?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Health resources are an important factor to reduce infant and child mortality. However, taking into account budget constraints, it is very difficult to increase public health resources for all regions within a country at the same time. For this reason, in this paper, we assess the effects of the regional health government expenditure assignment as well as the regional health resources available such as beds or paediatricians. We estimate a dynamic model using a system-GMM (Generalised Method of Moments) to explain infant and child-mortality in Kazakhstan during the period 2000–2018. In this period, Kazakhstan experiences a sharp decrease in infant and child mortality reaching the target values from sustainable development goals (SDG). We evaluate several variables to capture the effects of public health resources assignment, such as expenditure per capita, expenditure depending on previous year mortality rates as well as health facilities resources for children by region. Results show that an increase in health expenditure per capita in those regions with high mortality levels is particularly relevant to reduce infant mortality while health facilities are actually more important to reduce an under-5 mortality rate.
1. Introduction
Many papers focused on analysing the factors which decrease infant and under-5 child mortality, few of them analyse regional differences within a national territory, i.e. comparing areas with similar institutional structure. In a regional setting, we can assess the way on how the countries assign the budget to the regions. This is particularly important in countries so large as Kazakhstan and with a low population density (around 7 hab/km2), which makes more difficult to provide health services to remote territories of the country. For this reason, the aim of this paper is to find the determinants behind the regional differences on children’s health outcomes measured using infant mortality and child mortality in Kazakhstan.
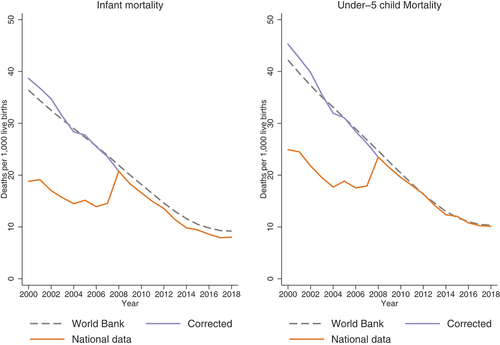
As the OECD report on the Kazakhstan health system OECD (Citation2018) highlights, “Kazakhstan has made significant economic progress over recent decades … and Health has risen on the policy agenda with a number of sector reforms introduced.” Like other CIS countries, since 1995 Kazakhstan have had a growing trend of total health expenditure per capita in USD PPP.Jakovljevic et al. At the same time, in last two decades Kazakhstan shows a striking reduction of infant and under-5 child mortality rates ().
Figure 1. Evolution of infant and under-5 child mortality in Kazakhstan (average and regional variation).
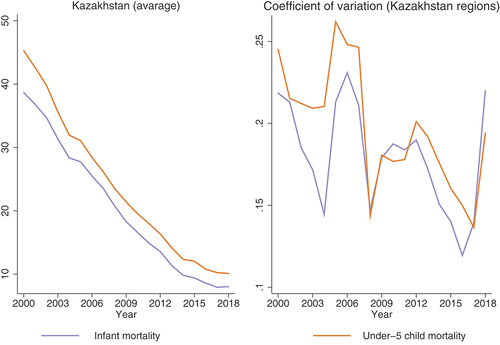
In fact, under-5 child and infant mortality rate in Kazakhstan decreased by more than 50% from 2009 to 2018, reaching the Sustainable Development Goal in 2016 set at 12 deaths per 1,000 live births for infant mortality and 25 for under-5 child mortality rate. However, as we can observe through the coefficient of variation in , the striking improvement in infant mortality at the national level is masking marked differences across regions. In fact, OECD (Citation2018) points out that despite general economic progress, regional disparities have not been reduced. In particular, in 2018, the region with the lowest infant death rate, Nur-Sultan city, recorded approximately 5 deaths per 1000 live births while in Kostanay almost double this number and the mortality rate exceeded 10. These differences are even higher in rural areas.
Evidence suggests investing in child’s health will return in future social and economic benefits through improved productivity Stenberg et al. (Citation2014). For this reason, a good distribution of the health expenditure across regions is a key, since it can help to decrease future regional income inequality. In fact, authors such as Behera and Dash (Citation2020) point out that achieving healthcare goals plays an important role in the relationships between better human development and rising economic growth. Additionally, countries cannot grow in a sustainable way without reducing regional inequalities, and health considerably correlated with future education, productivity and consequently with the future economic growth (Grossman, Citation1972).
Thus, this paper contributes to the literature by analysing regional determinants of infant and under-5 child mortality in a big country such as Kazakhstan with particular characteristics such high levels of education and immunisation.Footnote1 Additionally, it contributes by analysing how regional distribution of the health budget affects infant and under-5 child mortality.
The paper starts with Introduction and then is structured as follows: section one provides a brief discussion of the literature review that supports our paper, section two explains the methodology and the databases used, section three shows the results that are discussed in section four and finally we draw some conclusions.
2. Literature review
In the way to achieve the Sustainable Millennium Goals healthcare development is becoming a key public policy priority worldwide. Investments in healthcare grow globally outside of the European Union in emerging Eurasian countries, such as Kazakhstan, while Western Pacific countries, including China, are leading in healthcare spending growth rates. M. Jakovljevic et al. (Citation2019b) For almost two decades after 1995 per capita health spending have been higher in middle-income countries (more than 5 percent annually, purchasing power-adjusted) compared to high-income countries (3 percent annually; Dieleman et al., Citation2017).
