 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Children cope with high temperatures differently than adults do, largely because of slight alterations in their body proportions and heat loss mechanisms compared to fully mature humans. Paradoxically, all current tools of assessing thermal strain have been developed on adults. As the Earth’s warming continues to accelerate, children are set to bear the health risk brunt of rising global temperatures. Physical fitness has a direct impact on heat tolerance, yet children are less fit and more obese than ever before. Longitudinal research reveals that children have 30% lower aerobic fitness than their parents did at the same age; this deficit is greater than can be recovered by training alone. So, as the planet’s climate and weather patterns become more extreme, children may become less capable of tolerating it. This comprehensive review provides an outline of child thermoregulation and assessment of thermal strain, before moving to summarize how aerobic fitness can modulate hyperthermia, heat tolerance, and behavioral thermoregulation in this under-researched population. The nature of child physical activity, physical fitness, and one’s physical literacy journey as an interconnected paradigm for promoting climate change resilience is explored. Finally, future research foci are suggested to encourage continued exploration of this dynamic field, notable since more extreme, multifactorial environmental stressors are expected to continue challenging the physiological strain of the human population for the foreseeable future.
Introduction
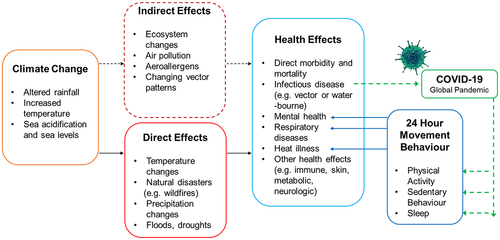
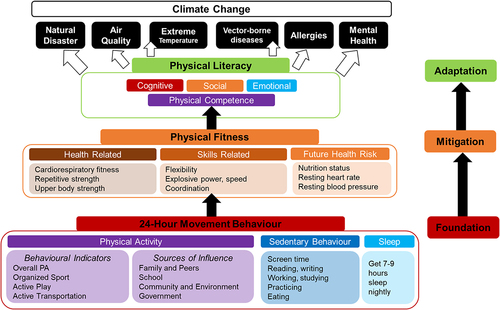
Planet Earth is rapidly becoming an extreme environment for humans to survive and thrive upon, especially considering most of the world’s population live in tropical zones. For example, the current increase in global surface temperature is estimated to be 1.09°C in 2011–2020 above temperatures observed from the y 1850–1900 [Citation1]. This estimated increase in global surface temperature is thought to be principally due to the additional warming occurring between 2003 and 2012 (+0.19°C), with at least a 50% likelihood that global warming will reach (or exceed) 1.5°C in the near-term, even for “very low” greenhouse gas emission scenarios [Citation1]. The World Health Organization (WHO) defines ‘health” in its 1946 constitution as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [Citation2], a lofty challenge for present-day humans to achieve. While the world is getting hotter[Citation3], children are becoming less fit [Citation4–6] and more obese [Citation7], and climate change will increase the likelihood of novel vector-borne diseases entering the human population [Citation8,Citation9], rendering the possibility of further movement restrictions to novel disease outbreaks likely, itself creating a vicious-cycle of isolation, physical de-training[Citation10], and increased risk for heat injury [Citation11], especially for vulnerable populations [Citation12], like prepubescent children [Citation13]. Isolation and detraining are well-researched areas in environmental and space physiology [Citation14,Citation15], but not often associated with the indirect effects of climate change. With global warming projections suggesting, at minimum, a 2°C increase in global average temperatures by the year 2100 [Citation9],including the disruption of ecosystem balance and extreme weather events that come with these increases), current climate change policies do not address child health needs in adequate or robust ways [Citation16,Citation17]. A child born today will be affected by climate change throughout their lifetime, both directly (e.g. wildfires, floods) and indirectly (e.g. aeroallergens, altered disease vectors; ) [Citation8]. Future heat exposures will exceed critical levels for physically active humans far more often than occurs today [Citation18]. Current extreme heat risk projections oversimplify critical inter-individual human thermoregulatory factors, which result in unreliable, and often unrealistic, estimates of future adverse health outcomes [Citation19]. Climate change can also act as both a cause or consequence to greater physical inactivity [Citation20], especially in vulnerable populations, like children, or the elderly.
Figure 1. Climate change impacts on human health. The effects of climate change will exert both direct and indirect outcomes on human health, which may seriously affect the 24-hour movement behavior patterns of people. One example outlined here pertains to the COVID-19 pandemic outbreak, resulting from the introduction of a novel coronavirus pathogen to the human species with concomitantly strong mitigation measures aimed at reducing virus spread. However, these societal measures also directly impacted billions of people’s ability to move freely, causing significant barriers to remain physically active. These rapidly evolving measures are not conducive to maintaining adequate or optimal health over the past 2 y. Remaining confined for days, weeks, or sometimes months on end can significantly impair one’s mental health, affect respiratory health, and may place certain individuals at greater risk of suffering heat illness, especially if confinement periods coincide with extreme weather events. Similar negative feedback loops may occur as a result from direct (e.g. flooding, wildfire, heat), or indirect (e.g. air pollution, seasonal allergy severity) climate change effects further exacerbating negative 24-hour movement behaviors.
In terms of human thermoregulation, children are not simply smaller adults. Children have greater surface-area-to-mass ratio, lower sweating rates, and higher peripheral skin blood flow in the heat than adults (reviewed in [Citation21–24]). Children’s decreased heat storage capacity means they are more reliant on so-called “dry” mechanisms of heat exchange (conduction, convection) compared to adults [Citation21]. Although kids acclimatize to heat, they do so more slowly than their adult counterparts [Citation22]. When children play, they may be at greater health risk as body temperatures rise [Citation25] and heat dissipation potential is progressively reduced moving in the hot environment. Repeated exercise in the heat leads to physiological adaptation [Citation26], reducing heat strain (see detailed review [Citation27]). Unfortunately, information on active/exercising heat strain in children is lacking. Recent evidence has suggested that behavioral thermoregulation can be compromised in small children who depend on supervisory control [Citation28]. Although caretakers in day-care centers were able to accurately assess their own thermal status, they were not able to gauge the children’s, nor could they correctly recall symptoms of temperature-related illness [Citation28]. This poses an additional risk of heat strain for small children. Over two decades ago, research on heat strain in children was more prevalent [Citation23,Citation29–31]. Today, WHO policy briefs [Citation17,Citation32], the new Lancet series on climate change and child health [Citation8,Citation33], and thermal physiologists [Citation24,Citation25,Citation34] all agree that climate change and child health is an urgent public health concern [Citation8,Citation16], especially since, of all the adaptive heat stress studies available (mostly conducted in adults), those which do target children mostly come from an era when fitness levels were much higher.
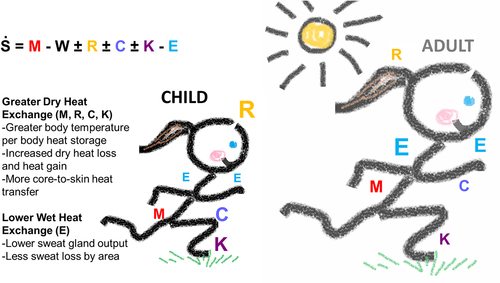
Thermal strain assessment in children
Elevated core temperature provides is one way heat loss mechanisms are activated in humans [Citation35] to avoid thermal injury and premature fatigue [Citation36,Citation37]. These mechanisms can be both autonomic and behavioral in nature [Citation38] and include active vasodilation of shunt vessels, and activation of eccrine sweat glands [Citation38]. Heat is then dissipated primarily via dry (radiation, convection) and wet (evaporation) mechanisms (, concept adapted from Ref. [Citation35]). The radiant energy from the sun can contribute a significant heat load when exercising in a natural environment [Citation39] or in simulated lab environment [Citation40]. and increased heat production from metabolic workload further accentuates rising core temperatures [Citation41]. Indeed, exercise itself is a pyrogenic activity [Citation42]. Airflow (even warm, ambient temperature airflow [Citation43]) can impact both dry and evaporative heat transfer, but is often not sufficiently considered in most lab-based research [Citation44]. The ability to maintain heat balance (S) in a given environment relies on an individual’s metabolic storage (M), their external work rate (W), radiative (R), convective (C), conductive (K), and evaporative (E) heat exchange, which also depend on one’s cardiovascular and sweat response capabilities. Thus, heat storage is the essential parameter when assessing heat strain. Heat storage is calculated as the difference between heat lost and heat produced, and estimated as an invariant weighting system between mean core and mean skin temperatures (), with the relative contribution of each compartment (core/skin) expressed as a ratio [Citation45] assuming a specific heat capacity of the body (per unit tissue). At best, some investigations have found that estimating changes in mean body temperature using core and skin temperature weightings are inaccurate in exercising humans, even when applying a correction factor [Citation46]. More worrying is the fact that accurately and validly assessing
has not been robustly revisited since the original research was first conducted in the early 20th century (i.e. 1914–1918), especially in terms of the pediatric population. Two of the most commonly cited references in exercise physiology for determining body surface area [Citation47] and
weightings in humans [Citation48] e.g. latter cited ~1842 times (Google Scholar), are not validated in children, performed on only N = 3 healthy, male (Caucasian) participants, and demonstrating acceptable levels of statistical accuracy (at best) less than 60% of the time[Citation49] and even falling to less than 15%[Citation50]. Despite this fact, researchers continue to use these weightings widely. Presently, there is no true “gold-standard” for determining
, but the closest for whole-body assessment is the International Standard Organization (ISO 9886) 14-site model [Citation51] where each site is worth 0.071 (i.e. 1/14) of: forehead, neck, right scapula, left upper chest, right upper arm, left lower arm, left hand, right abdomen, left paravertebral, right anterior thigh, left posterior thigh, right shin, left calf, right foot instep. The data upon which this standard was based is thought to originate from an earlier 16-point model communicated at an American Society of Heating, Refrigerating and Air-Conditioning Engineers conference in 1972 [Citation52], which itself was created as a measure of thermal sensation and not of skin temperature per se. This model is unweighted because each temperature measurement site is supposed to represent an equal amount of skin surface area, and yet, body proportions vary considerably with age [Citation53] rendering this weighting system, by definition, inaccurate when applied to a child. Aside from
measurement, it is also important to reiterate here that the “skin” as an organ structure is highly heterogeneous [Citation54], and a critical component to thermoregulation in its own right, including driving thermal comfort [Citation55,Citation56]. Thus, updated, objective data on skin temperature responses in children are needed.
