Abstract
Liposarcomas are rare, malignant tumors of adipocyte differentiation. Surgery is the main treatment method. We are reporting a rare case of a 65- year- old female patient with a massive dedifferentiated thigh liposarcoma that was growing for 10 years and spread to the retroperitoneum.
Background
Liposarcomas are malignant tumors of adipocyte differentiation [Citation1,Citation2]. According to the most recent World Health Organization classification, liposarcomas are divided into five categories: well differentiated (which includes adipocytic, sclerosing and inflammatory subtypes), dedifferentiated, myxoid, pleomorphic and myxoid pleomorphic [Citation2,Citation3]. Liposarcomas are rare tumors with an incidence of approximately 1 per 100,000 persons a year, but they are also among common (20%) soft tissue sarcomas [Citation4,Citation5]. They can be found anywhere in the body, but the most common site for liposarcomas is in the extremities, followed by the retroperitoneum [Citation1]. The recurrence rate, the risk of distant metastases and survival mostly depend on the histological type of liposarcoma [Citation1,Citation6]. Magnetic resonance imaging is the main imaging modality, and histopathological assessment of tissue sample obtained by biopsy technique is required to obtain a definitive diagnosis [Citation7]. Surgical excision is the main treatment option for most liposarcomas. The standard surgical procedure is en bloc excision with a R0 margin. Adjuvant radiotherapy and/or chemotherapy may be required for high-grade lesions [Citation1,Citation7].
The authors of the present case report describe a case of giant liposarcoma of the thigh that grew for 10 years, and subsequently extended into the retroperitoneum. Also, this case report aims to describe our surgical treatment protocol and its outcome. To our knowledge, this is the first such case reported in the literature.
Case report
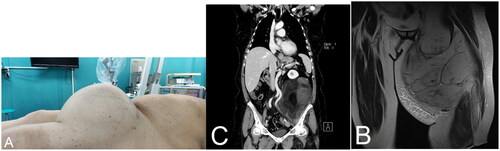
A 65-year-old female patient was admitted to the hospital for treatment of a tumor on her left thigh. Initially, the patient came to another institution because of a lump on her left thigh that did not cause any symptoms. Ultrasound imaging and core needle biopsy were performed, which described a benign lipomatous formation in the proximal part of the left thigh. Since then, the tumor has been growing for ten years, but in the last year the tumor started to grow rapidly. On examination, the patient reported pain in the inguinal region caused by stretching of the inguinal ligament due to the size of the tumor. Also, the patient complained of pain under the left costal arch, which was associated with irritation of the peritoneum by necrosis of the proximal part of the tumor. Due to the mass of the tumor, which was approximately 15 kg at the time of examination, the patient was unable to walk. As the reason for showing up late for the examination, the patient said that she was afraid of the coronavirus disease 2019 (COVID-19). Clinically, a swelling of 30 × 30 cm in size was observed on the front medial side of the thigh. When palpating the abdomen, resistance was palpated in the lower left quadrant, which corresponded to the intra-abdominal part of the tumor. Radiological images showed a heterogeneous mass with fat content on the ventral side of the left thigh. The formation also expanded to the rectus femoris muscle and compressed the other thigh muscles dorsally. There were also noticeable changes in the rectus femoris muscle and the vastus lateralis muscle, which could indicate muscle infiltration by a tumor or fatty degeneration. The tumor spread cranially through the inguinal canal into the pelvis extraperitoneally. In the pelvis, iliac blood vessels were pushed medially and dorsally by the formation. Furthermore, the formation occupied a large part of the left hemiabdomen, in the abdominal cavity. It compressed the descending colon to the right and reached the kidney, which was pushed cranially by the tumor formation (). The finding of the core needle biopsy primary corresponded to an atypical lipomatous tumor, but liposarcoma could not be excluded.
Figure 1. The patient’s pre-operative photo and the patient’s clinical photo. A left thigh tumor 30 × 30 cm in size can be seen (a). Magnetic resonance imaging of the thigh is showing heterogeneous mass with fat content on the ventral side of the left thigh that is compressing the upper leg muscles (B). Computed tomography image of the abdomen and pelvis is showing the formation occupying a large part of the left hemiabdomen. Also, the tumor is compressing the descending colon to the right and is reaching the kidney which is pushed cranially (C).