To improve health outcomes policymakers should identify the factors that can prevent illness from happening (preventable factors) and those factors that can treat illness once it happens (treatable factors). Identifying the variables behind those factors where policymakers can act is key to reducing regional disparities on health outcomes. Factors related to prevention (factors causing sickness) are more related with individual and/or family behaviour such as diet, regular physical activity, parent’s smoking or alcohol consumption, etc. Thus, these kinds of factors increase the probability that a child develops an illness. In this case, education can be one of the better tools from a policy point of view. However, treatable factors are more related to the health sector (e.g., service delivery, health workforce, medical products, technologies), health sector financing (e.g., expenditure per capita, health coverage, etc.), health systems governance (e.g., adoption of enabling policies for women’s and children’s health). Thus, these factors are very linked with the public health system, and in this case how it is structured at regional level.Footnote2
The availability and quality of most of the factors mentioned that can prevent and treat infant and child illness, i.e. reducing mortality are funded by public, private and external health expenditure. However, to promote and maintain the health system in remote areas when private health is not profitable, public expenditure is the one giving coverage, i.e. improving health care facilities, providing immunizations, childbirth care etc. and as a result reducing infant and child mortality (Kiross et al., Citation2020). However, this requires governments to do an optimal allocation of funding to most needed areas (Sommer, Citation2020). For this reason, health expenditure is one of the variables that can determine the proper work of health system and its proper assignment by regions can decrease infant and child mortality inequality rates at regional level, boosting a faster reduction at national level.
M. B. Jakovljevic et al. (Citation2016) comparing health expenditure and longevity trends between the European Union (EU), the Commonwealth of Independent States (CIS), and South-Eastern Europe (SEE) countries for the period 1989–2012, found that despite a high increase in healthcare per capita expenditures (adjusted for PPP) in most of the states in these regions, longevity improved only in SEE and nearly all EU countries, but not in CIS economies (M. B. Jakovljevic et al., Citation2016).
There is an important amount of evidence stating that public expenditure reduces infant and child mortality in different regions of the world, including developing countries as a whole (Dhrifi, Citation2018; Ray & Linden, Citation2020), African countries (Asiedu et al., Citation2015), Southern African countries (Nyamuranga & Shin, Citation2019), Sub Sahara African countries (Novignon & Lawanson, Citation2017), as well as South and South-East Asian countries (Behera & Dash, Citation2020; Rahman et al., Citation2018). Nonetheless, the magnitude of the effect is different depending on country, according to their development level and wealth, its resource allocation and adequate institutional governance, which might influence the effectiveness and efficiency of expenditure allocation Dhrifi (Citation2018), (Nyamuranga & Shin, Citation2019).
However, authors such as Filmer and Pritchett (Citation1999) do not find strong evidence that public health expenditure plays a positive role in improving infant and under-five child mortality rates. The reasons why public health expenditure may not come out significant to reduce child mortality or child mortality can be related to:
The trade-off with out-pocket spending or external expenditure i.e. if public expenditures replace pocket spending or external expenditure and does not reduce infant of child mortality (Bokhari et al., Citation2007; Musgrove, Citation1996).Footnote3 However, out-of-pocket expenditure does not guarantee the access to the healthcare expenditure (Kiross et al., Citation2020) and access of the health sector can really determine the level of infant and child mortality.Footnote4 Actually, Kiross et al. (Citation2020) do not find significant effect of private health expenditure on infant or neonatal mortality. Additionally, private out-of-pocket health can have important consequences on the household finances and send them to extreme poverty (Kiross et al., Citation2020).
The high level of corruption and the translation of public health expenditure on health infrastructures and good quality services (Akinlo & Sulola, Citation2019; Farag et al., Citation2013). In fact the level of good governance can determine the magnitude of the impact of health expenditure on infant and under-5 infant mortality (Sommer, Citation2020). Government health resources can be used to improve or invest in large-scale health programs that include personal training, hospital updates, equipment, and primary care. Public medical care expenditures fund everything from immunizations to family planning (Sommer, Citation2020). For instance, this should translate in a higher number of beds per kids, pediatricians per kids, etc. In fact, Muldoon et al. (Citation2011) identify that higher number of doctors together with better access to water and less corrupted government are important determinants of health and infant mortality. However, corruption reduces the amount of public medical care expenditures available leading to health facilities without the equipment and staff necessary to provide efficient and effective care and undermined the effectiveness of public health expenditure on reducing infant and under-five child mortality.
Endogeneity and dynamics of the public expenditure variable Bokhari et al. (Citation2007), Behera and Dash (Citation2020), Bhalotra (Citation2007), Rahman et al. (Citation2018), and Nwude et al. (Citation2020), i.e. several authors found that public health expenditure has effects on infant mortality in developing countries after controlling for unobservable heterogeneity and time trends on the sample.
Related with prevention factors, income per capita can measure the effect of income on health working through different indirect channels such as better nutrition, better housing, better sanitation, etc. (Filmer & Pritchett, Citation1999; Poudel et al., Citation2022). In low- and middle-income economies undernutrition is one of the key causes of under-5 children mortality (Black et al., Citation2013). Several authors found that income per capita decreases infant and under-5 child mortality, particularly in developing countries (Asiedu et al., Citation2012, Citation2015; Baird et al., Citation2011; Harttgen et al., Citation2013; Headey, Citation2013; Nwude et al., Citation2020). For instance, poor households in developing countries share a higher risk in mortality compared with their richer counterparts. In this sense, the improvements of average income per inhabitant in a country should also increase the average level of health of the population, in particular of the kids. The reason is that the population would have more resources to use in health and the government would also have higher rents to provide public health. Literature has broadly proven for most countries that the infant population get more affected by poverty than other age groups, emphasizing their vulnerability, especially in health (Bönke & Schröder, Citation2011; Cantó & Luis, Citation2014).Footnote5 These income shocks affect particularly infant mortality in rural areas (Bhalotra, Citation2010) and girls Baird et al. (Citation2011).
Parents’ education, in particular mother’s, has a negative impact on mortality rate according to many studies (Auster et al., Citation1969; Filmer & Pritchett, Citation1999; Grossman, Citation1972; Hug et al., Citation2018; Kemna, Citation1987; Nyamuranga & Shin, Citation2019; Pamuk et al., Citation2011). However, Kazakhstan as other post-Soviet Union countries shows high level of female education with lower variability across regions, so this variable may not play a role. The same happens with the level of immunization or access to water.