Figure 2. Mechanisms of heat exchange in children. The ability to maintain heat balance (S) relies on an individual’s metabolic storage (M), their external work rate (W), radiative (R), convective (C), conductive (K), and evaporative (E) heat exchange. Children’s (supposedly) decreased heat storage capacity compared to adults means they are more reliant on so-called “dry” mechanisms of heat exchange (conduction, convection) to maintain heat balance.
Using thermal indices and models for heat stress assessment is not a new phenomenon. In 1905, Haldane presented his argument that a wet-bulb temperature would be a better indicator of physiological effects than dry bulb temperature alone in certain conditions (e.g. hot, wet, confined)[Citation57]. The subsequent Wet Bulb Globe Temperature (WBGT) index was initially developed in the 1940–1950s in response to a number of military personnel suffering fatal heat stroke during trainings (reviewed in Ref. [Citation58]). WBGT is based on two (or three in solar radiation) sensors; a 15 cm diameter black globe with a temperature sensor floating in its center, and a thermometer that is covered with a suspended wet wick which is in contact with wind and radiation, thus taking into account the main factors responsible for heat exchange [Citation59]. WBGT is widely used in both industrial [Citation60] and sporting contexts [Citation61], and can be relatively easily calculated based on standard meteorological measurements [Citation62], but the index does not consider a number of important factors like clothing insulation or exercise (metabolic heat production). Today, the Universal Thermal Climate Index (UTCI [Citation63], justified here [Citation64]) is the most comprehensive model for characterizing exercising heat strain in humans. Developed from a European COST action, it was created to represent outdoor thermal environments more accurately, considering the dynamic nature of human thermoregulation, fitness, clothing type, anthropometry, and more. Although recent work has looked at quantifying the impact of heat and climate change on work capacity in adults [Citation65] using these models, no such effort has yet been afforded to exercising children.
The pediatric population presents unique challenges for assessing heat stress because they differ in both morphology and physiology to human adults. Child–adult differences in body mass and (less substantially) body composition can influence heat-storage capacity. Children have greater surface-area-to-mass ratio, lower sweating rates, and higher peripheral skin blood flow in the heat than do adults (reviewed in Refs [Citation21–23]). Evidence reported by Arlegui and colleagues found that prepubertal children’s regional sweat rates differ compared to adults [Citation66], possibly affecting mathematical models used in human thermoregulation at present when they are applied to the pediatric population. Classical exercise studies in children have found them to be more reliant on so-called “dry” mechanisms of heat exchange (conduction, convection) compared to adults [Citation21]. Moving more blood to the skin during times of exercising heat stress requires an increase in cardiac output [Citation67] (i.e. the volume of blood pumped out of the heart expressed as a rate, usually per minute), and since cardiac output is comparable between children and adults (when taken relative to fat-free mass [Citation68]), young ones may not have the reserve required to meet the proportionally greater demands of elevated skin blood flow. If exercise continues vigorously in the heat, skin blood flow can be sacrificed preferentially to maintain arterial blood pressure [Citation69], which might compromise heat loss further in children, who rely more heavily on this action for heat loss. All this to say, children do not necessarily possess a thermoregulatory system that is inadequate or worse than adults [Citation23,Citation70], only that it operates differently and needs to be considered based on the environmental conditions presented.
Moving and working in higher ambient temperatures
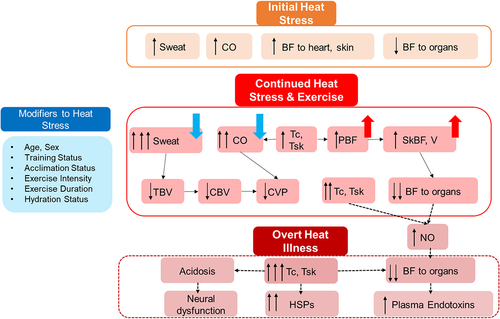
Death, heat stroke morbidity, heat exhaustion, dehydration, and/or central nervous system malfunction can each be associated with intense heat exposure according to the WHO [Citation71] and the Intergovernmental Panel on Climate Change (IPCC) [Citation72]. It has been reported that of the almost half of the global population (including >1 billion workers) exposed to “high heat episodes” (usually defined by regional weather criteria), one-third of those exposed report negative health effects [Citation73]. Simply having elevated skin temperature increases ones’ heart rate and perception of effort [Citation74]. Heatwaves and high heat exposures are responsible for labor loss and health risks in industries like agriculture [Citation75], and others [Citation76], and although less is known regarding child labor in these circumstances, we know that hyperthermia can impair complex motor task performances [Citation77], and direct exposure of solar heat to the head affects motor-cognitive outcomes [Citation40]. It is clear one country’s “hot” day is another country’s “mild” one, where mortality trends to sudden increases in ambient temperature follow vastly different patterns, whether in Helsinki, London, Beijing, Taiwan, or Lille, France, for example. What remains is that when humans get “hot,” it places a tremendous burden on the cardiovascular system [Citation67,Citation78–80]; heart rate increases, and there are significant decreases to central blood volume, right atrial pressure [Citation69], mean pulmonary artery pressure, pulmonary capillary wedge pressure [Citation81], left atrial volumes [Citation82], and total peripheral resistance [Citation78] for humans of any age (). With decreases seen in stroke volume prevalent during heat stress, maintaining cardiac output falls solely on one’s capacity to increase heart rate to meet blood delivery demands, a challenge currently not well established for hot, exercising children, especially those of varying levels of cardiorespiratory fitness, highlighting the important role that blood (flow, volume, consistency) plays for both the thermoregulatory and cardiovascular purposes. Since the control of skin blood flow and volume share effector loops for both the control of body temperature and blood pressure, respectively, this dual innervation can inherently cause competition between systems, and lead to the physiological failure experienced during severe heat stress, ultimately causing heatstroke if left unchecked [Citation80].
Figure 3. Simplified schematic of conflicts arising within the cardiovascular system during continued heat exposure and exercise. Serious physiological consequences to increased heat load can include hyperthermia, endotoxemia, cerebral hypoxia, and potentially death, in extreme cases. The dashed box depicts physiological responses that can occur during exertional heat stress, although at what point normal responses to heat turn to clinically problematic levels of heat illness will depend on many factors, including (but not limited to) some highlighted in the “modifiers” box listed on the left-hand side of this figure. Certain functions which occur normally in response to exercising in a hot environment, (and are necessary for stimulating positive heat acclimation processes) are depicted above the dashed line, but at a certain point, the heat strain accrued can become a clinical concern. Blue downward arrows indicate a factor which may be downregulated or less impactful in children, whereas red upward arrows indicate a factor which children may experience to greater extent relative to fully mature humans. Abbreviations: CO, cardiac output; BF, blood flow; PBF, peripheral blood flow; PBV, peripheral blood volume; TBV, total blood volume; CBV, central blood volume; CVP, central venous pressure; V, volume; Tc, core temperature; Tsk, skin temperature.
