Abstract
A case study of a 71-year-old man with a giant cutaneous squamous cell carcinoma of the scalp and calvaria is presented, where a combination of surgical excision, reconstruction with a latissimus dorsi muscular free flap, immunotherapy, and radiotherapy were used to control the disease for two years without recurrence.
Introduction
Non-melanoma skin cancers are the most prevalent form of cancer, with cutaneous squamous cell carcinoma being the second most common type. Squamous cell carcinomas are generally treated by surgical excision, Mohs surgery, or electrodessication and curettage. Non-surgical options also exist, and include Photodynamic Therapy, topical or systemic chemotherapy, radiotherapy and immunotherapy [Citation1]. There is no universal agreement on the definition of locally advanced disease, and accurate staging and risk stratification for patients can be challenging. Patients with advanced cSCC are often deemed ineligible for either or both curative surgery and radiation therapy and, until recently, were limited to off-label systemic cisplatin-fluorouracil or cetuximab therapy, which offers modest clinical benefits and potentially severe toxicity [Citation2]. A new systemic therapy, cemiplimab, has been approved to treat locally advanced and metastatic cSCC. Its use is safe and effective and needs to be considered as a first-line treatment in such cases. The clinical case of a man with an aggressive, giant squamous cell carcinoma of the scalp and calvaria is reported. Demolitive surgery and reconstruction with a latissimus dorsi muscular free flap were performed, followed by other therapeutic modalities. The combination of these different therapeutic approaches allowed us to control the disease for up to two years without evidence of recurrence and residual disease. Different therapeutic modalities have been adopted to address a case that went further than the outline of the standard guidelines. A few cases in the literature [Citation3] reported the combination of antiPDL-1, radiotherapy, and surgery. No cases applied a combination of all these modalities to keep the neoplasm under control and bring the patient to further radical surgery. We report the case of a patient where the use of these therapies, in a non-schematic sequence, due to the patient’s clinical conditions, was able to achieve control of the disease.
Case presentation
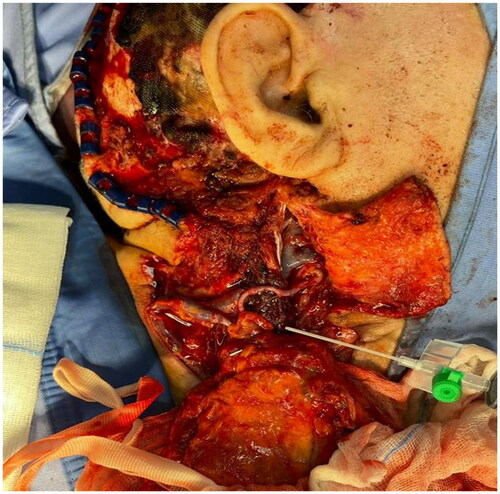
A 71-year-old patient was referred to our unit for an aggressive squamous cell carcinoma of the scalp in the parieto-mastoid area (). The tumor presented as an enormous nodular ulcerated lesion measuring 17 cm cranio-caudally and 11 cm antero-posteriorly. Assessment of the lesion through a contrast-enhanced magnetic resonance showed a maximum thickness of 5 cm and bone erosion. The lesion was infiltrating the underlying bone structures, the external theca, the diploe, and the internal theca for 2.5 cm at the level of the sigmoid sinus in the temporo-occipital place, and the external theca and diploe at the level of the angular gyrus in the parietal place. The ulcerated right parieto-mastoid tumoral burden presented necrotic areas and a vegetative appearance. The case was discussed collegially during the Head and Neck Multidisciplinary Team presented by the Plastic and Reconstructive Surgery Unit. As the patient has been recently admitted to the Internal Medicine Unit because of fever and asthenia, antibiotic therapy was started, and a surgical approach was defined. Combined resection and reconstruction surgery were planned with the Neurosurgery colleagues even if surgical radicality was not certain. Neurosurgeons, Plastic and ENT Surgeons performed the combined surgery. The neurosurgical team first removed the tumoral mass, and performed right parietal craniotomy and mastoidectomy. Tumor removal was almost complete. The dural plane was intact, and a minute neoplastic spot infiltrating the transverse sinus was evident and left in situ (). Afterward, the ENT colleagues performed a right latero-cervical node clearance, and the plastic surgeons reconstructed the defect. A latissimus dorsi free muscular flap was harvested, the skin island measured 16 × 6 cm and a 12 cm peduncle was dissected up to the intersection with the axillary artery cutting off the lateral circumflex artery of the scapula [Citation4,Citation5].