3. Methods and data
3.1. Estimation methods
Some authors such as Asiedu et al. (Citation2015); Novignon and Lawanson (Citation2017) argue that infant and under 5 child mortality are likely to be persistent, i.e., current values of child mortality are likely to be correlated with their previous values.Footnote6 For this reason, lagged infant and under 5-child mortality variables should be included as an explanatory variable in its corresponding regression model and, consequently, a dynamic model should be used for estimating the determinants of infant and under-five child mortality. Within these class of models based on a finite set of regions, the fixed effects estimator is considered to be more appropriate than random effects since regional-specific characteristics tend to be correlated to other individual effects representing omitted variables. We can formalize the model as:
where is infant mortality rate (dependent variable) is a scalar accounting for the infant mortality persistence, the regressor vector
is
and is composed of the explanatory variables (beds per number of kids, pediatricians by kids, health expenditure per capita, share of kids in rural areas and GDP per capita) and is
. The fixed effect component
follows one component error such as:
where and
are independent of each other and among themselves.
The OLS and within transformation estimator are biased and inconsistent since a lagged dependent variable is included. Generalized method of moments (GMM) proposed by Arellano and Bond (Citation1991) is more efficient than the Anderson and Hsiao (Citation1982) estimator. Arellano and Bond (Citation1991) propose to use the existing orthogonality conditions between lagged values and disturbances as additional instruments. To improve the previous estimation technique, Blundell and Bond (Citation1998) consider the additional assumption that,
This system GMM estimator uses lagged differences as instruments for equations in levels, in addition to lagged levels of instruments for equations in first differences. The system GMM estimator shows a dramatic efficiency gain over first-difference GMM (Arellano & Bond, Citation1991) as 1, assuming a stationarity restriction on the initial conditions of
.
Although GMM estimators perform better in panels with large N and small T, Soto (Citation2007) proves through Monte Carlo simulations that the system GMM estimator has a lower bias and higher efficiency than all the other estimators analysed, including the standard one-step difference GMM estimators. Previously, Judson and Owen (Citation1999) have also shown that when T = 20 GMM OR Anderson and Hsiao (Citation1982) estimator may be chosen.Footnote7
Moreover, the GMM framework is flexible and it accommodates unbalanced panels as well as multiple endogenous variables. This is an important characteristic since variables such as public health, GDP per capita or characteristics of health system such as number of pediatricians or bed may be endogenous.Footnote8 For this reason, we will use the system-GMM (Blundell & Bond, Citation1998) to estimate our model, since it seems to perform better. We will use Sargan overidentification test to test the validity of the assumptions used to obtain the moment conditions of System GMM. However, the system GMM may generate too many instruments in panels with large T leading to the problem of overfitting and reducing the power of the Sargan and Hansen test (Roodman, Citation2009b,a). We use two main techniques to limit the number of instruments: (i) to use only 2 of 3 lags instead of all available lags, (ii) to collapse the vectors of instruments that have the same information.
3.2. Data and indicators for measuring regional health resources
Based mainly on the data from the Committee on Statistics of the Ministry of National Economy of the Republic of Kazakhstan, we have built a panel of indicators for Kazakhstan oblasts from 2000 to 2018.Footnote9 Details on the indicators definitions are included in table A1 in the Appendix.
The dependent variables infant and under-5 child mortality indicators for Kazakhstan regions have suffered a methodological change in 2018 and we have had to adjust the series. In 2008, Kazakhstan switched to the new criteria for live births recommended by the World Health OrganizationFootnote10 creating a break in the series. In , we can see the break in the national series comparing the corrected data from the World Bank.
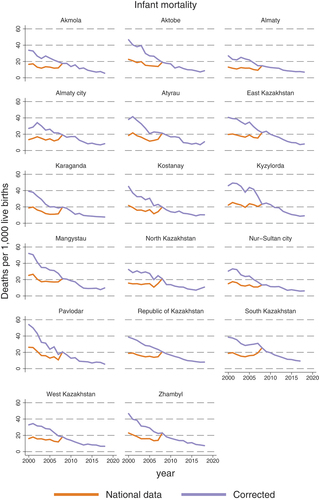
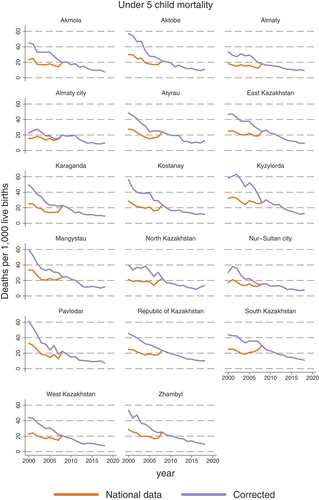
Unfortunately, the World Bank does not provide data for Kazakh regions and we have to adjust regional series. For the correction, we base on number of deaths for Kazakhstan on infant and under-5 children from the World Bank (corrected series) and we distribute this total for each region applying the regional shares calculated from the number of deaths based on the national data (unadjusted series). We assumed that methodological changes do not affect the relative position of each region on the total number of infants and under-5 children deaths. Once we have calculated the total number of death for each region and age-group, infant and under-5, respectively, we divide them by the number of alive kids in each year (based on national data) and we multiply for 1,000 to get the indicators. Results for each region can be seen in the Figures A1 and A2 in the Appendix).Footnote11
For independent variables, we have also done some data adjustments (details on all definition are in the appendix). In particularly, population data have different aggregation depending on the age group, and have been aggregated for getting the ranges that we needed. As authors such as Kiross et al. (Citation2020) point out: to estimate the determinants of infant and under-5 children mortality we need to control for different country demographic structures. In particularly, the share of young population (in this case we used younger than 14) is expected to increase infant and under-5 children mortality outcomes by increasing death rates. Urbanization rate is other important control variable related with the distribution of the population. Additionally, part of these regional differences in infant or under-5 child mortality may arise due to differences in the distribution of health resources. In fact, regional disparities in Kazakhstan are significant in the number of medical workers and rural and remote areas suffer from a shortage of qualified health personnel. Across rural Kazakhstan, the ratios of doctors to population are abysmally low. This fact suggests not only that rural doctors are probably overworked, but also that adequate access to good quality care in rural areas may be compromised. Actually, recent medical graduates tend to prefer working in urban areas, not only as they offer better financial and social opportunities, but also because the workload is higher in rural areas.