Children may become at greater heat risk in a future warming world since the current generation of young people are less fit [Citation6,Citation83] and more obese [Citation7] than previous generations, especially more so over the past 30 y. One investigation from Bangkok, Thailand, studied 457 schoolboys (aged 5.5–12 y) and observed that, expectedly, tympanic temperature was elevated while the boys exercised outdoors during their physical education classes [Citation84]. The authors found that the incidence rate of increased body temperatures (up to 38°C) in overweight students was 2.1-fold higher than normal weight students, and that maximal levels of heat stress were found during afternoon classes in the first semester, when WBGT was 33.9°C and relative humidity was 48.5% [Citation84]. For comparison, the authors reported that WBGT in semesters 1 and 2 (i.e. July–Sept 2009) were 29.95 ± 1.87°C and 28.32 ± 2.39°C. More recent work conducted in the United States reports that of >3.8 million emergency department visits (to 47 participating children’s hospitals) during high heat days, patients were more likely to be male (53.1% versus 46.9%) and younger (54.4%, 0–5 y; 27.8%, 6–12 y; and 17.8%, 13–18 y of age) [Citation85]. Data were obtained between May and September (2016–2018). Researchers found that the hotter days were associated with higher relative risk of emergency department visits for all causes, including heat-related illnesses, bacterial enteritis, infectious and parasitic diseases, and nervous system diseases, among others [Citation85]. Data are similar for adults, where days of extreme heat in the United States were associated with an excess absolute risk of emergency department visits for heat-related illness of 24.3 per 100,000 (95% confidence interval: 22.9–25.7) people per day [Citation86]. It should be noted that there is inherent complexity when one is studying or generalizing physiological responses in children, due to variations in their developmental stages, different rates of development and non-uniform classifications between organizations (e.g. for pubertal stages, chronological age groups, etc.). Regarding risk of heat illness, children are (arguably) at greatest risk when there are extremes in temperature (including humidity), and this risk will vary across age groups/developmental stages, with greatest risk seen in younger ones[Citation24]. Direct epidemiological research on health risk or odds ratio for suffering a heat-related injury determined by age and stage, taking into account a child’s aerobic training and/or acclimation status have not yet been determined in the literature.
In adults, we know that aerobic training confers higher sweat rates and smaller rises in core temperature during uncompensable heat stress [Citation87]. Higher aerobic fitness provides multiple structural and functional adaptations also to the cardiovascular system which better enable it to meet the competing demands upon cardiac output [Citation67,Citation88]. Aerobically fit people are also better able tolerate higher temperatures [Citation89], consistently underestimating their actual physiological heat strain [Citation90]. Notably, mechanisms of thermal strain can be physiological or non-thermal in nature [Citation91]. As mentioned previously, when children play in hotter ambient temperatures, they might be at greater health risk for suffering heat-related illness compared to playing in a cooler environment as their body temperatures rise from their physical activity [Citation25]. Conversely, exercise in the heat also leads to physiological adaptation, reducing heat strain. During hot summer periods, children may not take appropriate steps to avoid heat illness/injury (e.g. drinking more water, moving into the shade, stop playing). Researchers have found that hydration status is considerably better-maintained when children drink flavored versus unflavored water [Citation92]. Recent studies in this field are lacking the direct evidence for elucidating mechanisms between cardiac function, fitness state, and heat tolerance in children; updated data on these physiological responses would be hugely beneficial from a mechanistic and population health perspective, especially to determine causality between the heat stress experienced in childhood and one’s future health risk to high heat events as a fully mature adult. Repeated exposure to high heat in either natural settings or lab-induced adaptations to facilitate better fluid balance and increase cardiovascular stability (reviewed in Ref. [Citation27]) may be a useful and protective countermeasure later in life.
In adults, many relevant adaptations occur within the first week of heat acclimation [Citation93,Citation94], including plasma volume expansion, reduced heart rate at a given work rate, reduced core and skin temperatures, and improved thermal comfort; sweat rate increases more slowly. With heat acclimation aerobic exercise capacity is increased. To this point, a recent meta-analysis has found that (in adults) aerobic fitness is the most effective mitigation strategy in terms of one’s ability to alter core temperature [Citation95], even greater than heat acclimation itself. It must also be mentioned that heat acclimation is a highly individualized response, with some research demonstrating, for example, negligible effects on thermoregulation in trained individuals residing in the tropics [Citation96]. Previous work has clearly shown that heat exposure and/or heat adaptation induce significant up-regulation of protective molecules (e.g. heat shock proteins, HSPs and hypoxia-inducible factor 1-alpha) and related downstream factors [Citation97]. Oxidative stress and antioxidant capacity are modulated by many external factors, e.g. heat exposure and hypoxia [Citation98]. These modulations exert profound effects on physiological status, health, and wellbeing in humans, and have not been investigated thoroughly in children. Meaningful, mechanistic, insights are needed to determine whether heat stress can be protective to heat tolerance in children, and if so, identify where along the oxidative pathway this is likely to occur. Finally, it is important to note that although thermotolerance is conferred partly by high fitness, there are also behavioral elements that are learned. For example, water intake increases with heat acclimation since sweat rate increases and (especially) sodium retention is optimized. In other words, heat acclimated people retain more salt, which provides a drive for thirst, facilitating better hydration maintenance in those who are heat acclimated compared to those who are not. There is evidence that children voluntarily dehydrate when moving in hot conditions [Citation99–101]. To what extent thirst drives drinking behavior in children can be explored further, especially through the lens of behavioral thermoregulation in prepubescent children who sweat less than fully mature people.
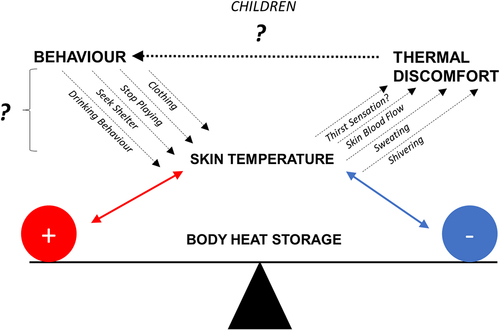
Children would thus benefit on multiple fronts to a heat acclimation protocol in terms of acute, physiological responses (e.g. lower resting core temperatures, lower cardiovascular strain due to plasma volume expansion, etc.) but also in terms of behavioral queues (e.g. thirst sensation). For example, Schlader reiterated in his article, that in animal-based research, there are repeated examples where behavior is the more (most) preferred, powerful, and diverse thermoregulatory response [Citation102] compared to physiological adaptation per se. In their model, the importance of skin temperature is highlighted to stress that one’s behavior to changes in skin temperature can effectively modulate overall temperature regulation. Unfortunately for children, there is very little information on how they “perceive” heat, cold, changes in their internal body temperature, to what extent skin temperature may modify their responses, or whether (if given the opportunity) they are able to make sound behavioral choices based on how they feel (), especially when playing or engaged in outdoor physical activity. As such, thermal comfort and sensation in young ones is an area ripe for exploration, and one which should be revisited to determine whether there are meaningful differences between ages, maturity, training status, or other factors.
Figure 4. Skin temperature as a modulator of core temperature. When humans are given the opportunity to behaviorally thermoregulate, they may choose from a variety of activities that can directly affect skin temperature, which in turn (eventually) modifies core temperature. However, it is not known to what extent (i.e. how powerful) behavioral thermoregulation affects temperature regulation in children, especially young ones who may be dependent on supervisory control. This is a health risk concern, especially since prepubescent children who are under heat stress see changes in skin blood flow to a relatively greater extent than fully mature humans. Children may therefore experience greater (or sometimes lesser) thermal strain to a given environment compared to adults. They may also not be aware of how they are feeling when moving in a hot environment.
Children who compete in the heat
Many young athletes train and compete in conditions that place high demands on their body’s thermoregulatory system, including elevated ambient temperatures and/or in humid conditions. These environmental factors, coupled with the metabolic cost of exercise (and in sports requiring protective equipment) can place children at risk for thermal or fluid imbalance (i.e. perturbations in body water content within the intra- and extracellular compartments, as well as whole-body electrolyte concentrations). Hypohydration, a decrease in whole-body water stores due to combined water and electrolyte losses in sweat, is usually the major health concern during exercise in the heat, whereas hyperhydration is typically a less frequent concern. Relative to body size, children demonstrate less total sweat water and sodium losses during exercise than adults (0.25–0.65 L ∙ h−1 and 0.19–0.27 g ∙ h−1 Na+ loss vs 1.5–3.0 L ∙ h−1 and 0.8–4.0 g ∙ h−1 Na+ loss, in children vs adults, respectively) [Citation99]. There have been numerous studies investigating the thermoregulatory demands of young athletes participating in club or school sport, with particular focus paid to American football [Citation103,Citation104] and elite tennis [Citation105–107]. Unsurprisingly, some authors have found that junior tennis players who began their match poorly hydrated demonstrate progressively increasing thermal strain, and possibly greater risk of exhibiting exertional heat illness as the match progresses [Citation107]. There was also a study reporting the number of fatal exertional heat stroke (EHS) incidents reported to the Japan Sport Council that occurred during organized high-school sports between 2009 and 2018 [Citation108]. This study found that 22.2% (n = 14/63) of fatalities were due to EHS; these occurred during the summer months (June–Sept), and were most prevalent when double training sessions were conducted in 1 d [Citation108]. Experts are now suggesting that a period of ≥14 consecutive days should be implemented to the fall preseason training/practice period for all secondary school athletes to mitigate any risk of exertional heat illness, and should include sport-specific and athlete-specific recommendations based on heat acclimatization guidelines [Citation109].