Anastomoses were performed between the subscapular artery and the superior thyroid artery and between the subscapular vein and the external jugular vein (). The tissue defect was covered with the latissimus dorsi free flap, and a partial thickness skin graft was taken from the right thigh [Citation6,Citation7]. Anatomopathological reports were consistent with moderately differentiated, ulcerated, infiltrating, G2 squamous cell carcinoma. The neoplasm was reaching the lower margin of surgical excision. One out of 51 lymph nodes of dissection was positive for metastasis. At the postoperative CT scan, the residual neoplasm was shown in the retro-auricular area. At this point, the patient was referred for radiotherapy consultation. He was not considered suitable for adjuvant radiotherapy because of severe depression and anxiety disorder. An indication was given to start immunotherapy with cemiplimab, a monoclonal antibody that belongs to the class of immune checkpoint inhibitors and has shown substantial antitumor activity in patients with metastatic and locally advanced cutaneous squamous cell carcinoma [Citation8]. The patient was started on six cycles of intravenous cemiplimab (350 mg every three weeks). After five months, a total body CT scan showed a tumoral residue posteriorly to the mandibular condyle measuring 105 × 58 x 48 mm in the cranio-caudal, transverse and anteroposterior diameters. After six months, a CT scan demonstrated reduced local recurrence with cemiplimab immunotherapy, and a brain MRI highlighted stable disease. One year after the surgery, following the clinical progression of the disease (), radiation therapy was exclusively indicated with concomitant cemiplimab therapy. At first, due to the extent of the disease and poor performance status, palliative radiation therapy was started with 45 Gy total (3 Gy in 15 fractions). However, at the end of the radiotherapy treatment, the clinical improvement that took place in the response did improve the performance status of the patient. Therefore, a second radiotherapy phase was delivered (2 Gy in 9 fractions, a total of 18 Gy) for a total of 45 Gy + 18 Gy. Overall, a total physical treatment of 63 Gy and an equivalent dose of 67 Gy (EQD2) were completed. Radiotherapy toxicity was reported, and a G3 actinic acute mucositis and a G2 mucositis accounted as side effects. A CT scan was performed and showed a partial response which, however, continued and even improved. Three months later, magnetic resonance of the facial skeleton revealed a further improvement of the lesion. Clinically, full response over the genial region skin was evident. However, a doubt of persistence in the retro-auricular region was present. An ulcerated nodular lesion of 2 cm diameter was present in the right retro-auricular region, and the plastic surgeon proceeded with surgical excision. Histology was negative for disease: ulcerated areas with extensive calcified deposits in the superficial and deep dermis accompanied by histiocytic giant cell reaction-like foreign body reaction were found. No residual evidence of disease was reported. At a two-year follow up the patient is still free from disease ().
Discussion
This case shows a dramatic response of an advanced cutaneous squamous cell carcinoma for whom there is no widely accepted standard of care using different therapeutic approaches. The use of cemiplimab allowed us to combine different therapeutic modalities and allowed us to address an excessive scalp tumor surgically. We could control an enormous neoplasm that could not have been managed in the past, before the availability and the possibility of combining all these therapeutic modalities. Tanvetyanon et al. [Citation9] used adjuvant radiation and adjuvant concurrent chemoradiation for patients with high-risk cutaneous SCCHN. They found that the use of concurrent adjuvant chemoradiation was associated with improved recurrence-free survival, mainly because of a reduction in the regional progression of the disease. In September 2018, the United States Federal Drug Administration approved cemiplimab for advanced cutaneous squamous cell carcinoma (cSCC) [Citation10]. It became thus possible to treat adult patients with metastatic or locally advanced cutaneous SCCHN that were not candidates for curative surgery or curative radiation therapy. In our case, the patient was followed up for one year and had a partial response to cemiplimab. After progression, a new Multidisciplinary Team evaluation gave indication to a radiation treatment, which further improved locoregional disease. Available evidence indicates that cutaneous SCCHN with high-risk features, including positive surgical margins, nodal involvement, and perineural or soft tissue invasion, can be effectively controlled by adjuvant radiation [Citation11]. Nevertheless, data indicate that treatment with surgery followed by adjuvant radiotherapy for high-risk patients still leaves room for improvement. For instance, Givi et al. [Citation12] reported 5-year survival ranges from 40% to 66% among patients with parotid or cervical node involvement. Radiotherapy is another important therapeutic modality, a safe and highly effective tool to address giant scalp tumors with extensive bone destruction [Citation13]. Our patient was initially not fit for this treatment, and cemiplimab allowed us to control the disease and take him to a partial response until he was eventually suitable to be irradiated [Citation14]. The combination of anti-PDL1 immunotherapy, radiation therapy, and surgery for cSCC has been previously described in the literature, but no neoplasm control and eradication cases have been described. Our case report shows how the possibility of combining and associating these different therapeutic modalities in a particular sequence allowed us to bring the patient to complete remission.
