Abstract
Background
This paper reports a rare anatomical variant of the facial artery (FA) - namely, a double FA pattern - which has significant implications in a wide range of surgical and aesthetic medicine disciplines.
Case
The study involves a case report and literature review of the FA and its variants. The case is that of a 61-year-old female cadaver with a unilateral FA variant branching pattern discovered during a cadaveric dissection for an anatomy course.
Discussion
The dissection revealed an unusual supply of the typical FA distribution by two separate branches from either side of the maxillary artery. The first branch, termed FA1, followed a typical FA course arising from the external carotid to supply the lower portion of the face via lingual, inferior labial, and mental arterial branches. The second branch, termed FA2, arose superior to the maxillary artery near the origin of a typical transverse facial artery, to supply the upper portion of the face via superior labial, lateral nasal, and angular arterial branches. No direct communication between the two branches was observed grossly via dissection. The observed branching pattern has not previously been reported in literature and has critical implications for surgical planning and intervention.
Conclusion
This study emphasizes the importance of understanding variant FA anatomy in procedures requiring precise anatomical knowledge of arterial supply to the face. Duplicate and/or secondary facial arteries necessitate careful consideration for their potential consequences on the success of surgery of the head and neck, dermal fillers, and embolization for epistaxis procedures.
Introduction
The face is a highly vascular area with numerous arterial variations [Citation1]. The facial artery, formerly also known as the external maxillary artery to differentiate it from what was known as the internal maxillary artery, is a major blood vessel responsible for supplying oxygenated blood to the face and portions of the neck. The course of FA is known for its tortuosity, to allow for stretching with the dynamic actions of the face such as facial expression and mastication [Citation1–3].
FA provides the major blood supply to diverse structures in the superficial face, including the skin and mucosal tissues of the face; muscles of facial expression, speech, and chewing; and salivary and labial glands. It typically originates from ECA within the carotid triangle, ascends through the submandibular gland, and winds across the inferior border of the mandible before ascending anterior to the masseter to supply the anterior (frontal) portions of the face. The main facial branches of the facial artery are the inferior labial branch (lower lip, labial glands), superior labial branch (upper lip, nasal septum, ala of the nose), lateral nasal branch (dorsum of the nose), and the angular artery (lacrimal sac, orbicularis oculi muscle).
The FA terminates as AA, supplying the medial canthus of the eye (). AA also anastomoses with the dorsal branch of the ophthalmic artery.
The transverse facial artery (TFA) is another contributor to the blood supply of the superficial space, including the skin, muscle and other structures in the cheek area. Most importantly, it primarily supplies blood to the parotid gland and the facial nerve. It typically originates from the superficial temporal artery (STA) before coursing through the face superficial to the masseter, just inferior to the zygomatic arch. It then anastomoses with branches of the FA [Citation3].
Known anatomical variations of the facial and transverse facial arteries
Several variants of the FA have been reported. Common variants in the literature include differences in the origin, course, and terminal branching. For instance, FA may alternatively originate from a linguofacial or thyro-linguo-facial trunk. In a study of 30 cadavers, only 2 were found to have a higher (more distal) origin of FA, both originating just below the maxillary artery origin within the parotid gland. Other cases in the literature include an enlarged FA [Citation3], an FA with a branch to the lingual artery [Citation4], an FA originating from the internal carotid or common carotid in the absence of the external carotid [Citation5,Citation6], and an FA with a branching submental artery with varying distances from the FA origin [Citation7].
In the current case, variants in the terminal branches of FA are most relevant. A meta-analysis of terminal FA variants described in literature determined five classifications based on terminal arteries: (1) superior or inferior labial (15.55%), (2) inferior alar (5.89%), (3) lateral nasal or angular (69.81%), (4) dominant lateral branch (1.72%), and (5) hypoplastic facial (0.81%) [Citation8]. In a study of 201 facial arteries in 112 cadavers in the UK, six variants were detected, including the classifications listed in the meta-analysis as well as no FA detected (2%). In the 7 specimens with an absent FA, a dominant TFA supplied the territory of FA [Citation9]. In another UK study of 50 facial arteries in 25 cadavers, 5 of these variants were detected based on their terminal arteries, including cases of an absent FA in which the transverse facial, infraorbital, or ophthalmic arteries served as alternative blood supply [Citation10].