Maintaining fitness amid varied environmental challenges
In 2014, the Intergovernmental Panel on Climate Change (IPCC) stated that for “the immediate future, accelerating public health and medical interventions to reduce the present burden of disease … is the single most important step that can be taken to reduce the health impacts of climate change” [Citation72], with the latest report indicating that the number of deaths and people at risk of heat stress in Europe will increase two- to threefold at global warming levels of 3°C compared to 1.5°C [Citation1]. As we know, climate change will severely affect all aspects of human life in both direct and indirect ways [Citation8]. The extraordinary impact the COVID-19 pandemic has had on human movement restrictions will not be a one-off situation. From the earliest days of this COVID-19 pandemic, researchers have been sounding the alarm on how the negative impacts of isolation, cconfinement,and physical (in)activity will affect all persons [Citation10], and children in particular [Citation110]. Problematically, most governments remained either unaware or unconcerned about the effects that self-confinement would have on the physical and mental health of its citizens [Citation13]. Even for the Republic of Slovenia, which has some of the most fit and active children in the world [Citation111,Citation112], the grave costs that self-isolation measures have had on children’s physical fitness was stark, with the “SLOfit” research group observing the greatest decrease in child fitness in its >30-y history [Citation13] of conducting child fitness surveillance on the national level.
Maintaining physical fitness throughout the lifespan requires pro-active steps to promote a healthy (i.e. survival) lifestyle. In terms of heat stress, we know that adequate supply of blood flow to the heart and brain is critical to maintaining an upright posture; work capacity and cognitive function; and continuous, repeated, and/or prolonged exposure to elevated temperature imposes additional circulatory demands, both at rest and during exercise [Citation113]. Cerebral blood flow and its regulation are improved with fitness [Citation114] in both younger and older adults [Citation115] and passive heat exposure can detrimentally affect brain blood flow in adults [Citation116]. In terms of passive heat research in children, there is evidence from Finland who completed 60 min of Finnish sauna and exhibited only moderate hormonal changes to the heat, in-line with magnitudes expected from adults [Citation117]. We do not know if early-life bouts of high-heat exposure provide protective benefits to humans, as has been demonstrated in animal models [Citation118] (e.g. enhanced heat shock protein expression in battery chicks exposed to heat stress when just hatched). However, lifetime fitness trends may play a role in modifying physiological responses to heat stress, and further research is needed in this area to determine effective heat acclimation strategies in all children, especially since recent evidence in adults has found that relative reductions in energy expenditure caused by heat are significantly smaller (by up to 16%) in fit people compared to those with lower aerobic capacity [Citation119]. That aerobic fitness can itself modulate the relationship between sweat rate and body temperature (in adults) is a point of consideration when one presages how much physical strain will be required when moving in a hotter world, especially for those who may not be capable of benefitting from evaporative heat loss adaptations.
Physical activity, physical fitness, and physical literacy: Paradigm cousins to climate change resilience
According to current WHO physical activity guidelines, children and adolescents should be physically active at moderate to vigorous intensities (MVPA) for an average of at least 60 min ∙ d−1 [Citation120]. Physical activity can be defined as any dynamic state of being during which bodily movement is produced by the skeletal muscles and results in energy expenditure greater than that observed during hibernation alone [Citation121]. Research continues to demonstrate that participating in regular physical activity is indispensable to maintaining health and fitness across the lifespan, although global trends in child physical activity report consistent and rapid declines in this metric [Citation122], especially over the past 30 y [Citation123]. These include secular trends reporting physical fitness data for 25,000,000–50,000,000 children and adolescents (aged 6–19 y, from 27 countries, 1958–2003) during which cardiorespiratory endurance declined by −0.36% per year[Citation124]. Whether the physical activity “dose” suggested in these updated guidelines corresponds to attaining adequate health benefits are not currently known [Citation125], but the amount one engages in physical activity is not the only factor to consider when the aim is to minimize morbidity across the lifespan. As global warming affects weather patterns in terms of overall increasing temperatures, precipitation change, and other phenomena, there may be less children playing outside as a result, further exacerbating the inactivity issue.
Contrary to physical activity, sedentary time (and especially screen time) is associated with negative health outcomes [Citation126], with screen time guidelines suggesting a maximum of 1 h ∙ d−1 for children 5 and under, and older children are actively encouraged to limit their use of electronic devices and other recreational screen time to up to 2 h ∙ d−1 [Citation120], including (especially) avoiding screens before bedtime. Attaining enough sleep is also necessary for maintaining healthy child development, which should range between 8 and 12 h of sleep per night [Citation127]. Together, these three movement behaviors (i.e. physical activity, sedentary behavior, and sleep) have been termed “24-hour movement behavior” (24-HMB), a relatively new paradigm, by which Canada was the first nation to release 24-HMB guidelines for children and youth [Citation128]. Although there have been concerted efforts to push for unified strategies of determining global physical activity levels in children and youth [Citation129,Citation130], specific goals for maintaining overall health are not well established, and declining global patterns of daily physical activity indicate the vast majority of children and youth are not meeting WHO recommendations [Citation122]. Physical activity is notoriously difficult to quantify, especially at a population level, and these methodological challenges have been well examined elsewhere (see reviews: Refs [Citation126,Citation131]). This review will only emphasize that when discussing how much physical activity children partake in, there are many influences to consider. One group who has attempted to create a harmonized process and a standardized grading framework is an international consortium called the “Global Matrix.” First published in 2014 [Citation129], the Global Matrix systematically identified nine original key indicators (with corresponding benchmarks to consider) when grading how active children are. These original indicators include Organized Sport Participation, Active Play, Active Transportation, Sedentary Behavior, Family and Peers, Schools, Community and Built Environment, Government, and Overall Physical Activity. There have been three generations of reports published (2014, 2016, 2018) which take a global perspective in attempting to determine children’s physical activity in their day-to-day life (see Refs [Citation129,Citation130,Citation132]) with a fourth-generation report forthcoming (~November 2022). The key point to consider regarding childhood physical activity is that it is dynamic, difficult to quantify, and daily participation rates are falling (precipitously) globally.
Physical fitness is another powerful health marker for all ages. From the 1960s to ~2017, there have been global declines observed in childhood functional explosive lower-body strength[Citation133] and cardiorespiratory fitness [Citation134], including more recent declines in sit-up performance [Citation135] (from 2010 to 2017), although handgrip strength has increased moderately (~19%) across several decades [Citation136]. Universal health-related cut-points for musculoskeletal strength in children have not yet been determined as data remain insufficient to this point [Citation137], but there are criterion-based health cutoff values available for a wide range of children and youth for cardiorespiratory fitness [Citation4]. Unlike the methodological issues related to accurately quantifying physical activity [Citation131], there are many robust, valid, and widely available tools for charting childhood physical fitness, especially in school settings. Monitoring fitness in schools can be an effective policy making tool since many well-educated professionals (e.g. teachers nurses, school doctors, etc.) can oversee effective and accurate fitness measurements (e.g. SLOfit [Citation138]). Having a child fitness surveillance system in place at a national level offers education and public health decision-makers an opportunity to respond quickly and effectively to real-time changes in child physical fitness trends, a critical pillar of any public health strategy. To wit, regular childhood physical fitness assessments can (1) track changes in a child’s fitness status to design appropriate, student-centered programs; (2) assess changes derived from physical activity interventions; and (3) establish cooperation with parents, doctors, and other health-care professionals to synchronize interventions for children who may be presenting with current or future health risk(s). It is important to note that fitness testing per se should never be used to “grade” a student in the school setting. The pedagogical goals of completing regular fitness testing must be clearly communicated to the children so they are aware of the testing context, and not that their performance will be “graded.” Timely testing allows for professionals to gain an understanding of the child’s educational development and health status to make informed decisions regarding education or further countermeasures to physical inactivity as required. Thus, physical fitness is a key component to any successful pedagogical toolkit, especially moving forward as external pressures to child health become ever more challenging. Physical fitness has been added to the list of physical activity indicators of the Global Matrix 4.0 generation of data, since one’s physical fitness represents in many ways, the sum physical activity and movement one completes in a habitual manner.
The final piece of this physical movement puzzle includes the term “physical literacy,” which has been defined as the “motivation, confidence, physical competence, knowledge, and understanding that individuals develop in order to maintain physical activity at an appropriate level throughout their life” [Citation139]. Like the skills of reading, writing, listening, and speaking (which each combine to form language literacy), physical literacy is comprised of several components (i.e. physical, cognitive, emotional, and social domains, ) which interact holistically to facilitate both the participation and enjoyment of physical activity throughout the lifetime [Citation140]. A child who has not yet developed optimal physical literacy will avoid physical activity whenever possible; they may have low confidence in their physical ability and will not be motivated to participate in structured physical activities [Citation139], whereas a physically literate child will move well and confidently across a range of physically challenging situations. In this way, children can “read” their physical environment, anticipate movement needs, and respond with intelligence and imagination. There is clear evidence that monitoring physical fitness in children is critical to maintaining this key health indicator [Citation141]. Higher levels of physical fitness are associated with greater physical activity [Citation142] and better academic performance [Citation143,Citation144] and certainly, fitness testing is much more than “just one more school assessment” since it helps to increase the physical literacy of both the child and their parents as well. How fit a child is now will relate to how fit and active they will become in adulthood [Citation145]. The multidimensional and interactive nature of physical fitness is what makes it a central aspect to creating lifelong healthy and sustainable daily habits. So, physical fitness is a critical component to physical literacy overall. Individuals who have high physical literacy are more attuned to how their body works, what it needs to function properly, and are better able to foster lifelong physical activity habits.