The surgical team, in addition to a plastic surgeon, also consisted of an abdominal surgeon. An elliptical incision was made above the tumor formation. The capsule of the tumor was separated from subcutaneous tissue. In the course of preparation of the tumor bed, fat infiltration was confirmed in the central part of the rectus femoris muscle, the distal insertion of which was subsequently cut. The neurovascular bundle was prepared and separated from the entrance into the adductor canal towards the proximal part. The tumor mass was separated until it entered the inguinal canal. A medial laparotomy was made and extended towards the inguinal canal. Subsequently, the peritoneal cavity was opened. A tumor formation in the left paracolic space, which pushed all the organs into the right hemiabdomen, was confirmed. The retroperitoneal space was entered through an incision along Told’s line. The ureter was separated from the tumor during visualization of the tumor site. The tumor was separated all the way to the inguinal canal. The inguinal ligament was subsequently cut and the laparotomy incision was connected to the incision in the femoral region. An en bloc resection of the tumor was performed and the specimen was sent for histopathological analysis. The retroperitoneum was closed and the parietal peritoneum was sutured. The fascia, aponeurosis of the oblique muscle and the abdominis externus were sutured and the inguinal ligament was reconstructed. Neurovascular bundle was covered by the flaps. Gracilis and vastus lateralis muscle flaps were used as regional myofascial flaps – meaning they were pulled under the inguinal ligament and used to cover the neurovascular bundle in the left femoral region. Preoperatively, a plan was made so that the wound could be primarily closed (). Due to the size of the tumor, part of the skin was excised en block with the tumor, and the local skin flaps were used for the reconstruction of the defect. The rectus femoris muscle was not spared because its proximal part was most likely the origin of the tumor. The patient started walking after three weeks with the help of one crutch.
The size of the excised sample was 48 × 33 × 22 cm and it weighed 15 kg (). The area of necrosis with a diameter of 8 cm was found in the sample. Also, a bone with a diameter of 2 cm was found in the center of the sample. Histologically, there were well-differentiated areas made of lipoblasts within the tumor tissue. They alternated partly with myxoid areas and partly with the area made of spindle cells. Immunohistochemically, tumor cells were MDM2 (focally) positive. The histopathological finding corresponded to high-grade dedifferentiated liposarcoma according to the FNCLCC adult sarcoma grading system.
Discussion
Only the rectus femoris muscle was invaded by the tumor, and since no structure of the retroperitoneum was invaded by the tumor, we believe that the origin of the tumor was in the left upper leg, from where the tumor spread through the inguinal canal into the retroperitoneal space.
The histopathological finding corresponded to high-grade dedifferentiated liposarcoma. Dedifferentiated liposarcomas are liposarcomas that progressed from primary or recurrent atypical lipomatous tumors/well-differentiated liposarcomas and are characterized by much higher rates of recurrence, metastases and mortality rates [Citation8,Citation9]. Although they are historically considered to be only high grade, variable grading has been recently recognized in dedifferentiated liposarcomas [Citation10]. Dedifferentiated liposarcoma typically occurs in middle-aged and elderly adults. The histological feature of dedifferentiated liposarcoma is the transition from atypical lipomatous tumor/well-differentiated liposarcoma to non-lipogenic sarcoma, and immunohistochemical stains are usually positive for MDM2 and/or CDK4 [Citation3,Citation8]. Dedifferentiated liposarcoma has a better prognosis than other high grade pleomorphic sarcomas. Nevertheless, it still has a recurrence rate of 40–75%, metastatic rate of 10–15% and is associated with mortality rate of 28% [Citation10–12].