Like FA, variants in the origin and course of TFA have also been studied for its relevance in surgery of the head and neck. In a retrospective study of 100 patients with previous head computed tomography angiography with bilateral TFA visualization, TFAs originated from the superficial temporal artery (91.7%), a common trunk with the superficial temporal artery and maxillary artery (4.7%), the external carotid artery (3.1%), or the maxillary artery (0.5%). One case of TFA demonstrated dominance over a hypoplastic facial artery [Citation11], which has also been described in previous reports [Citation3].
Case report
The face of a 61-year-old female cadaver was dissected by a faculty member (AME) to prepare cadaveric prosections for a first-year anatomy course. The dissection was performed in accordance with Grant’s Dissector, 17th Edition [Citation2]. As such, skin flaps were developed bilaterally. The left side of the face was dissected first. No anomalies were discovered; i.e. the left facial artery (FA) was a branch of the external carotid artery (ECA), and the typical FA branches were identified. These included the inferior labial artery (ILA), superior labial artery (SLA), lateral nasal artery (LNA) and ended with the angular artery (AA). A small transverse facial artery (TFA) was identified in its usual position; i.e. as a branch of the superficial temporal artery (STA) shortly after its takeoff from ECA and which proceeded anteriorly for a short distance before dividing into multiple tributaries.
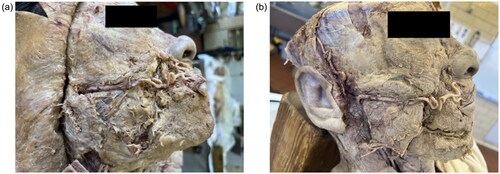
On the right side, however, a large transverse (horizontally-oriented) artery - at about the level of the inferior edge of the tragus - was encountered immediately upon elevating the skin flap (). Situated within the subcutaneous tissue and surrounded by branches of the facial nerve, it was resting in a furrow in the parotid gland and continued superficial to the masseter.
Figure 1. (a) Initial view of a right anomalous facial artery before skin removal, coursing horizontally across the face. Branches of the facial nerve are visible immediately surrounding the artery. (b) Further dissection demonstrated two facial arteries from the external carotid artery (ECA).
On further dissection, it was noted that this cadaver had essentially two right facial arteries: a superior artery (encountered first and referenced as FA2) and an inferior artery (FA1), arising from the ECA in the neck and supplying the inferior portion of the distribution that is normally covered by a single FA. FA1 actually arose from ECA via a Common Trunk, which then divided into FA1 and the Lingual Artery (LA). ().
FA2 originated from the STA 9 mm distal to the bifurcation of ECA into the maxillary artery (MA) and STA (). FA1 originated from ECA 37 mm proximal to the MA/STA bifurcation (see for measurements; note that FA2 is 1 mm wider in diameter than FA1). Therefore, ECA essentially trifurcated into an MA, STA, and an aberrant FA (aka FA2).
Figure 2. (a) The proximal end of ECA gives rise to a common trunk (CT), which divides into FA1 and lingual artery (LA). FA1 later gives off mental artery (MeA). The distal end of ECA gives rise to a trifurcation of MA, FA2, and STA. The superior thyroid artery (SThA) is also identified. (b) with arteries outlined in red.
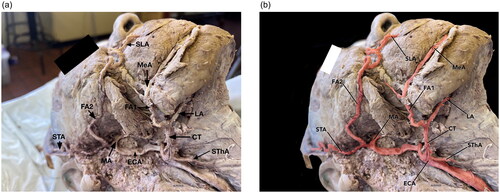
Furthermore, the typical distribution of the end-arteries of FA was divided into two regions (). The lower (inferior) portions, consisting of ILA and a large mental artery (MeA), derived from FA1. The upper (superior) portion of that distribution, however - including SLA and AA - originated from FA2.