Figure 5. Physical Literacy model with a feed-forward physical domain. Physical literacy is comprised of several components which include the physical, cognitive, emotional, and social domains. Acquiring motor skills results in physical fitness; being more physically fit allows children to learn new skills more easily, creating a powerful feed-forward positive relationship that itself feeds into the physical literacy model, affecting each of the other three domains, respectively.
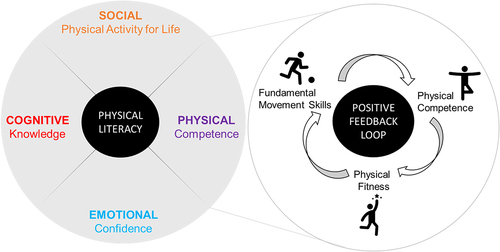
Skill and health-related fitness development are legitimate manifestations of physical literacy development, and therefore important in our understanding of this model. Physical competence is determined by one’s level of physical fitness and fundamental motor skills, which are reciprocally interconnected [Citation146,Citation147]. So, acquiring motor skills results in physical fitness, and being more physically fit will allow the child to learn new skills more easily, creating a powerful feed-forward, positive relationship (). Being adept in the Physical Competence domain enables an individual to participate in a wide range of activities over multiple contexts (e.g. on land, in water, and gliding over ice) and settings (e.g. school, household, commuting, leisure, occupation, competition). An individual who is progressing on their physical literacy journey in a positive way will be more confident moving in diverse environments effectively and in unpredictable situations. This person will have positive motivation to continue both short-term and lifelong physically active behavior. Only a person who is confident in their ability to move and learn new motor skills, will have the motivation to continue being physically active, especially as it may become more difficult to do so in their everyday life.
Maintaining adequate childhood fitness as a climate change countermeasure
Because of the recent COVID-19 movement restrictions, Europe (and the world) has been experiencing an acceleration in physical inactivity, and potentially chronic low fitness levels for its entire population, especially in its younger generation [Citation13]. Rolling movement restrictions present potentially devastating consequences to the European healthcare system, now and in the future. To counteract the escalating human cost (both financially and physically) of this ongoing crisis, there must be concerted efforts to creating, promoting, and demanding, lifelong physical activity programs [Citation110,Citation148], especially for standardized approaches to physical activity during times of pandemic self-isolation. These programs can also be used to establish physical fitness monitoring systems as a means of both assessing the scale of the physical inactivity problem, in addition to evaluating the effectiveness of any adopted policies or action plans enacted by national or EU governments. In this way, creating strong public health policies that build on the foundation of attaining daily minimum levels of physical activity, through to achieving and maintaining high physical fitness, builds a strong umbrella of protection toward one’s lifelong physical literacy (). By maintaining adequate fitness, today’s generation of children will be better equipped to meet the challenges of global warming and other environmental challenges manifested in our daily lives by this changing climate. Certainly, the urgency has never been greater to establish standardized fitness surveillance in young people [Citation149], especially since most children do not currently meet 24-HMB guidelines [Citation122], and physical inactivity is more likely to occur when daily maximum temperatures are high [Citation150].
Figure 6. Integrated model of physical activity, fitness, and literacy within the 24-hour movement behavior and climate change context. Maintaining adequate physical activity ensures there is a foundational groundwork of physical readiness which will be necessary to produce basic resistance and mitigation against degrading 24-hour movement behaviors brought on by the direct or indirect factors associated with climate change, some of which include direct warming, novel disease vectors, wildfire, air pollution, increased aeroallergens, and more. Overall physical activity is comprised of any bodily movement that may occur when doing active behaviors like organized sport, spontaneous play, or active transport, and can also be heavily impacted by sources of influence like school curricula, community infrastructure, and government policies. Maintaining high physical fitness in both health-related and skills-related fitness domains is a key tool for unlocking the habit of lifelong physical literacy, enabling young ones to better understand how their body works and fosters adaptation to movement challenges as they learn and grow.
What we know
Climate change will not only exert direct effects like higher ambient temperatures in many regions but it will also be responsible for indirect effects that can independently affect child physical activity habits [Citation33], for example as observed during the COVID-19 global pandemic [Citation13]
Prepubescent children thermoregulate differently than fully mature adults [Citation24], and this may affect their ability to offload heat under certain environmental conditions[Citation21]
There are more emergency room admissions of younger children when ambient temperatures are highe r[Citation85]
Children in the past have exhibited lower drive to drink, possibly placing them at increased risk for voluntary dehydration [Citation101], although grape flavor increases fluid intake, based on previous research [Citation92]
Adults who are tasked with caring for children do not always know (or remember) signs and symptoms of heat illness [Citation28]
Aerobic fitness is declining [Citation6], and fat stores are increasing [Citation7] in young people globally
Only ~10% of preschoolers, children, and adolescents from Europe are currently meeting 24-HMB recommendations [Citation122]
Possible future research foci
Investigations into prepubertal responses to exercise in hot conditions could aim to focus on the following areas of interest:
1. To revisit current assessments of thermal strain in children (e.g. skin temperature weighting and statistical methods) when determining child–adult comparisons to heat stress + exercise load
2. To compare different heat mode(s) and their direct effect on indices of heat acclimation (i.e. passive versus active heating on core and skin temperature, sweat rate, exercise capacity, perceived exertion, and temperature perceptions in both boys and girls).
3. To determine whether children produce greater thermo-protective and/or behavioural responses to a given heat stress compared to adults (e.g. heat shock proteins, reduced cardiovascular strain, augmented brain blood flow). If so, identify which heat mode could be most effective at eliciting these adaptations.
4. To determine whether previous heat acclimation bestows carry-over benefits for children when re-exposed to high temperatures, including behavioural factors e.g. thermal perceptions relative to thermal strain, and therefore, whether longer-term effects help build thermal resilience in children.
5. To determine to what extent cross-adaptation or maladaptation occurs when children are (or have been) physically isolated due to pandemic mitigation measures, and whether these measures place them at greater risk for poorer heat tolerance by virtue of attenuated fitness.
6. To establish whether highly fit children perform better (physically) in hot conditions compared to unfit children, especially in terms of this modern generation (i.e. establish the repeatability of landmark studies performed ~15–30 y ago)
Conclusions
Maintaining adequate physical fitness during childhood based on repetitive, daily physical activity will foster greater physical literacy skills that will be imperative to a child’s health outcomes as climate change affects our environment in substantive and long-term ways. Fit people are better able to tolerate higher temperatures, through a combination of physiologic, behavioral, and psychological factors. Young children thermoregulate differently than adults, and although there exists an excellent array of foundational studies in the field of pediatric thermoregulation, there are still many avenues to be explored. Building resiliency to maintain healthy 24-h movement behaviors in young people should be prioritized in research and policy as we adapt to an ever-changing world.
List of abbreviations
| BF | = | Blood flow |
| CVP | = | Central venous pressure |
| CO | = | Cardiac output |
| EHS | = | Exertional heat stroke |
| IPCC | = | Intergovernmental Panel on Climate Change |
| ISO | = | International Standard Organization |
| MVPA | = | Moderate-to-vigorous physical activity |
| PA | = | Physical activity |
| PBV | = | Peripheral blood volume |
| PF | = | Physical fitness |
| PL | = | Physical literacy |
| TBV | = | Total blood volume |
| Tc | = | Core temperature |
| = | Mean skin temperature | |
| UTCI | = | Universal Thermal Climate Index |
| V | = | Volume |
| WBGT | = | Wet Bulb Globe Temperature |
| WHO | = | World Health Organization |
| 24-HMB | = | 24-hour movement behavior |
Acknowledgments
The author would like to thank the ongoing support of her colleagues from the Faculty of Sport, University of Ljubljana, and the many thermal physiologists from around the world who have engaged in open, stimulating conversations on the timely topics presented in this paper.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Shawnda A. Morrison
Dr Shawnda Morrison is an environmental exercise physiologist, originally from Canada, who completed her bachelor’s and master’s degrees at the University of New Brunswick (Canada), doctoral work at the University of Otago (New Zealand), and a postdoctoral fellowship from the University of Waterloo (Canada). Shawnda’s expertise lies in adaptive and integrative human physiology in extreme environments. During her >20-y tenure as an exercise scientist, Shawnda has managed complex, multinational bedrest studies for the Canadian and European Space Agencies which looked at the combined effects of physical inactivity, hypoxia, and artificial gravity on human vascular structure and function, sleep, behavioral thermoregulation, and other multi-system effects. Shawnda holds industry gold-standard certifications as a Certified Clinical Exercise Physiologist (since 2001) and Somnologist, Expert in Sleep Medicine (since 2014). More recently, she has been the Report Card Leader for the Republic of Slovenia on the Active Healthy Kids Global Alliance Global Matrix initiative and founder of Active Healthy Kids Slovenia (est. 2015).
References
- IPCC, 2022: Climate change 2022: summary for policymakers. Impacts, adaptation, and vulnerability. contribution of working group ii to the sixth assessment report of the intergovernmental panel on climate change. Geneva
- International Health C. Constitution of the World Health Organization. 1946. Bull World Health Organ 2002; 80(12): 983–984.
