Abstract
Aim: The purpose of the study was to assess the marginal adaptation and discrepancy of SSC’s. Differences in adaptation and discrepancy between the four surfaces (mesial, lingual, distal, and buccal) were evaluated.
Methods: The placement of stainless steel crowns were completed on a phantom head in accordance with the clinical technique. The ideal tooth preparation was made and this ‘master tooth’ duplicated to achieve a sample size of 15. The stainless steel crowns were placed, trimmed, and cemented as per the clinical technique. The cemented stainless crowns were analyzed under 100× stereomicroscope magnification. The marginal adaptation and discrepancy of each specimen was measured every 2 µm.
Results: All the specimens showed marginal adaptation and discrepancy. The lingual margin had a significantly better adaptation (p < .0001) over the other surfaces. The buccal surface was the only surface that had an appropriate supra-CEJ level with a significance of p < .0001.
Conclusion: The marginal discrepancies occur during the trimming procedure and assessment of the gingival approximation of the SSC margin. The inspection of stainless steel crown adaptation and discrepancy is an essential clinical step.
Introduction
Dental caries is one of the major oral health problems affecting children [Citation1]. If caries is left untreated, its consequences, which include pain and infection, will negatively affect the child’s health and subsequently have an effect on the family as well [Citation2]. Therefore, surgical and restorative measures are crucial to mitigating the disease process [Citation3].
Restorative treatment of carious teeth restores function, maintains the arch integrity and eliminates the progression of dental caries [Citation1]. The complexity of the restorative treatment increases when dental caries involves more than one surface of the tooth. The removal of dental caries can lead to a more extensive cavity preparation. The larger the restoration, the greater the probability of fracture [Citation4]. The extent of tooth destruction determines the ability of the clinician to re-establish a functional crown morphology with adjacent contacts [Citation5].
Failure of restorative materials is more common in primary teeth compared with permanent teeth [Citation6]. This is due to factors such as patient cooperation, primary tooth morphology, differences in tooth structure, and the type of restorative material used. For primary teeth, it has been reported that full coronal coverage increases the structural integrity of the tooth and durability of the restoration [Citation1]. Accordingly, the American Academy of Pediatric Dentistry (AAPD) recommends the use of stainless steel crowns (SSC’s) in primary teeth, especially where caries involves multiple surfaces [Citation7]. SSC’s were introduced in the 1950s. Thereafter, the recommendation followed for it to become a definitive restoration for primary molars [Citation8,Citation9]. Since then, different designs of SSC’s have been developed in an attempt to achieve greater adaptation and replication of the morphological features of the teeth. Crowns that were neither trimmed nor contoured were initially introduced but their use was limited [Citation10]. This led to the development of pre-trimmed and pre-contoured SSC’s, which have straight proximal sides [Citation11]. These SSC’s are the most commonly used. The advantage over untrimmed SSC is in that the design follows the gingival contour and tooth anatomy [Citation11,Citation12]. The longevity of the restorative treatment is one of the most important aspects of clinical dentistry. SSC’s have gained popularity with pediatric dentists due to their successful performance as a restorative material [Citation13]. SSC’s had a higher degree of wear resistance compared to other direct restorative materials such as amalgam, composite, compomer, and Resin Modified Glass Ionomer (RMGIC) [Citation14]. The longevity of the SSC’s could be extended from 5 to 15 years when adequate marginal adaptation is achieved [Citation11]. SSC’s are cost effective [Citation15] compared with other conventional restorative materials, due to their superiority in restoring multi-surface cavities in primary molars [Citation1,Citation16]. The main disadvantage is the perception of the patient that SSC’s have poor esthetics. The esthetic demand has grown significantly in recent decades for adults and children [Citation17].
With the investigation of SSC’s, there are two essential areas of concern namely, marginal adaptation and marginal discrepancy. Marginal adaptation is defined as ‘the perpendicular marginal distance from the internal surface of the restoration to the finishing line of the preparation’ [Citation18]. This is clinically significant, as any increase in the marginal gap between the tooth surface and the crown may result in dissolution of the cement, which in turn increases the risk of microleakage, recurrent caries, and periodontal disease [Citation19]. This significantly affects the longevity, retention, and the success of SSC’s [Citation20]. The marginal discrepancy describes the vertical discrepancy between the crown margin at various points and the abutment [Citation21]. Maintaining an accurate marginal fit between the tooth and the crown is essential for protecting the tooth from chemical, physical, bacterial, and thermal influence [Citation22]. The ideal extension of SSC to achieve proper retention is at the cement-enamel junction (CEJ) or slightly occlusal to it. Accordingly, unequal extension in the margin may result either in an open margin or in over-extension of the SSC margin [Citation11]. The extension of the crown margin can be assessed clinically by passing a periodontal probe around the margin [Citation22,23] and ensuring that no blanching of the gingiva is present clinically due to the impingement of the biological width by the SSC [Citation11]. Studies evaluating the periodontal health in association with SSC placement found a positive correlation between plaque index and gingivitis in SSC’s where poor marginal adaptation was reported [Citation9,Citation24–26].