Conclusions
To our knowledge, our case report first showed how the combination of currently available therapeutic modalities has allowed us to keep a giant squamous cell carcinoma under control and eventually completely eradicate it. Two years after surgery, the patient is still alive with no evidence of disease. The choice and the sequence of treatments must be tailored to the individual patient, physician’s preferences and multidisciplinary team decisions.
Ethical approval and consent to participate
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
The participant has given written informed consent for publication.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Stratigos AJ, Garbe C, Dessinioti C, et al. European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: part 2. Treatment. Eur J Cancer. 2020; 128:83–102. Epub 2020 Feb 26. PMID: 32113942.
- Claveau J, Archambault J, Ernst DS, et al. Multidisciplinary management of locally advanced and metastatic cutaneous squamous cell carcinoma. Current Oncology. 2020;27(4):399–407.
- Schaffer M, Simonovich A, Livof A, et al. Use of cemiplimab in locally advanced cutaneous squamous cell carcinoma. Clin Case Rep. 2020;10:1–4.
- Trignano E, Fallico N, Nitto A, et al. The treatment of composite defect of bone and soft tissues with a combined latissimus dorsi and serratus anterior and rib free flap. Microsurgery. 2013;33(3):173–183. Epub 2013 Feb 25. PMID: 23436310.
- Chen HC, Fallico N, Ciudad P, et al. Latissimus dorsi-rib pedicle flap for mandibular reconstruction as a salvage procedure for failed free fibula flap. J Craniofac Surg. 2014;25(3):961–963. PMID: 24777023.
- Trignano E, Fallico N, Fiorot L, et al. Flap monitoring with continuous oxygen partial tension measurement in breast reconstructive surgery: a preliminary report. Microsurgery. 2018;38(4):402–406. Epub 2017 Nov 13. PMID: 29131393.
- Trignano E, Dessy LA, Fallico N, et al. Treatment of pectoralis major flap myospasms with botulinum toxin type a in head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2012; 65(2):e23-8–e28. Epub 2011 Nov 9. PMID: 22071458.
- Migden MR, Khushalani NI, Chang ALS, et al. Cemiplimab in locally advanced cutaneous squamous cell carcinoma: results from an open-label, phase 2, single-arm trial. Lancet Oncol. 2020; 21(2):294–305.
- Tanvetyanon T, Padhya T, McCaffrey J, et al. Postoperative concurrent chemotherapy and radiotherapy for high-risk cutaneous squamous cell carcinoma of the head and neck. Head Neck. 2015;37(6):840–845.
- Ahmed SR, Petersen E, Patel R, et al. Cemiplimab-rwlc as first and only treatment for advanced cutaneous squamous cell carcinoma. Expert Rev Clin Pharmacol. 2019;12(10):947–951.
- Wang JT, Palme CE, Morgan GJ, et al. Predictors of outcome in patients with metastatic cutaneous head and neck squamous cell carcinoma involving cervical lymph nodes: improved survival with the addition of adjuvant radiotherapy. Head Neck. 2012;34(11):1524–1528.
- Givi B, Andersen PE, Diggs BS, et al. Outcome of patients treated surgically for lymph node metastases from cutaneous squamous cell carcinoma of the head and neck. Head Neck. 2011;33(7):999–1004.
- Gruber I, Koelbl O. Dramatic radiotherapy response of a giant T4 cutaneous squamous cell carcinoma of the scalp with extensive bone destruction: a case report. J Med Case Reports. 2021;15(1):610.
- Likhacheva A, Awan M, Barker CA, et al. Definitive and postoperative radiation therapy for basal and squamous cell cancers of the skin: executive summary of an American society for radiation oncology clinical practice guideline. Pract Radiat Oncol. 2020;10(1):8–20.