- Copernicus Climate Change Service. Another exceptional month for global average temperatures. 2019. Accessed 18 March 2021. https://climate.copernicus.eu/another-exceptionalmonth-global-average-temperatures
- Ruiz J, Cavero-Redondo I, Ortega F, et al. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br J Sports Med. 2016;50(23):1451–1458.
- Tomkinson G, Carver K, Atkinson F, et al. European normative values for physical fitness in children and adolescents aged 9-17 years: results from 2 779 165 Eurofit performances representing 30 countries. Br J Sports Med. 2018;52(22):1445–14563. DOI:10.1136/bjsports-2017-098253.
- Tomkinson G, Léger L, Olds T, et al. Secular trends in the performance of children and adolescents (1980-2000): an analysis of 55 studies of the 20m shuttle run test in 11 countries. Sports Med. 2003;33(4):285–300.
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. NCD-RisC. DOI:10.1016/S0140-6736(17)32129-3.
- Helldén D, Andersson C, Nilsson M, et al. Climate change and child health: a scoping review and an expanded conceptual framework. Lancet Public Health. 2021;5(3):e164–e75.
- Anderko L, Chalupka S, Du M, et al. Climate changes reproductive and children’s health: a review of risks, exposures, and impacts. Pediatr Res. 2020;87(2):414–419.
- Burtscher J, Burtscher M, Millet GP. Indoor) isolation, stress and physical inactivity: vicious circles accelerated by Covid-19? Scand J Med Sci Sports. 2020;30(8):1544–1545.
- Daanen H, Bose-O’Reilly S, Brearley M, et al. COVID-19 and thermoregulation-related problems: practical recommendations. Temperature. 2020;8(1):1–11. DOI:10.1080/23328940.2020.1790971.
- Buoite Stella A, Filingeri D, Ravanelli N, et al. Heat risk exacerbation potential for neurology patients during the COVID-19 pandemic and related isolation. Int J Biometeorol. 2021;65(4):627–630. DOI:10.1007/s00484-020-02044-2.
- Jurak G, Morrison SA, Kovač M, et al. A COVID-19 crisis in child physical fitness: creating a barometric tool of public health engagement for the republic of Slovenia. Front Public Health. 2021;9(179). DOI:10.3389/fpubh.2021.644235.
- Pavy-Le Traon A, Heer M, Narici M, et al. From space to Earth: advances in human physiology from 20 years of bedrest studies (1986-2006). Eur J Appl Physiol. 2007;101(2):143–194.
- Narici M, De Vito G, Franchi M, et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur J Sport Sci. 2020:1–22.
- Ahdoot S, Pacheco S, Paulson JA. Global climate change and children’s health. Pediatrics. 2015;136(5):e1468–84.
- Pegram J, Colon C. Are climate change policies child-sensitive? New York: United Nations Children’s Fund (UNICEF; 2019.
- Casanueva A, Kotlarski S, Fischer AM, et al. Escalating environmental summer heat exposure—a future threat for the European workforce. Reg Environ Change. 2020;20(2):40. DOI:10.1007/s10113-020-01625-6.
- Vanos J, Baldwin J, Jay O, et al. Simplicity lacks robustness when projecting heat-health outcomes in a changing climate. Nat Commun. 2020;11(1):6079.
- Zisis E, Hakimi S, Lee EY. Climate change, 24-hour movement behaviors, and health: a mini umbrella review. Glob Health Res Policy. 2021;6(1):15.
- Notley SR, Akerman AP, Meade RD, et al. Exercise thermoregulation in prepubertal children: a brief methodological review. Med Sci Sports Exerc. 2020;52(11):2412–2422.
- Falk B, Dotan R. Temperature regulation and elite young athletes. Med Sport Sci. 2011;56:126–149.
- Falk B, Dotan R. Children’s thermoregulation during exercise in the heat: a revisit. Appl Physiol Nutr Metab. 2008;33(2):420–427.
- Smith CJ. Pediatric thermoregulation: considerations in the face of global climate change. Nutrients. 2019;11(9):2010.
- McGarr GW, Saci S, King KE, et al. Heat strain in children during unstructured outdoor physical activity in a continental summer climate. Temperature. 2020;8(1):80–89. DOI:10.1080/23328940.2020.1801120.
- Tyler CJ, Reeve T, Hodges GJ, et al. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Med. 2016;46(11):1699–1724.
- Periard JD, Eijsvogels TMH, Daanen HAM. Exercise under heat stress: thermoregulation, hydration, performance implications and mitigation strategies. Physiol Rev. 2021;101(4):1873–1979.
- Folkerts MA, Gerrett N, Kingma BRM, et al. Care provider assessment of thermal state of children in day-care centers. Build Environ. 2020;179:106915.
- Morrison SA, Sims ST. Thermoregulation in children: exercise, heat stress & fluid balance. Annales Kinesiologiae. 2014;5(1):41–55.
- Hebestreit H, Bar-Or O, McKinty C, et al. Climate-related corrections for improved estimation of energy expenditure from heart rate in children. J Appl Physiol (1985). 1995;79(1):47–54.
- Hebestreit H, Bar-Or O. Influence of climate on heart rate in children: comparison between intermittent and continuous exercise. Eur J Appl Physiol. 1998;78(1):7–12.
- McMichael AJ. Climate change and human health. Geneva: World Health Organisation; 1996.
- Watts N, Amann M, Arnell N, et al. The 2019 report of the Lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836–1878. DOI:10.1016/S0140-6736(19)32596-6.
- Morrison SA, Périard JD, De Boever P. Daanen HAM. editorial: the effects of climate change and environmental factors on exercising children and youth from sports act living. Frontiers in Sports and Active Living. 2021; May 28; 3:690171.10.3389/fspor.2021.690171
- Gisolfi CV Exercise and Thermoregulation. In: Sutton JR, Thompson MW, Torode ME, editors. 10th Biennial Conference, Sydney, Australia; 1995; University of Sydney; p. 63–74.
- Morrison S, Sleivert GG, Cheung SS. Passive hyperthermia reduces voluntary activation and isometric force production. Eur J Appl Physiol. 2004;91(5–6):729–736.
- Nybo L, Nielsen B. Hyperthermia and central fatigue during prolonged exercise in humans. J Appl Physiol. 2001;91(3):1055–1060.
- Gagge AP, Gonzalez RR. Mechanisms of heat exchange: biophysics and physiology. In: Fregly MJ, Blatteis CM, editors. Handbook of physiology: environmental physiology. New York: Oxford University Press; 1996. p. 45–84.
- Nielsen B, Kassow K, Aschengreen F,E. Heat balance during exercise in the sun. Eur J Appl Physiol. 1988;58(1–2):189–196.
- Piil JF, Christiansen L, Morris NB, et al. Direct exposure of the head to solar heat radiation impairs motor-cognitive performance. Sci Rep. 2020;10(1):7812. DOI:10.1038/s41598-020-64768-w.
- Asmussen E, Boje O. Body temperature and capacity for work. Acta Physiol Scand. 1945;10(1):1–22.
- Bradford CD, Cotter JD, Thorburn MS, et al. Exercise can be pyrogenic in humans. Am J Physiol Regu Integr Com Physiol. 2007;292(1):R143–R9.
- Morris NB, English T, Hospers L, et al. The effects of electric fan use under differing resting heat index conditions: a clinical trial. Ann Intern Med. 2019;171(9):675–677.
- Morrison SA, Cheung S, Cotter JD. Importance of airflow for physiologic and ergogenic effects of precooling. J Athl Train. 2014;49(5):632–639.
- Burton AC. The average temperature of the tissues of the body. Nutr J. 1935;9(3):261–280.
- Jay O, Reardon FD, Webb P, et al. Estimating changes in mean body temperature for humans during exercise using core and skin temperatures is inaccurate even with a correction factor. J Appl Physiol. 2007;103(2):443–451. DOI:10.1152/japplphysiol.00117.2007.
- DuBois D, DuBois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med. 1916;17(6_2):863–871.
- Ramanathan NL. A new weighting system for mean surface temperature of the human body. J Appl Physiol. 1964;19(3):531–533.
- Liu W, Lian Z, Deng Q, et al. Evaluation of calculation methods of mean skin temperature for use in thermal comfort study. Build Environ. 2011;46(2):478–488.
- Nielsen R, Nielsen B. Measurement of mean skin temperature of clothed persons in cool environments. Eur J Appl Physiol. 1984;53(3):231–236.
- ISO. Evaluation of thermal strain by physiological measurements. International Organization for Standardization; 9886:2004Geneva, Switzerland.
- Olesen S, Bassing J, Fanger P. Physiological comfort conditions at sixteen combinations of activity, clothing, air velocity and ambient temperature. ASHRAE Trans. 1972;78:199–206.
- Haycock GB, Schwartz GJ, Wisotsky DH. Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr. 1978;93(1):62–66.
- Romanovsky AA. Skin temperature: its role in thermoregulation. Acta Physiol. 2014;210(3):498–507.
- Nakamura M, Yoda T, Crawshaw LI, et al. Regional differences in temperature sensation and thermal comfort in humans. J Appl Physiol (1985). 2008;105(6):1897–1906. DOI:10.1152/japplphysiol.90466.2008.