In this report, we are presenting the case of a female patient with a massive dedifferentiated liposarcoma of the thigh that was growing for 10 years and, subsequently, spread to the retroperitoneum. By reviewing the literature, we found a similar case report describing a massive, initially retroperitoneal, dedifferentiated liposarcoma which spread to other anatomical regions [Citation13], but we did not find any case reports describing dedifferentiated liposarcoma of the upper leg that was growing for 10 years and spread through the inguinal canal into the retroperitoneum. Due to the specificity of the case, a new, specific surgical technique was used. In the presentation of the case, we describe this specific surgical technique. Also, the technique can serve as a recommended option for the surgical treatment of similar cases in the future. During the surgery, there were parts of the operation that were demanding. When separating the neurovascular bundle from the tumor, caution was required due to the attachment of the neurovascular bundle to the tumor capsule (there was no tumor cell invasion into the bundle). Also, attention was needed when separating the tumor from the urethra due to the proximity of the structure and the possibility of damage to the urethra. As the apex of the tumor formation was necrotic, no synthetic mesh was placed due to the greater risk of infection. Due to the complexity of the surgery, in this case, as well as in future similar cases, it is necessary to plan the procedure well, consult an oncologist, organize a multidisciplinary team, make good tumor demarcation with CT and MR, and possibly reduce the tumor mass with neoadjuvant chemotherapy. In this case, the patient was conditioned for one month before surgery to improve nutritional status.
Ethical consideration
The authors have granted informed consent from the patients to use the images.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Zafar R, Liposarcoma WY. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. [cited 2023 May 16]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK538265/
- Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO classification of soft tissue tumours: news and perspectives. Pathologica. 2021;113(2):1–4. doi:10.32074/1591-951X-213.
- Organisation mondiale de la santé, Centre international de recherche sur le cancer, editors. Soft tissue and bone tumours. 5th ed. Geneva: OMS; 2020. (World health organization classification of tumours).
- Lee ATJ, Thway K, Huang PH, et al. Clinical and molecular spectrum of liposarcoma. J Clin Oncol. 2018;36(2):151–159. doi:10.1200/JCO.2017.74.9598.
- Bock S, Hoffmann DG, Jiang Y, et al. Increasing incidence of liposarcoma: a population-based study of national surveillance databases, 2001–2016. Int J Environ Res Public Health. 2020;17(8):2710. doi:10.3390/ijerph17082710.
- Zagars GK, Goswitz MS, Pollack A. Liposarcoma: outcome and prognostic factors following conservation surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1996;36(2):311–319. doi:10.1016/s0360-3016(96)00265-9.
- Gronchi A, Miah AB, Dei Tos AP, et al. Soft tissue and visceral sarcomas: ESMO–EURACAN–GENTURIS clinical practice guidelines for diagnosis, treatment and follow-up⋆. Ann Oncol. 2021;32(11):1348–1365. doi:10.1016/j.annonc.2021.07.006.
- Nishio J, Nakayama S, Nabeshima K, et al. Biology and management of dedifferentiated liposarcoma: state of the art and perspectives. J Clin Med. 2021;10(15):3230. doi:10.3390/jcm10153230.
- Thway K. Well-differentiated liposarcoma and dedifferentiated liposarcoma: an updated review. Semin Diagn Pathol. 2019;36(2):112–121. doi:10.1053/j.semdp.2019.02.006.
- Dedifferentiated liposarcoma [Internet]. [cited 2023 May 17]. Available from: https://www.pathologyoutlines.com/topic/softtissuededifflipo.html.
- McCormick D, Mentzel T, Beham A, et al. Dedifferentiated liposarcoma clinicopathologic analysis of 32 cases suggesting a better prognostic subgroup among pleomorphic sarcomas. Am J Surg Pathol. 1994;18(12):1213–1223. doi:10.1097/00000478-199412000-00004.
- Henricks WH, Chu YC, Goldblum JR, et al. Dedifferentiated liposarcoma: a clinicopathological analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol. 1997;21(3):271–281. doi:10.1097/00000478-199703000-00002.
- Salemis NS, Nisotakis K, Patouras P, et al. Retroperitoneal liposarcoma extending into the thigh. Am J Surg. 2011;201(5):e38–40–e40. doi:10.1016/j.amjsurg.2010.04.019.