As we explained in the literature, two key variables are GDP per capita and the government health expenditure per capita, both in real terms (at prices of 2010). In order to capture the way that government health expenditures are distributed by region we calculate the share of health expenditure of each region in the national health expenditure budget relative to the share of population of each region from the national populations. If the government assigned the health budget according to the number of people in each region this ratio should be 1 or closer to 1 in all regions.
Being Hexp as health expenditure at national (N) and regional level (R) respectively, and pop is the population.
As we mentioned before health expenditure may not translate on better health infrastructures and for this reason, we should include additional variables focusing on capturing quantity of health resources (hospital, beds, doctors (pediatricians), etc.) as well as their quality that may be approximated by the expenditure or investment in health resources. In this sense, we calculate children’s health resources such as number of pediatric beds or number of pediatricians relative to the number of children younger than 14 years old, since this is the age until usually children are using it. Since all the physicians are able to treat the kids in a general way, we use number of physicians per capita and pediatricians per physicians to find out if there is an effect from specialized doctors (pediatricians).
shows the descriptive statistics. As we have mentioned in the introduction, infant and under-5 mortality level have decreased in an extraordinary way from an average of 39.30 infant death by 1,000 alive kids to 8.10, and similar for kids under-5 from 46.76 to 10.06. However, there is not a big change in the difference between regions as the coefficient of variation shows, and in fact for infant mortality, it has not decreased at all. However, under-5 mortality rate have experienced a small reduction. There are also marked differences between regions and over time in terms of GPD per capita and health expenditure per capita. As the OECD report also point out, Kazakhstan has experienced a great economic growth and put health in the policy agenda, this translates into an increase of the GDP per capita and health expenditure per capita over time. The economic differences between regions slightly decreased and it looks like there was an important reduction on the government health expenditure per capita between regions.
Table 1. Descriptive statistics
Data about health infrastructure for children such as beds (beds per 1,000 children) and share of pediatricians had slightly decreased over time after a small increase at the beginning of the period, even if the share of children under 14 years old is almost the same along the whole period.
4. Results
In order to assess the determinants of infant mortality and under-five child mortality and the effects of health expenditure allocation, we estimate 4 different specifications estimated by system-GMM.Footnote12 We apply diagnose test to all estimation. First order autocorrelation test, AR(1), rejects null hypothesis which states that the moment conditions are valid while second order autocorrelation AR(2) hypothesis is not rejected in any estimation which is consistent with the assumption of Blundell and Bond (Citation1998). Additionally, Hansen test is reported in all estimations for testing the instrument over identification restriction. Hansen test shows problems of identification when we include time dummies and regional-trends, however since we consider that it important to take them into account and we report the estimations excluding them in the appendix.Footnote13
Results for infant mortality of Kazakhstan regions from the period 2000–2018 are shown in . First model specification is quite standard in literature considering GDP per capita, government health expenditure per capita, and control variables such as share of population with access to drinking water, share of female with high education (18–22), sanitation facilities per capita, the degree of urbanization and the share of population younger that 14.Footnote14
Control variables, urbanization rate and share of people younger than 14 turn to be significant and positive, i.e. they increase infant mortality. Population with access to water turns to be negative and significant if we do not control by time dummies and regional trends ( in the Appendix). Additionally, the first specification includes other standard variables in literature such as GDP per capita and Government health expenditure per capita. Nor GDP per capita neither health expenditure per capita appear to be significant when we control by time dummies and regional-trends ().Footnote15 Taking into account that regions are competing by the same national budget we add a variable appending to measure the share of funding received according to the share of population that the regions have. Since it will be almost impossible to detail and estimate government budget specifically dedicated to infants or children under-5, include whole government budget for health and consequently we divide for whole population in each since they are competing for health funding or need to be used to treat whole population and not just children .Footnote16
Table 2. GMM estimation results for explaining infant mortality, time dummies and regional-trends included
Substituting health per capita by indicator of health funding turns the gdp per capita significant and but the indicator does not come significant if we do not control by the time-dummies and regional trends ( in the Appendix). However, if we control by time-dummies and regional-trends () and we include share of funding that national government assigns to each region relative to the population is not enough to measure if government is doing an efficient assignment. In fact, not all regions have the same needs even if they have the same share of population by age-groups, because as we mentioned before regions depart from quite different levels of infant mortality, so government budget assignment may try to correct previous disparities and assigned relative more budget to those regions that have higher infant mortality. To measure this effect, we add the interaction between government budget assignment indicator and the previous year infant mortality (lag of infant mortality). Results show that when government health funds assignment is higher for those regions or regions that have higher level of infant mortality the measure is effective and it reduces infant mortality (interaction coefficient turn to be negative and significant). However, if funds assignment is not related with the level of infant mortality they are not effective and even counterproductive, showing a significant and positive effect (net effect of both effects is negative). This effects loose the power if we don not control by time-dummies and regional trends.