Figure 3. (a) FA2 Runs transversely across the cheek to give branches to the superior labial artery (SLA) and lateral nasal artery (LNA). FA1 gives rise to MeA, which gives rise to the inferior labial artery (ILA). (b) with arteries outlined in red.
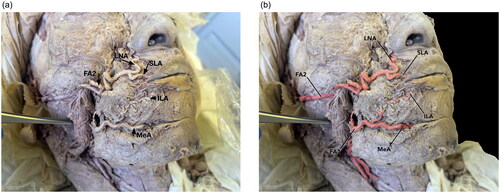
Figure 4. Measurements: FA1, MA, FA2, and STA branch from ECA. The diameter of ECA is 8 mm proximally, 7 mm after FA1 takeoff, and 5 mm after MA takeoff. As ECA terminates as STA, the diameter is 3 mm. The diameters of FA1, MA, and FA2 are 3, 5, and 6 mm, respectively. The distance between the takeoffs of FA1 and MA is 37 mm, and the distance between the takeoffs of MA and FA2 is 9 mm.
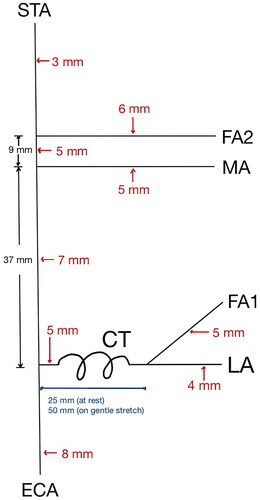
Figure 5. Normal facial artery branches from ECA and courses around the inferior border of the mandible before branching into the superior and inferior labial arteries, and LNA. FA, via LNA, ultimately terminates as AA at the medial canthus of the eye. Image source: [Citation1].
![Figure 5. Normal facial artery branches from ECA and courses around the inferior border of the mandible before branching into the superior and inferior labial arteries, and LNA. FA, via LNA, ultimately terminates as AA at the medial canthus of the eye. Image source: [Citation1].](/cms/asset/a3423220-5e01-46fb-8650-380116cb09d4/icrp_a_2376136_f0005_c.jpg)
Of note is that this cadaver had two other anomalies, also on the right side. The right recurrent laryngeal nerve passed around the brachiocephalic artery as it turned superiorly, rather than around the right subclavian artery. In addition, the right pectoralis minor muscle had two innervations. Both the medial pectoral nerve and the intercostobrachial nerve were seen to enter and exit the muscle into the pectoralis major. It is not known or postulated that these are necessarily related.
Discussion
It is debatable whether the artery in this case report is primarily a variant duplication of FA or whether it represents what is essentially an “overgrown” TFA. We prefer the former, because so much of the distribution of this artery (FA2) constitutes branches that would normally be derived from a single FA. TFA typically courses for only a relatively short distance and then ends with anastomoses to some branches of FA. This artery, on the other hand, is so extensive and sweeping in the area it solely oxygenates - without significant connections to FA1 - that we feel it is a FA with equal standing to the one originating from ECA in the neck. Furthermore, FA2 is actually slightly bigger (wider in diameter) than FA1. We recognize, however, the potential for one or more differing interpretations.
FA1 appears most similar to the inferior portion of the normal FA, with the same origin near the angle of the mandible coming off from a common trunk as the lingual artery (LA) and coursing superiorly. FA1 also gives rise to the mental artery (MeA) in this cadaver, which gives rise to ILA. On the other hand, FA2 originates from STA immediately after its takeoff from MA (essentially a trifurcation), gives rise to SLA, and terminates as AA. The origin of FA2 appears most similar to TFA, crossing the face superficial to the masseter and inferior to the zygomatic arch, and coming off more distal from MA in their common trunk.