- Nakamura M, Yoda T, Crawshaw LI, et al. Relative importance of different surface regions for thermal comfort in humans. Eur J Appl Physiol. 2013;113(1):63–76. DOI:10.1007/s00421-012-2406-9.
- Haldane JS. The influence of high air temperatures: no. 1. Am J Hyg. 1905;5(4):494–513.
- Budd GM. Wet-bulb globe temperature (WBGT)–its history and its limitations. J Sci Med Sport. 2008;11(1):20–32.
- Yaglou CP, Minard D. Control of heat casualties at military training centers. AMA Arch Ind Health. 1957;16(4):302–316.
- Organisation IS. Hot environments – estimation of the heat stress on working man, based on the WBGT-index (wet bulb globe temperature). Geneva: International Organization for Standardization; 1989.
- Armstrong LE, Casa DJ, Millard-Stafford M, et al. American college of sports medicine position stand. exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572.
- Liljegren JC, Carhart RA, Lawday P, et al. Modeling the wet bulb globe temperature using standard meteorological measurements. J Occup Environ Hyg. 2008;5(10):645–655.
- Błażejczyk K, Jendritzky G, and Bröde P, et al. An introduction to the universal thermal climate index (UTCI). Geographia Polonical. 2013;86(5–10).
- Jendritzky G, de Dear R, Havenith G. UTCI–why another thermal index? Int J Biometeorol. 2012;56(3):421–428.
- Foster J, Smallcombe JW, Hodder S, et al. An advanced empirical model for quantifying the impact of heat and climate change on human physical work capacity. Int J Biometeorol. 2021;65(7):1215–1229. DOI:10.1007/s00484-021-02105-0.
- Arlegui L, Smallcombe JW, Fournet D, et al. Body mapping of sweating patterns of pre-pubertal children during intermittent exercise in a warm environment. Eur J Appl Physiol. 2021;121(12):3561–3576.
- Rowell LB. Human cardiovascular adjustments to exercise and thermal stress. Physiol Rev. 1974;54(1):75–159.
- Rowland T, Hagenbuch S, Pober D, et al. Exercise tolerance and thermoregulatory responses during cycling in boys and men. Med Sci Sports Exerc. 2008;40(2):282–287.
- Brengelmann GL, Johnson JM, Hermansen L, et al. Altered control of skin blood flow during exercise at high internal temperatures. J Appl Physiol Respir Environ Exerc Physiol. 1977;43(5):790–794.
- Falk B. Effects of thermal stress during rest and exercise in the paediatric population. Sports Med. 1998;25(4):221–240.
- WHO. Quantitative risk assessment of the effects of climate change on selected causes of death 2030s and 2050s. Geneva: World Health Organisation; 2014.
- IPCC. Human health: impacts, adaptation and co-benefits, chapt 11, WGII, AR5. Geneva: Inter-Governmental Panel on Climate Change; 2014.
- Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. Lancet. 2021;398(10301):698–708. DOI:10.1016/S0140-6736(21)01208-3.
- Hospers L, Cheuvront SN, Kenefick RW, et al. Independent influence of skin temperature on whole-body sweat rate. Med Sci Sports Exerc. 2020;52(11):2423–2429.
- Ioannou LG, Tsoutsoubi L, Samoutis G, et al. Time-motion analysis as a novel approach for evaluating the impact of environmental heat exposure on labor loss in agriculture workers. Temperature. 2017;4(3):330–340. DOI:10.1080/23328940.2017.1338210.
- Morris NB, Piil JF, Morabito M, et al. The HEAT-SHIELD project - Perspectives from an inter-sectoral approach to occupational heat stress. J Sci Med Sport. 2021;24(8):747–755. DOI:10.1016/j.jsams.2021.03.001.
- Piil JF, Lundbye-Jensen J, Trangmar SJ, et al. Performance in complex motor tasks deteriorates in hyperthermic humans. Temperature. 2017;4(4):420–428. DOI:10.1080/23328940.2017.1368877.
- Rowell LB, Brengelmann GL, Murray JA. Cardiovascular responses to sustained high skin temperature in resting man. J Appl Physiol. 1969;27(5):673–680.
- Rowell LB. Cardiovascular aspects of thermoregulation. Circ Res. 1983;52(4):367–379.
- Laitano O, Murray KO, Leon LR. Overlapping mechanisms of exertional heat stroke and malignant hyperthermia: evidence vs conjecture. Sports Med. 2020;50(9):1581–1592.
- Wilson TE, Tollund C, Yoshiga CC, et al. Effects of heat and cold stress on central vascular pressure relationships during orthostasis in humans. J Physiol. 2007;585(1):279–285. DOI:10.1113/jphysiol.2007.137901.
- Nelson MD, Haykowsky MJ, Petersen SR, et al. Increased left ventricular twist, untwisting rates, and suction maintain global diastolic function during passive heat stress in humans. Am J Physiol Heart Circ Physiol. 2010;298(3):H930–7.
- Lang J, Tremblay M, Léger L, et al. International variability in 20 m shuttle run performance in children and youth: who are the fittest from a 50-country comparison? A systematic literature review with pooling of aggregate results. Br J Sports Med. 2018;52(4):276.
- Somboonwong J, Sanguanrungsirikul S, Pitayanon C. Heat illness surveillance in schoolboys participating in physical education class in tropical climate: an analytical prospective descriptive study. BMJ Open. 2012;2(4):e000741.
- Bernstein AS, Sun S, Weinberger KR, et al. Warm season and emergency department visits to U.S. children’s hospitals. Environ Health Perspect. 2022;130(1):17001.
- Sun S, Weinberger KR, Nori-Sarma A, et al. Ambient heat and risks of emergency department visits among adults in the United States: time stratified case crossover study. BMJ (Clin Res Ed). 2021;375:e065653.
- Ravanelli N, Gagnon D, Imbeault P, et al. A retrospective analysis to determine if exercise training-induced thermoregulatory adaptations are mediated by increased fitness or heat acclimation. Exp Physiol. 2021;106(1):282–289.
- Roberts MF, Wenger CB. Control of skin circulation during exercise and heat stress. Med Sci Sport Exer. 1979;11:36–41.
- McLellan TM. The importance of aerobic fitness in determining tolerance to uncompensable heat stress. Comp Biochem Physiol Part A Mol Integr. 2001;128(4):691–700.
- Tikuisis P, McLellan TM, Selkirk G. Perceptual versus physiological heat strain during exercise-heat stress. Med Sci Sport Exercise. 2002;34(9):1454–1461.
- Mekjavic IB, Eiken O. Contribution of thermal and nonthermal factors to the regulation of body temperature in humans. J Appl Physiol (1985). 2006;100(6):2065–2072.
- Wilk B, Bar-Or O. Effect of drink flavor and NaCL on voluntary drinking and hydration in boys exercising in the heat. J Appl Physiol (1985). 1996;80(4):1112–1117.
- Daanen HA, Jonkman AG, Layden JD, et al. Optimising the acquisition and retention of heat acclimation. Int J Sports Med. 2011;32(11):822–828.
- Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25(1):20–38.
- Alhadad SB, Tan PMS, Lee JKW. Efficacy of heat mitigation strategies on core temperature and endurance exercise: a meta-analysis. Front Physiol. 2019;10:71.
- Lee JKW, Nio AQX, Fun DCY, et al. Effects of heat acclimatisation on work tolerance and thermoregulation in trained tropical natives. J Therm Biol. 2012;37(5):366–373.
- Maloyan A, Palmon A, Horowitz M. Heat acclimation increases the basal HSP72 level and alters its production dynamics during heat stress. Am J Physiol. 1999;276(5):R1506–15.
- Maloyan A, Eli-Berchoer L, Semenza GL, et al. HIF-1alpha-targeted pathways are activated by heat acclimation and contribute to acclimation-ischemic cross-tolerance in the heart. Physiol Genomics. 2005;23(1):79–88.
- Meyer F, Bar-Or O. Fluid and electrolyte loss during exercise. The paediatric angle. Sports Med. 1994;18(1):4–9.
- Meyer F, Bar-Or O, Salsberg A, et al. Hypohydration during exercise in children: effect on thirst, drink preferences, and rehydration. Int J Sport Nutr. 1994;4(1):22–35.
- Bar-Or O, Dotan R, Inbar O, et al. Voluntary hypohydration in 10- to 12-year-old boys. J Appl Physiol Respir Environ Exerc Physiol. 1980;48(1):104–108.
- Schlader Z. The relative overlooking of human behavioral temperature regulation: an issue worth resolving. Temperature. 2014;1(1):20–21. doi:10.4161/temp.29235.
- Scarneo-Miller SE, Saltzman B, and Adams WM, et al. Regional requirements influence adoption of exertional heat illness preparedness strategies in United States high schools. Medicina (Kaunas). 2020;56(10): 488.
- Adams WM, Mazerolle SM, Casa DJ, et al. The secondary school football coach’s relationship with the athletic trainer and perspectives on exertional heat stroke. J Athl Train. 2014;49(4):469–477.
- Misailidi M, Mantzios K, Papakonstantinou C, et al. Environmental and psychophysical heat stress in adolescent tennis athletes. Int J Sports Physiol Perform. 2021;16(12):1895–1900.