Additionally, as we mentioned in the literature review government health expenditure may not translate in better quality and quantity health resources due to corruption or mismanagement of resources. Therefore, the government health expenditure not always reduce infant mortality. Taking this into account, we also include the level of infrastructure (pediatric beds per capita, physicians per capita, % pediatricians relative to physicians) in order to control by the quality of health infrastructures and the funding allocation. .Footnote17 Results don’t change relative to the previous model specification, and health expenditure assignment reduce infant mortality if it is higher in those region with higher infant mortality if we control by time-dummies and region-trends. Net effect of the share of government health expenditure is negative, i.e. it decreases infant mortality. However, health resources (beds per children under 14 or share of pediatricians) do not turn to be significant. Pediatricians per capita tend to be significant when we do not control by time-dummies and regional trends ().
shows estimation results on under-5 child mortality where we estimate the 4 model specification done for infant mortality. Similar to previous results Share of population younger than 14 appears to be positive and significant while Access to water turn to be significant and negative if we do not control by time dummies and regional-trends ( in the Appendix). GDP per capita turns to be significant and negative for children under-five,Footnote18 and it is consistent with many papers mentioned in the literature where one of the main factors to reduce under-5 child mortality is to increase families income, in this case measured through out GDP per capita. However, government health expenditure per capita doesn’t come to be significant as it happens with the indicator about the government health expenditure assignment at regional level, not in the second specification neither when we interact it with the lag value of under-5 child mortality. Opposite to infant mortality, when we control by time-dummies and regional trends, health infrastructure seems to be more important in case of child mortality. However, it loses significance once we include physicians per capita and GDP per capita. Paper such as Mohanty and Behera (Citation2020) also show how infrastructure can be as important as health expenditure on reducing infant and child mortality.
Table 3. GMM estimation results for explaining under-5 child mortality, time dummies and regional-trends included
5. Discussion
Government health expenditure is a key guarantee to access the health system and maintain and improve human welfare throughout financing and appropriate training of health workers, to provide medical equipment and health infrastructure, and to promote illness prevention throughout promoting immunization, communicable diseases, preventive health services, and food safety, particularly in a large country such as Kazakhstan (Kiross et al., Citation2020). For this reason, an efficient distribution of the resources across regions is essential to reduce current regional disparities on infant and under-5 child mortality rate as well as future productivity, growth, and income disparities. Our results show that it is not enough to assign health resources in terms of population, i.e. potential users, but also more resources where they have worse mortality ratios (as infant mortality estimations show) and to have appropriate number of health infrastructure (as under-5 child mortality estimations prove).
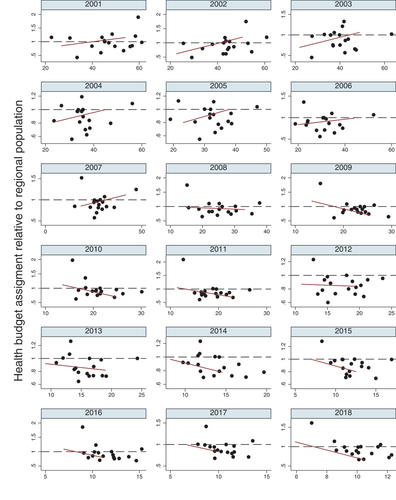
shows the assignment of government health budget relative to the region population in relation with the infant mortality rate of the previous year and it looks like that just at the beginning of the period regional health assignment relative to the population is higher for those regions that experience higher rates of infant mortality.Footnote19 Actually, the period of higher health budget assignment to the regions which need it the most corresponds with the faster decreases in infant and under-5 child mortality rates.
Figure 3. Relationship between government health budget regional distribution and infant mortality ratio of previous year.
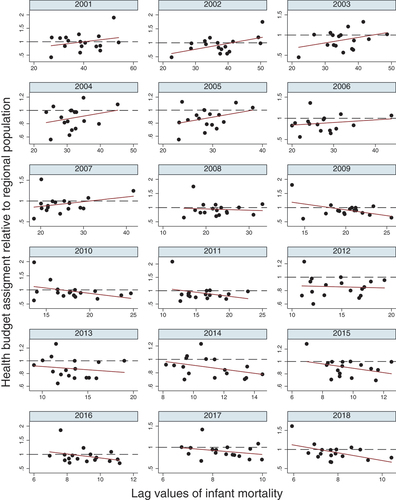
However, it looks when the infant mortality rates started to decrease, then health budget assignment is not so clear. Possible reasons for this may be related to the specifics of the budgetary process in Kazakhstan and the distribution of state budget funds across the regions of the country. Kazakhstan has a two-level budget for financing healthcare—national and sub-national (regional). Overall, 60% of regional government spending is financed by the central government (Beazley et al., Citation2019). The central government allocates the budget to regions via targeted capital transfers, current transfers, and inter-budget general transfers (grants and withdrawals). Thus, the budget allocation of health expenditure not related with health needs may be produced at different levels. First, although the decision-making process on capital investments in different sectors of the economy, including healthcare are regulated by special normative and methodological rules (e.g., The rules for developing or adjusting, conducting the necessary examination of state investment project proposals, as well as planning, considering, selecting, monitoring and evaluating the implementation of budget investments and determining the feasibility of budget lending) and carried out by line ministries and the Ministry of National Economy of Kazakhstan, in many cases decisions are not data-based and demand-driven, but politically determined. For example, as mentioned by Katsaga et al. (Citation2012), a very expensive project called “Construction of 100 schools and 100 hospitals on the basis of public-private partnerships” was not related to the needs of the population in healthcare services but was dictated by political interests. As a result, excessive capacity and expensive medical equipment created and purchased within this kind of projects are not used efficiently enough.
Second, the health budget allocation is mainly determined by historical data, indexation for inflation rates, some regional demographic characteristics (the number and density of population, age, etc.) and to some extent according to spending limits for government programs, new policy initiatives and strategic priorities Beazley et al. (Citation2019). However, the determination of budget limits is not fully related to population needs, that makes healthcare expenditures less effective.
In addition, we have the whole government budget on health, but we cannot distinguish if programs target children or other population groups. It is also true that health expenditure from other population groups may also have spillover effects on children health.
Behera and Dash (Citation2018) suggests the improvement in revenue collection as an instrument to generate fiscal space that may give the possibility to allocate more funds to health.
Thus, the main limitation of this study arises by the unavailability to distinguish health expenditure by types of programs, such as spending on treatment, prevention, and more details on health resources and its quality, for instance, health system capital inputs and health workforce. Access to such data was however difficult, and some of this data is available just for two years, which makes impossible to do the econometric analysis. Additionally, the paper will benefit if it could control by share of private health funds, even if it is out of the scope of this paper.