In a large-scale study described in a previous section, variant terminal arteries of FA include angular, lateral nasal, inferior alar, superior labial, inferior labial, and no FA detected. The first four described variants demonstrate one dominant FA supplying SLA and ILA. The terminal ILA variant (2%) is similar to FA1, while the undetected FA (2%) included 7 cases of TFA dominance, which is similar to FA2. However, none of these cases appear to describe the dual facial arteries (FA1 and FA2) as seen in the current case [Citation9]. Similarly, the other two studies of cadaveric facial arteries mentioned previously did not describe any cases similar to the current case [Citation10,Citation12].
Two case reports of variant FA were also examined. In a case report from India by Marx et al. a cadaver was found to have a right FA terminating as ILA and a left FA without an ILA branch, but normal superior labial, lateral nasal, and angular arteries [Citation13]. In another case report from Nepal by Kumar et al. an FA arose from a common linguofacial trunk and terminated as ILA, while a TFA gave rise to superior labial, lateral nasal, and angular arteries [Citation14]. Both of these cases describe similarities to FA1 and FA2 in this case. However, key differences include FA1 and FA2 appearing on the same side of the face, with MeA arising from FA1 and ILA arising from MeA, and FA1 continuing superiorly to supply other areas of the face.
In examining variant TFA literature, one large-scale study of 100 patients with bilateral CTAs showed one case (0.5%) of a dominant TFA and hypoplastic FA [Citation11]. This case also appears similar to the current case, but does not describe in detail the arterial branches from TFA and FA.
Clinical implications
Plastic surgery
Knowledge of variant FA and TFA are important in planning for plastic surgery and head and neck procedures, whether reconstructive or aesthetic. There are many examples of this; we have chosen to highlight a few.
For instance, FA is commonly used as a pedicle in flaps, such as nasolabial skin, oral mucosal, buccal mucosal, and facial artery musculomucosal (FAMM) flaps, for correction of oromucosal defects due to causes such as tumor ablation, trauma, cleft palate, and oroantral fistula [Citation3].
FAMM is used to repair surgical defects in the oral cavity, oropharynx, intranasal lining, and orbit and to treat mandibular osteoradionecrosis. Variant facial anatomy can influence FAMM flap elevation, size, and pivot point. In the current case, there are two potential sources of blood supply with separate branches. Flap design and execution must incorporate the correct arterial inflow to maintain viability of the flap. Furthermore, the pivot point varies based on blood supply; specifically, an inferior base flap is considered when facial vessels enter the face through the anterior border of the masseter, while a superiorly-based flap is based on the angular artery or the superior labial branches of FA. These considerations underscore the importance of FA anatomy in the planning and design of the FAMM flap [Citation15]. Similarly, surgeons should be aware of the variant FA anatomy for other flaps such as the vermillion/labial flap and other reconstructive procedures.
For facelifts and similar procedures, care must be taken particularly if SMAS or deep plane procedures are being planned. For example, if an aberrant artery such as this is identified intraoperatively, the proposed surgical procedure may need to be modified.
To prevent complications related to FA and TFA variation, pre-surgical planning when appropriate may include accurate preoperative imaging such as color Doppler to assess the anatomy of TFA and FA, or ECA angiography if Doppler yields uncertain results [Citation16].
ENT/head and neck surgery
Procedures such as parotid and maxillary sinus surgery, particularly those using the Weber Ferguson approach, may be impacted by anomalous arterial patterns. Awareness or variants may warrant additional preoperative imaging.
Aesthetic medicine
Aesthetic medicine can involve the injection of volume replacement (fillers). Injectable fillers are viscous when compared with neuromodulator injection (which is a liquid). TFA and FA anatomy are relevant since inadvertent intra-arterial injection can cause complications ranging from tissue necrosis to blindness [Citation11,Citation16].
