systematic reviews, there is insufficient evidence to support delaying the majority of dermatological procedures (including laser hair removal, manual dermabrasion, non-ablative laser therapy, superficial chemical peel). However, there is evidence to support delaying mechanical dermabrasion and fully ablative laser therapy in this setting.
This left a small number of papers concentrating on cutaneous surgery. These covered a broad range of procedures including cosmetic procedures (rhinoplasty, blepharoplasty, fat transfer, liposuction, face lift, punch elevation, subcision), full thickness skin graft, non-melanoma skin cancer excisions, punch biopsy, dental extraction and arthroscopy.
The available randomised control trials (RCTs) were not specific to incisional wounds, leaving small cohort sizes. A 1984 dose safety RCT documented two patients who underwent otolaryngolical surgery with normal recovery [Citation4]. Another patient in this study reported slow wound healing but no further information is given. A RCT focusing on Roaccutane combined with anti-ageing cosmetic procedures demonstrated no difference in wound healing between the 39 Roaccutane patients and the 39 control patients with the same procedures [Citation5].
Cohort studies comprise the bulk of the literature. Of note is a prospective cohort study of 29 immunosuppressed patients taking acitretin (a second generation retinoid) undergoing removal of non-melanoma skin cancers [Citation6]. Wounds were closed with simple layered closure, full thickness skin graft, flaps or allowed to heal by secondary intention. There was no significant difference between groups in terms of the end points of infection, hypertrophic scarring, hypertrophic granulation tissue and dehiscence. However, this group is not representative of the usual patient group taking Roaccutane (young, otherwise well acne patients) and this may impact their propensity to adverse scarring.
A 2012 retrospective cohort study focused on mucosal healing following wisdom tooth extraction [Citation7]. About 26 patients who were taking or had recently ceased (within 1 month) Roaccutane, who had wisdom tooth extraction, had higher rates of alveolar osteitis, however all patients demonstrated otherwise normal mucosal healing. Lack of statistical power and incomplete data collection in the study makes it difficult to demonstrate a causal link between Roaccutane and dry sockets. A more recent prospective cohort study featured a subgroup analysis of 20 patients who demonstrated normal healing with cutaneous surgery including excision, subcision, biopsy, punch elevation and dental extraction [Citation8].
Case series and reports are largely in agreement with the above. However, a retrospective case series of three patients receiving rhinoplasty and post-operative use of Roaccutane demonstrated nasal tip deformities up to 2 years post operatively and within 6 months of starting Roaccutane [Citation9]. Case reports of excisions for pilonidal abscess, hidradenitis suppurativa, lip abscess and genital warts demonstrate normal healing through primary or secondary intention [Citation10–13].
Recent systematic reviews have also attempted to collate the available evidence. The recent consensus recommendation from an American group of dermatologists and plastic surgeons was that there is insufficient evidence to support delaying cutaneous surgery for patients on Roaccutane [Citation3]. A systematic review and case report from a group in the United Kingdom found the power of the available evidence was poor, particularly for operations other than otolaryngeal and maxillofacial, and suggested there is some doubt that Roaccutane impairs wound healing [Citation2]. Muscle flaps and Roaccutane use may be an area for further research as there was some evidence of skeletal muscle necrosis.
There are of course considerations beyond the cosmetic results of surgical procedures. A 2016 paper suggests it is safe to operate on patients taking Roaccutane after systematic review of its effects on coagulation, liver function, renal function, arrhythmias, infection and wound healing [Citation14].
Discussion
Despite being a widely prescribed drug, Roaccutane has been poorly studied. The surgical dictum of avoiding surgery whilst on Roaccutane nevertheless persists. It appears to have first emerged in the mid-1980s from case series of patients with either delayed healing or keloid scarring following dermatological procedures [Citation15]. This restriction has become increasingly relevant as Roaccutane has become more widely used.
The Australian Medicines Handbook (AMH) [Citation16] makes no mention of precautions with surgical procedures, whilst MIMS [Citation17] advises against waxing, dermabrasion and laser therapy. The consumer medicine information (for patients) [Citation18] and product information (for healthcare professionals) [Citation19] from the Australian supplier of Roaccutane both recommend avoiding waxing, dermabrasion and laser treatment. None of these resources make mention of avoiding cutaneous surgery. This would align with the presented evidence and recommendations from the systematic reviews [Citation2,Citation3], however is at odds with common practice.
The available evidence presented above would suggest that it is unlikely that Roaccutane significantly impairs wound healing, nor facilitates over production of scar. This however, is not founded in levels of evidence that negate the need for open disclosure with the patient surrounding potential adverse effects of their intended surgery, particularly if cosmetic. This is certainly the case in surgery outside of maxillofacial and head & neck surgery. Some patients, regardless of medications, personal and family history, will heal with hypertrophic or keloid scars. In the setting of Roaccutane use it is important to clarify these issues with patients, and appropriately warn.