6. Conclusions
In this paper, we assess the effects of the regional health government expenditure assignment as well as health resources available, such as beds or pediatricians. Results show that a higher health resources assignment in terms of expenditure (particularly for infant mortality) and health resources is actually important to reduce infant and under-5 mortality rate. We take into account that the national government can not increase the budget in all regions and need to distribute. A proper distribution to the regions who need it the most is what actually decreases infant mortality. And this have worked at the beginning of the period when, actually, Kazakhstan experienced a sharp decrease of infant mortality.
As Akinlo and Sulola (Citation2019) point out, policies should focus on improve the efficiency of government expenditure on health, and to ensure that more resources are allocated to primary health care, as well as targeting low income groups and areas that are experience higher infant and child mortality. Unfortunately, in this paper we are not able to distinguish which part of the health expenditure is dedicate to primary health care and which part to hospitality health. OECD (Citation2018) report shows that Kazakhstan inherited a system from Soviet Union, really focused on hospitality resources and need to increase the primary health provision.
Additionally, this paper proves that without a proper allocation of health funds to the regions, regional disparities on health will not decrease and this may result on future income and growth disparities.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1. On the one hand, more than 95% of women in Kazakhstan older than 15 years old had achieved tertiary education level in 2010. i.e. similar levels to Sweden and higher than other countries such as United Kingdom, France, Finland or Spain (Barro-Lee database). On the other hand, immunization rates on HepB3, DPT or measles are around 99%, characteristics of former Soviet Union countries.
2. Other policy measures could be associated with environmental management, infrastructure development, overcoming inequalities and realizing rights (World Health Organization., 2007).
3. Households may divert its funds towards other uses once the government increases its provision of basic health care, using the same total amount.
4. There is not agreement if private expenditure is more health-promoting than private (Dhrifi, Citation2018; Rahman et al., Citation2018) or public health instead (Behera & Dash, Citation2020; Ray & Linden, Citation2020).
5. Actually, authors such Anand and Ravallion (Citation1993) as argue that the effect of income per capita on health outcomes turns insignificant when poverty and government spending variables are controlled for. In fact, children from poor households in low or middle income countries might have up to 2 times higher probability to die compared with children from richer households (Hug et al., Citation2018).
6. This also implies that investments in health outcomes should be continuous.
7. System GMM was not consider in the analysis, only the difference GMM.
8. System GMM solves issues of autocorrelation and unobserved country-specific heterogeneity as well as endogeneity, using lags of the dependent variable, lags of the first-differenced dependent variable and the first differences of the exogenous variables as instruments for the first-differenced equation.
9. Oblasts included are Akmola, Aktobe, Almaty, Almaty city, Nur-Sultan city, Atyrau, East Kazakhstan, Karaganda, Kostanay, Kyzylorda, Mangystau, North Kazakhstan, Pavlodar, South Kazakhstan, West Kazakhstan and Zhambyl. For the year 2018, data for South Kazakhstan is calculated aggregating Shymkent City and Turkestan.
10. According to the new criteria, a live birth is the complete release or removal from the mother’s body of a fetus weighing more than 500 grams, regardless of the gestational age, or at a period of 22 full weeks or more, which is breathing or exhibits other signs of life, such as heartbeat, pulsation of the umbilical cord or arbitrary movement of the muscles. Until 2008, a live birth was considered to be the complete isolation or extraction from the mother’s body of a fetus at a gestational age of 28 weeks or more (i.e., a fetus with a height of 35 centimeters or more, weighing 1000 grams or more), a necessary sign of life is breathing.
11. We have done the same calculation for series of the whole Kazakhstan. Results are in : “corrected” series, and as we can observed it is quite close to correction done by the World Bank.
12. A consistent estimate of lag dependent variable coefficient (lagged infant or under-five mortality) can be expected to lie in between the OLS levels and Within Groups estimates (Hsiao, Citation1986; Nickell, Citation1981), so we have also estimated OLS and within groups estimator to validate the GMM (Results upon request).
13. The coefficients are consistent in both tables although there is changes on significance of some of them partly due to the correlation of the regional trends with some variables such gdp and partly by the weakness of the instruments.
14. Other common control variables such as the degree of immunization were not included because present quite high values and a small degree of variation among regions as we have explained before.
15. However, it seems government health expenditure per capita turns to be significant if we do not control by time dummies and regional-trends ( in the Appendix).
16. Although, using whole health expenditure per capita instead of health expenditure on children should actually make this variable less endogenous, the statistical test shows that behaves in a endogenous way and we need to correct it.
17. Health resources also come out to be endogenous when control by time-dummies and country trends. In fact, The correlation may go in one or both directions, for instance, the number of pediatricians might decrease the mortality rate, but also this rate may affect the future pediatricians number.