In this case of variant anatomy, an anomalous facial artery such as FA2 occurs where only a small and relatively insignificant TFA is expected. Since AA anastomoses with a branch of the ophthalmic artery, cosmetic filler and neuromodulator injections in this region may be associated with additional complications. This includes in the case of fillers, tissue necrosis and/or embolization to distant arteries including the ophthalmic which may result in blindness.
Injections of neuromodulators into the masseter muscle have also recently gained traction for bruxism, TMJ pain, and masseter hypertrophy [Citation17]. The location of the FA2 across the upper masseter poses a danger (i.e. excess bleeding) if injecting neuromodulators into the area.
Targeted chemotherapy
TFA is also important in targeted intra-arterial chemotherapy as it is commonly a significant feeding artery of maxillary sinus cancer. Surgeons and interventional radiologists should be aware of TFA and its variants as well as variants of the facial arteries, as they may impact the success and potential complications of these procedures [Citation11].
Interventional radiology
Knowledge of FA anatomy is important for the treatment of refractory idiopathic epistaxis via maxillary artery and FA embolization [Citation18]. FA embolization stops flow through the SLA, which contributes to the arterial blood supply of the nasal septum. Anomalous FA anatomy, such as the current case, is relevant since FA1, which is located where FA is normally (across the inferior border of the mandible), eventually supplies ILA but not SLA. FA2 would need to be embolized instead in this case. The presence of a branch to the mental artery in the FA1 variant also necessitates consideration of potential complications such as reduced mental artery flow, which may cause alveolar bone atrophy [Citation19].
Other applications of FA embolization and arteriography include head and neck arteriovenous malformations [Citation20]; head and neck cancers; vascular tumors; hemorrhage after head and neck procedures such as tonsillectomy and dental extraction [Citation21]; and traumatic pseudoaneurysm of the facial artery [Citation22,Citation23]. Awareness of FA variation is critical to optimize outcomes and prevent complications in these procedures.
Conclusion
In conclusion, we present a rare variant of facial vasculature with significant implications across many disciplines. This cadaver has 2 facial arteries on her right side which both provided the major branches of a normal facial artery. However, because of the origin of the aberrant artery – where only a small and relatively insignificant transverse facial artery would normally be – there is the potential for inadvertent injury during surgery and injectable procedures.
Furthermore, this report showcases a unique variation even amongst known variations of the facial artery. Specifically, there is branching not previously seen in the literature, including one facial artery giving the mental and inferior labial arteries, and another supplying the superior labial, lateral nasal, and angular arteries. No significant connections between these two apparently independent systems were observed.
A wealth of literature exists in facial arterial anatomy because of its importance in surgery of the head and neck, and aesthetic medicine. Suggestions for future research include studies exploring the prevalence of various FA and TFA variations either by color Doppler ultrasonography and CTA imaging of live patients or via cadaver studies. Studies should also be conducted to determine the most effective preoperative imaging methods to identify these variants.
Acknowledgements
The authors acknowledge and thank the individual whose body and tissues were used in this study to better understand head and neck anatomy for the advancement of medical education and patient care. The authors would also like to thank Chris and Rob in the anatomy lab for their assistance and services.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Meegalla N, Sood G, Nessel TA, et al. Anatomy, Head and Neck: Facial Artery. [Updated 2024 May 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536932/
- Detton AJ. Grant’s dissector. Wolters Kluwer; 2017.
- Moore KL, Dalley AF, Agur A. Clinically oriented anatomy. 8th ed. Lippincott Williams and Wilkins; 2017.
- Ostrowski P, Szczepanek E, Niemczyk K, et al. A 3D map of the lingual artery-The perfect tool for transoral robotic surgeries on the base of tongue. Head Neck. 2023;45(4):1–7. doi:10.1002/hed.27303.
- K K. Eine seltene anomalie von Verzweigungen der A. carotis communis. Acta Anat Nipón. 1950;25:22–24.