The two patients in this case series are presented as evidence of outcome following incisional breast surgery in the presence of therapeutic Roaccutane. These patients underwent surgery leading to long scar lines and continued on Roaccutane throughout the perioperative period, and for months post operatively. Wound healing in these patients was within the ‘normal range for this operation, which is considered to have a propensity for hypertrophic scarring. There was a small amount of hypertrophic scarring in one patient which settled within the anticipated normal period. Whilst this study is limited by admittedly small numbers, these cases add important precedence to the literature that incisional surgery can occur whilst on Roaccutane. It remains important however to counsel patients that scarring is a complex process and there are patient and operative factors (including wound tension, infection, haematoma, location) that will predispose to abnormal scarring despite the safety of roaccutane.
Conclusions
Roaccutane is a commonly encountered medication in modern surgical practice. Long held beliefs that caution against its continued administration in the perioperative period are not based in evidence. This unfounded caution may needlessly delay patient surgery. These cases invite a critical appraisal of this dictum in the context of the available evidence and are the first cases reported in the literature for breast surgery performed while taking Roaccutane. As always, these cases challenge us to test aphorisms against the available scientific data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Abergel RP, Meeker CA, Oikarinen H, et al. Retinoid modulation of connective tissue metabolism in keloid fibroblast cultures. Arch Dermatol. 1985;121(5):632–635.
- Wootton C, Cartwright R, Manning P, et al. Should isotretinoin be stopped prior to surgery? A critically appraised topic. Br J Dermatol. 2014;170(2):239–244.
- Spring LK, Krakowski AC, Alam M, et al. Isotretinoin and timing of procedural interventions: a systematic review with consensus recommendations. JAMA Dermatol. 2017;153(8):802–809.
- Bruno N, Beacham B, Burnett J. Adverse effects of isotretinoin therapy. Cutis. 1984;33(5):484–486.
- Hernandez‐Perez E, Khawaja HA, Alvarez TYM. Oral isotretinoin as part of the treatment of cutaneous aging. Dermatol Surg. 2000;26(7):649–652.
- Tan SR, Tope WD. Effect of acitretin on wound healing in organ transplant recipients. Dermatol Surg. 2004;30(4 Pt 2):667–673.
- Sharma J, Thiboutot D, Zaenglein A. The effects of isotretinoin on wisdom tooth extraction. J Am Acad Dermatol. 2012;67(4):794–795.
- Mahadevappa OH, Mysore V, Viswanath V, et al. Surgical outcome in patients taking concomitant or recent intake of oral isotretinoin: a multicentric study-ISO-AIMS study. J Cutan Aesthet Surg. 2016;9(2):106–114.
- Allen BC, Rhee JS. Complications associated with isotretinoin use after rhinoplasty. Aesthetic Plast Surg. 2005;29(2):102–106.
- Griffiths W. Wound healing and the retinoids. Retinoids Today Tomorrow. 1986;4:26.
- Larson DL, Flugstad NA, O'Connor E, et al. Does systemic isotretinoin inhibit healing in a porcine wound model? Aesthet Surg J. 2012;32(8):989–998.
- Huoh KC, Chang KW. Lip abscess associated with isotretinoin treatment of acne vulgaris. JAMA Dermatol. 2013;149(8):960–961.
- Yew YW, Pan JY. Complete remission of recalcitrant genital warts with a combination approach of surgical debulking and oral isotretinoin in a patient with systemic lupus erythematosus. Dermatol Ther. 2014;27(2):79–82.
- Ungarelli LF, Hetem CMC, Junior JAF. Is it safe to operate on patients taking isotretinoin? Aesthetic Plast Surg. 2016;40(1):139–148.
- Rubenstein R, Roenigk HH, Jr., Stegman SJ, et al. Atypical keloids after dermabrasion of patients taking isotretinoin. J Am Acad Dermatol. 1986;15(2 Pt 1):280–285.
- Australian Medicines Handbook Pty Ltd. Isotretinoin. 2019. [cited 2019 Mar 19].
- MIMS Australia Pty Ltd. APO-Isotretinoin product information. 2018. [cited 2019 Mar 19].
- Roaccutane Consumer Medicine Information. 2018. [cited 2019 May 19]. Availble from: http://www.guildlink.com.au/gc/ws/ro/cmi.cfm?product=rocroacc10413.
- Australian Product Information, Roaccutane (Isotretinoin). 2018. [cited 2019 Mar 19]. Availble from: http://www.guildlink.com.au/gc/ws/ro/pi.cfm?product=roproacc10413.