18. The effect is even weaker when we do not control by time-dummies and regional trends .
19. Results are similar for under-5 child mortality in Table A3 in the appendix (6).
References
- Akinlo, A. E., & Sulola, A. O. (2019). Health care expenditure and infant mortality in sub-Saharan Africa. Journal of Policy Modeling, 41 (1), 168–23. https://doi.org/10.1016/j.jpolmod.2018.09.001
- Anand, S., & Ravallion, M. (1993). Human development in poor countries: On the role of private incomes and public services. Journal of Economic Perspectives, 7(1), 133–150. https://doi.org/10.1257/jep.7.1.133
- Anderson, T. W., & Hsiao, C. (1982). Formulation and estimation of dynamic models using panel data. Journal of Econometrics, 18(1), 47–82. https://doi.org/10.1016/0304-4076(82)90095-1
- Arellano, M., & Bond, S. (1991). Some tests of specification for panel data:monte carlo evidence and an application to employment equations. Review of Economic Studies, 58(2), 277–297. https://doi.org/10.2307/2297968
- Asiedu, E., Freeman, J. A., & Nti-Addae, A. (2012). Access to credit by small businesses: How relevant are race, ethnicity, and gender. American Economic Review, 102(3), 532–537. https://doi.org/10.1257/aer.102.3.532
- Asiedu, E., Gaekwad, N. B., Nanivazo, M., Nkusu, M., & Jin, Y. (2015). On the impact of income per capita on health outcomes: Is Africa different? Is Africa different. Journal of Economic Literature, 23(11), 24-33. https://www.aeaweb.org/conference/2016/retrieve.php?pdfid=13860&tk=ENGKZGkh Semantic Scholar
- Auster, R., Leveson, I., & Sarachek, D. (1969). The production of health, an exploratory study. The Journal of Human Resources, 4(4), 411. https://doi.org/10.2307/145166
- Baird, R., Friedman, J., & Schady, N. (2011). Aggregate income shocks and infant mortality in the developing world. Review of Economics and Statistics, 93(3), 847–856. http://direct.mit.edu/rest/article-pdf/93/3/847/1918948/rest_a_00084.pdf
- Beazley, I., Downes, R., & Nicol, S. Budgeting in Kazakhstan A roadmap for continued for continued budgetary governance reform. Technical Report 3, 2019.
- Behera, D. K., & Dash, U. (2018). The impact of macroeconomic policies on the growth of public health expenditure: An empirical assessment from the Indian states. Cogent Economics and Finance, 6(1), 1435443. http://doi.org/10.1080/23322039.2018.1435443.
- Behera, D. K., & Dash, U. (2020). Is health expenditure effective for achieving healthcare goals? Empirical evidence from South-East Asia Region. Asia-Pacific Journal of Regional Science, 4(2), 593–618. https://doi.org/10.1007/s41685-020-00158-4
- Bhalotra, S. (2007). Spending to save? State health expenditure and infant mortality in India. Health Economics, 16(9), 911–928. https://doi.org/10.1002/hec
- Bhalotra, S. (2010, 9). Fatal fluctuations? Cyclicality in infant mortality in India, Journal of Development Economics, 93(1), 7–19. https://doi.org/10.1016/j.jdeveco.2009.03.006
- Black, R. E., Victora, C. G., Walker, S. P., Bhutta, Z. A., Christian, P., De Onis, M., Ezzati, M., Grantham- Mcgregor, S., Katz, J., Martorell, R., & Uauy, R. Maternal and child undernutrition and overweight in low-income and middle-income countries. 2013.
- Blundell, R., & Bond, S. (1998). Initial conditions and moment restrictions in dynamic panel data models. Journal of Econometrics, 87(1), 115–143. https://doi.org/10.1016/S0304-4076(98)00009-8
- Bokhari, F. A., Gai, Y., & Gottret, P. (2007, 3). Government health expenditures and health outcomes, Health Economics, 16(3), 257–273. https://doi.org/10.1002/hec.1157
- Bönke, T., & Schröder, C. (2011). Poverty in Germany - statistical inference and decomposition. Jahrbucher Fur Nationalokonomie Und Statistik, 231(2), 178–209. https://doi.org/10.1515/jbnst-2011-0202
- Cantó, O., & Luis, A. (2014). Políticas públicas para reducir la pobrez infantil en España: Análisis de impacto. UNICEF Comité Español, Madrid. https://www.unicef.es/sites/unicef.es/files/unicef_politicas_para_reducir_pobreza_infantil_espana_baja.pdf
- Dhrifi, A. (2018). Health-care expenditures, economic growth and infant mortality: Evidence from developed and developing countries. Cepal Review, 2018(125), 71–97. https://doi.org/10.18356/02c1a26c-en
- Dieleman, J., Campbell, M., Chapin, A., Eldrenkamp, E., Fan, V. Y., Haakenstad, A., Kates, J., Liu, Y., Matyasz, T., Micah, A., Reynolds, A., Sadat, N., Schneider, M. T., Sorensen, R., Evans, T., Evans, D., Kurowski, C., Tandon, A., Abbas, K. M., & Murray, C. J. (2017). Evolution and patterns of global health financing 1995-2014: Development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. The Lancet, 389(10083), 1981–2004. https://doi.org/10.1016/S0140-6736(17)30874-7
- Farag, M., Nandakumar, A. K., Wallack, S., Hodgkin, D., Gaumer, G., & Erbil, C. (2013). Health expenditures, health outcomes and the role of good governance. International Journal of Health Care Finance and Economics, 13(1), 33–52. https://doi.org/10.1007/s10754-012-9120-3
- Filmer, D., & Pritchett, L. (1999). The impact of public spending on health: Does money matter? Social Science & Medicine, 49(10), 1309–1323. https://doi.org/10.1016/S0277-9536(99)00150-1
- Grossman, M. (1972). On the concept of health capital and the demand for health. The Journal of Political Economy, 80(2), 223–255. https://doi.org/10.1086/259880
- Harttgen, K., Klasen, S., & Vollmer, S. (2013). Economic growth and child undernutrition in sub-Saharan Africa. Population and Development Review, 39(3), 397–412. https://doi.org/10.1111/j.1728-4457.2013.00609.x
- Headey, D. D. (2013, 2). Developmental drivers of nutritional change: A cross-country analysis, World Development, 42(1), 76–88. https://doi.org/10.1016/j.worlddev.2012.07.002
- Hsiao, C. (1986). Analysis of panel data Econometric society monographs. Cambridge University Press https://doi.org/10.1017/9781009057745.
- Hug, L., Sharrow, D., Zhong, K., You, D., Ho, J., Retno Mahanani, W., Ma Fat, D., Grove, J., Bay, G., Black, R., Hopkins, J., Alkema, L., Cousens, S., Masquelier, B., Pedersen, J., & Neff Walker, F. Special thanks to the technical advisory group of the UN IGME for providing technical guidance on methods for child mortality estimation. Technical report, 2018.