- Basekim CC, Silit E, Mutlu H, et al. Type I proatlantal artery with bilateral absence of the external carotid arteries. AJNR Am J Neuroradiol. 2004;25(9):1619–1621.
- Ostrowski P, Bonczar M, Gliwa J, et al. Topographic anatomy of the submental artery and its clinical implications for reconstructive surgery. Clin Anat. 2023 Jul 21. Epub ahead of print; doi:10.1002/ca.24096.
- Koziej M, Bonczar M, Ostrowski P, et al. Termination points of the facial artery-A meta-analysis. Clin Anat. 2022;35(4):469–476. doi:10.1002/ca.23817.
- Lohn JWG, Penn JW, Norton J, et al. The course and variation of the facial artery and vein: implications for facial transplantation and facial surgery. Ann Plast Surg. 2011;67(2):184–188. doi:10.1097/SAP.0b013e31822484ae.
- Niranjan NS. An anatomical study of the facial artery. Ann Plast Surg. 1988;21(1):14–22. doi:10.1097/00000637-198807000-00003.
- Koziej M, Polak J, Wnuk J, et al. The transverse facial artery anatomy: implications for plastic surgery procedures. PLoS One. 2019;14(2):e0211974. doi:10.1371/journal.pone.0211974.
- Hong SJ, Park SE, Jo JW, et al. Variant facial artery anatomy revisited: conventional angiography performed in 284 cases. Medicine (Baltimore). 2020;99(28):e21048. doi:10.1097/MD.0000000000021048.
- Marx C, Kumar P, Reddy S, et al. Bilateral variation of facial artery: a case report. Rom J Morphol Embryol. 2008;49(3):399–401.
- Ajit K, et al. A Rare Variation in Facial Artery and Its Implications in Facial Surgery: case Report. Journal of Surgery. 2014;2(5):68–71.
- Angulo C, et al. Facial artery, an essential anatomy in different specialties: a review. Journal of Otolaryngology-ENT Research. 2022;14(1):14–20.
- Toure G, Nguyen T-M, Vlavonou S, et al. Transverse facial artery: its role in blindness after cosmetic filler and botulinum toxin injections. J Plast Reconstr Aesthet Surg. 2021;74(8):1862–1869. doi:10.1016/j.bjps.2020.12.042.
- Fernández-Núñez T, Amghar-Maach S, Gay-Escoda C. Efficacy of botulinum toxin in the treatment of bruxism: systematic review. Med Oral Patol Oral Cir Bucal. 2019;24(4):e416–e424. doi:10.4317/medoral.22923.
- Krajina A, Chrobok V. Radiological diagnosis and management of epistaxis. Cardiovasc Intervent Radiol. 2014;37(1):26–36. doi:10.1007/s00270-013-0776-y.
- Kikuta S, Iwanaga J, Kusukawa J, et al. The mental artery: anatomical study and literature review. J Anat. 2020;236(3):564–569. doi:10.1111/joa.13113.
- Meila D, Grieb D, Greling B, et al. Endovascular treatment of head and neck arteriovenous malformations: long-term angiographic and quality of life results. J Neurointerv Surg. 2017;9(9):860–866. doi:10.1136/neurintsurg-2016-012570.
- Storck K, Kreiser K, Hauber J, et al. Management and prevention of acute bleedings in the head and neck area with interventional radiology. Head Face Med. 2016;12(1):6. doi:10.1186/s13005-016-0103-3.
- Marco de Lucas E, Gutiérrez A, González Mandly A, et al. Life-threatening pseudoaneurysm of the facial artery after dental extraction: successful treatment with emergent endovascular embolization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(1):129–132. doi:10.1016/j.tripleo.2007.09.031.
- Ribeiro-Ribeiro AL, de Melo Alves Junior S, de Jesus Viana Pinheiro J. Traumatic pseudoaneurysm of the facial artery: late complication and effects on local blood flow. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(1):E4–9. doi:10.1016/j.tripleo.2011.03.018.