- Périard JD, Racinais S, Knez WL, et al. Thermal, physiological and perceptual strain mediate alterations in match-play tennis under heat stress. Br J Sports Med. 2014;48 1(1):i32–i8.
- Bergeron MF, McLeod KS, Coyle JF. Core body temperature during competition in the heat: national boys’ 14s junior championships. Br J Sports Med. 2007;41(11):779–783.
- Yamanaka MS, Hosokawa Y, Ayusawa M, et al. Epidemiology of sports-related fatalities during organized school sports in Japanese high schools between 2009 and 2018. PLoS One. 2021;16(8):e0256383.
- Adams WM, Hosokawa Y, Casa DJ, et al. Roundtable on preseason heat safety in secondary school athletics: heat acclimatization. J Athl Train. 2021;56(4):352–361. DOI:10.4085/1062-6050-596-20.
- Morrison SA, Jurak G, Starc G. Responding to a global pandemic: Republic of Slovenia on maintaining physical activity during self-isolation. Scand J Med Sci Sports. 2020;30(8):1546–1548.
- Morrison SA, Sember V, Leskošek B, et al. Assessment of secular trends and health risk in pediatric cardiorespiratory fitness from the republic of slovenia. Front Physiol. 2021;12:644781.
- Aubert S, Barnes JD, Aguilar-Farias N, et al. Report Card grades on the physical activity of children and youth comparing 30 very high human development index countries. J Phys Act Health. 2018;15(S2):S298–S314. DOI:10.1123/jpah.2018-0431.
- Rowell LB. Human cardiovascular control. New York: Oxford University Press; 1993.
- Ainslie PN, Cotter JD, George KP, et al. Elevation in cerebral blood flow velocity with aerobic fitness throughout healthy human ageing. J Physiol. 2008;586(16):4005–4010. DOI:10.1113/jphysiol.2008.158279.
- Bailey DM, Marley CJ, Brugniaux JV, et al. Elevated aerobic fitness sustained throughout the adult lifespan is associated with improved cerebral hemodynamics. Stroke. 2013;44(11):3235–3238. DOI:10.1161/STROKEAHA.113.002589.
- Gibbons T, Ainslie P, Thomas K, et al. Influence of the mode of heating on cerebral blood flow, non-invasive intracranial pressure and thermal tolerance in humans. J Physiol. 2021;599(7):1977–1996. DOI:10.1113/JP280970.
- Jokinen E, Välimäki I, Marniemi J, et al. Children in sauna: hormonal adjustments to intensive short thermal stress. Acta Physiol Scand. 1991;142(3):437–442.
- Goel A, Ncho CM, Choi YH. Regulation of gene expression in chickens by heat stress. J Anim Sci Biotechnol. 2021;12(1):11.
- Foster J, Smallcombe JW, Hodder SG, et al. Aerobic fitness as a parameter of importance for labour loss in the heat. J Sci Med Sport. 2021;24(8):824–830. DOI:10.1016/j.jsams.2021.05.002.
- WHO Guidelines on Physical Activity and Sedentary Behaviour. Geneva: World Health Organisation; 2020.p. 25.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. 433021. 1985;100(2):126–131. Washington, DC: 1974.
- Tapia-Serrano MA, Sevil-Serrano J, Sánchez-Miguel PA, et al. Prevalence of meeting 24-hour movement guidelines from pre-school to adolescence: a systematic review and meta-analysis including 387,437 participants and 23 countries. J Sport Health Sci. 2022. DOI:10.1016/j.jshs.2022.01.005
- Fühner T, Kliegl R, Arntz F, et al. An update on secular trends in physical fitness of children and adolescents from 1972 to 2015: a systematic review. Sports Med. 2021;51(2):303–320.
- Tomkinson GR, Olds TS. Secular changes in pediatric aerobic fitness test performance: the global picture. Med Sports Sci. 2007;50:46–66.
- Khan A, Lee EY, Rosenbaum S, et al. Dose-dependent and joint associations between screen time, physical activity, and mental wellbeing in adolescents: an international observational study. Lancet Child Adolesc Health. 2021;5(10):729–738.
- Poitras VJ, Gray CE, Borghese MM, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S197–239. DOI:10.1139/apnm-2015-0663.
- Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–58.
- Tremblay M, Carson V, Chaput J, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Met. 2016;41(6):S311–S27. DOI:10.1139/apnm-2016-0151.
- Tremblay MS, Gray CE, Akinroye K, et al. Physical activity of children: a global matrix of grades comparing 15 countries. J Phys Act Health. 2014;11(s1):S113–25. DOI:10.1123/jpah.11.s1.s113.
- Aubert S, Barnes JD, Abdeta C, et al. Global matrix 3.0 physical activity report card grades for children and youth: results and analysis from 49 countries. J Phys Act Health. 2018;15(S2):S251–S73. DOI:10.1123/jpah.2018-0472.
- Adamo KB, Prince SA, Tricco AC, et al. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: a systematic review. Int J Pediatr Obes. 2009;4(1):2–27.
- Tremblay MS, Barnes JD, González SA, et al. Global matrix 2.0: report card grades on the physical activity of children and youth comparing 38 countries. J Phys Act Health. 2016;13(11):S343–s66. DOI:10.1123/jpah.2016-0594.
- Tomkinson GR, Kaster T, Dooley FL, et al. Temporal trends in the standing broad jump performance of 10,940,801 children and adolescents between 1960 and 2017. Sports Med. 2021;51(3):531–548. DOI:10.1007/s40279-020-01394-6.
- Tomkinson G, Lang J, Tremblay M. Temporal trends in the cardiorespiratory fitness of children and adolescents representing 19 high-income and upper middle-income countries between 1981 and 2014. Br J Sports Med. 2019;53(8):478–486.
- Kaster T, Dooley F, Fitzgerald J, et al. Temporal trends in the sit-ups performance of 9,939,289 children and adolescents between 1964 and 2017. J Sports Sci. 2020;38(16):1913–1923. DOI:10.1080/02640414.2020.1763764.
- Dooley FL, Kaster T, Fitzgerald JS, et al. A systematic analysis of temporal trends in the handgrip strength of 2,216,320 children and adolescents between 1967 and 2017. Sports Med. 2020;50(6):1129–1144. DOI:10.1007/s40279-020-01265-0.
- Fraser B, Rollo S, Sampson M, et al. Health-related criterion-referenced cut-points for musculoskeletal fitness among youth: a systematic review. Sports Med. 2021;51(12):2629–2646. DOI:10.1007/s40279-021-01524-8.
- Jurak G, Leskošek B, Kovac M, et al. SLOfit surveillance system of somatic and motor development of children and adolescents: upgrading the Slovenian sports educational chart. Kinanthropologica. 2020;56(1):28–40. DOI:10.14712/23366052.2020.4.
- Whitehead M. The concept of physical literacy. Eur J Phys Educ. 2001;6(2):127–138.
- Longmuir PE, Gunnell KE, Barnes JD, et al. Canadian assessment of physical literacy second edition: a streamlined assessment of the capacity for physical activity among children 8 to 12 years of age. BMC Public Health. 2018;18(2):1047. DOI:10.1186/s12889-018-5902-y.
- Cairney J, Dudley D, Kwan M, et al. Physical literacy, physical activity and health: toward an evidence-informed conceptual model. Sports Med. 2019;49(3):371–383.
- Chen W, Hammond-Bennett A, Hypnar A, et al. Health-related physical fitness and physical activity in elementary school students. BMC Public Health. 2018;18(1):195.
- Sember V, Jurak G, Starc G, et al. Can primary school mathematics performance be predicted by longitudinal changes in physical fitness and activity indicators? Front Psychol. 2022;13:796838.
- Sember V, Jurak G, Kovač M, et al. Children’s physical activity, academic performance, and cognitive functioning: a systematic review and meta-analysis. Front Public Health. 2020;8:307.
- Kvaavik E, Klepp KI, Tell GS, et al. Physical fitness and physical activity at age 13 years as predictors of cardiovascular disease risk factors at ages 15, 25, 33, and 40 years: extended follow-up of the Oslo youth study. Pediatrics. 2009;123(1):e80–6.
- Barnett LM, Van Beurden E, Morgan PJ, et al. Does childhood motor skill proficiency predict adolescent fitness? Med Sci Sports Exerc. 2008;40(12):2137–2144.
- Lubans DR, Morgan PJ, Cliff DP, et al. Fundamental movement skills in children and adolescents: review of associated health benefits. Sports Med. 2010;40(12):1019–1035.
- Jurak G, Morrison SA, Leskošek B, et al. Physical activity guidelines during the COVID-19 pandemic outbreak. J Sport Health Sci. 2020;9(4):325–327. DOI:10.1016/j.jshs.2020.05.003.
- Lang J, Tomkinson G, Janssen I, et al. Making a case for cardiorespiratory fitness surveillance among children and youth. Exerc Sport Sci Rev. 2018;46(2):66–75. DOI:10.1249/JES.0000000000000138.
- Lewis LK, Maher C, Belanger K, et al. At the mercy of the gods: associations between weather, physical activity, and sedentary time in children. Pediatr Exer Sci. 2016;28(1):152–163.