- Jakovljevic, M. B., Vukovic, M., & Fontanesi, J. (2016, 7). Life expectancy and health expenditure evolution in Eastern Europe—DiD and DEA analysis, Expert Review of Pharmacoeconomics & Outcomes Research, 16(4), 537–546. https://doi.org/10.1586/14737167.2016.1125293
- Jakovljevic, M., Timofeyev, Y., Ekkert, N. V., Fedorova, J. V., Skvirskaya, G., Bolevich, S., & Reshet-nikov, V. A. (2019b). The impact of health expenditures on public health in BRICS nations. Journal of Sport and Health Science, 8(6), 516–519. https://doi.org/10.1016/j.jshs.2019.09.002
- Judson, R. A., & Owen, A. L. (1999). Estimating dynamic panel data models: A guide for macroeconomists. Economics Letters, 65(1), 9–15. https://doi.org/10.1016/s0165-1765(99)00130-5
- Katsaga, A., Kulzhanov, M., Karanikolos, M., & Rechel, B. Kazakhstan: Health system review. Health Systems in Transition, 14(4), 1–154. 2012.
- Kemna, H. J. (1987). Working conditions and the relationship between schooling and health. Journal of Health Economics, 6(3), 01676296. https://doi.org/10.1016/0167-6296(87)90008-7
- Kiross, G. T., Chojenta, C., Barker, D., & Loxton, D. (2020). The effects of health expenditure on infant mortality in sub-Saharan Africa: Evidence from panel data analysis. Health Economics Review, 10(1), 1–9. https://doi.org/10.1186/s13561-020-00262-3
- Mohanty, R., & Behera, D. (2020). How effective is public health care expenditure in improving health outcome? An empirical evidence from the Indian States. Working Papers, 1–29. https://www.nipfp.org.in/publications/working-papers/1897/
- Muldoon, K. A., Galway, L. P., Nakajima, M., Kanters, S., Hogg, R. S., Bendavid, E., & Mills, E. J. (2011). Health system determinants of infant, child and maternal mortality: A cross-sectional study of UN member countries. Globalization and Health, 7(1), 10. https://doi.org/10.1186/1744-8603-7-42
- Musgrove, P. Public and private roles in health theory and financing patterns. Technical report, 1996.www.worldbank.org
- Nickell, S. (1981). Biases in dynamic models with fixed effects. Econometrica, 49(6), 1417–1426. https://doi.org/10.2307/1911408
- Novignon, J., & Lawanson, A. O. (2017). Health expenditure and child health outcomes in Sub-Saharan Africa. African Review of Economics and Finance-Aref, 9 (1), 96–121. https://www.ajol.info/index.php/aref/article/view/162145
- Nwude, E. C., Ugwoke, R. O., Uruakpa, P. C., Ugwuegbe, U. S., & Nwonye, N. G. (2020). Official development assistance, income per capita and health outcomes in developing countries: Is Africa different? Cogent Economics and Finance, 8 (1), 1774970. https://doi.org/10.1080/23322039.2020.1774970.
- Nyamuranga, C., & Shin, J. (2019). Public health expenditure and child mortality in Southern Africa. International Journal of Social Economics, 46(9), 1137–1154. https://doi.org/10.1108/IJSE-12-2018-0643
- OECD. (2018). Kazakhstan 2018. Review of Health System.
- Pamuk, E. R., Fuchs, R., & Lutz, W. (2011). Comparing relative effects of education and economic resources on infant mortality in developing countries. Population and Development Review, 37(4), 637–664. https://doi.org/10.1111/j.1728-4457.2011.00451.x
- Poudel, S., Adhikari, C., Yadav, R. K., Yadav, D. K., Thapa, D. K., & Jakovljevic, M. (2022). Disempowered mothers have undernourished children: How strong is the intrinsic agency? Frontiers in Public Health, 10(February), 1–8. https://doi.org/10.3389/fpubh.2022.817717
- Rahman, M. M., Khanam, R., & Rahman, M. (2018). Health care expenditure and health outcome nexus: New evidence from the SAARC-ASEAN region. Globalization and Health, 14(1), 113. https://doi.org/10.1186/s12992-018-0430-1
- Ray, D., & Linden, M. (2020). Health expenditure, longevity, and child mortality: Dynamic panel data approach with global data. International Journal of Health Economics and Management, 20 (1), 99–119. https://doi.org/10.1007/s10754-019-09272-z
- Roodman, D. (2009a). Practitioners’ corner: A note on the theme of too many instruments. Oxford Bulletin of Economics and Statistics, 71(1), 135–158. https://doi.org/10.1111/j.1468-0084.2008.00542.x
- Roodman, D. (2009b). How to do xtabond2: An introduction to difference and system GMM in Stata. Stata Journal, 9(1), 86–136. https://doi.org/10.1177/1536867x0900900106
- Sommer, J. M. (2020). Accountable government spending: A cross-national analysis of child mortality in developing nations. International Journal of Health Services, 52(1), 73-88. https://doi.org/10.1177/0020731420960972
- Soto, M. (2007). System GMM estimation with a small number of individuals. Institute for Economic Analysis, 1–28. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.465.9928&rep=rep1&type=pdf
- Stenberg, K., Axelson, H., Sheehan, P., Anderson, I., Gülmezoglu, A. M., Temmerman, M., Mason, E., Friedman, H. S., Bhutta, Z. A., Lawn, J. E., Sweeny, K., Tulloch, J., Hansen, P., Chopra, M., Gupta, A., Vogel, J. P., Ostergren, M., Rasmussen, B., Levin, C., … Bustreo, F. Advancing social and economic development by investing in women’s and children’s health: A new global investment framework. (2014). The Lancet, 383(9925), 1333–1354. https://doi.org/10.1016/S0140-6736(13)62231-X.
Appendix
Table A1. Definitions of indicators
Table A2. GMM estimation results for explaining infant mortality
Table A3. GMM estimation results for explaining under-5 child mortality