The rationale of the present study was based on the paucity of studies that simultaneously focused on marginal adaptation and discrepancy. Additionally, no studies were performed on a standardized ‘ideal master tooth SSC preparation’.
The purpose of this study was to assess the marginal adaptation and discrepancy of SSC’s between the four surfaces (mesial, lingual, distal, and buccal).
Materials and methods
Design
An in vitro experimental study using 15 stainless steel crowns was conducted. The sample size justification was based on the literature, where it was found that a large number of measurements for each sample could compensate for the small sample size [Citation27]. According to this conclusion, two studies were conducted, using a small sample size (n = 10) and to overcome this small sample size, they increased the number of measurements per sample to 50 and 60 measurements [Citation28,Citation29]. This resulted in a more consistent distribution of the data with a small standard deviation compared to the mean values [Citation30].
This study was performed on a phantom head with an occluding maxillary and mandibular jaw in order to simulate the intra-oral clinical procedure. One polymethylmethacrylate second mandibular primary molar (Ivorine teeth, Colombia Dentoform Corp.) of a pediatric phantom head was selected. The rationale for this was to standardize the crown morphology between the samples. In this study, the typodont tooth was prepared for a SSC and termed ‘master tooth’.
Master tooth selection
The correlation between the remaining tooth structure and marginal adaptation is lacking in the literature. The influence of the residual tooth structure was evaluated on the retention and adaptation of the SSC. The cervical part of the tooth is the most important area for crown retention and adaptation [Citation31]. The selection of an artificial typodont tooth (polymethylmethacrylate second mandibular primary molar) resembles the sound tooth structure for the placement of a SSC. This eliminated the confounding factor of irregular tooth anatomy and caries that influence the morphology of the carious lesions.
Master tooth preparation
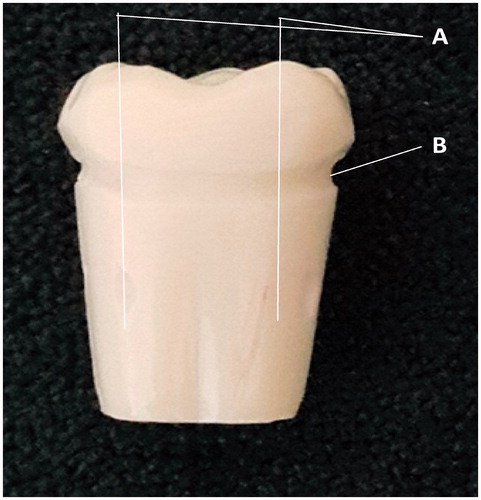
A standard SSC preparation was completed on the typodont second mandibular primary molar [Citation22]. The occlusal surface reduction by 1 mm, using an 836R bur (Modified end cylinder bur, Diatech Dental, Heerbrugg, Switzerland). illustrates the occlusal and proximal surface preparation using a diamond featheredge bur (Diatech Dental, Heerbrugg, Switzerland) to remove all mesial and distal undercuts without leaving any ledges.
The CEJ shown in is marked in the master tooth using an 836R bur to a depth and thickness of 1 mm. The marked CEJ was used as a reference line for the measurement of marginal adaptation and discrepancy.
In order to differentiate between the buccal, lingual, mesial, and distal surfaces of the tooth during the measuring of the marginal adaptation and discrepancy, a line was drawn from each cusp on the long axis of the tooth toward the apical part of the root surface, thereby separating the four surfaces. shows the four grooves were prepared using an 836R bur.
Duplication of master tooth
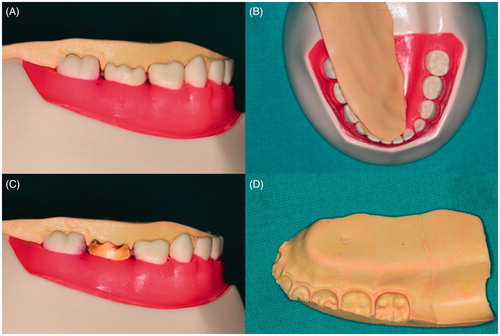
In order to standardize the shape of the 15 teeth used in the study, an additional silicone mold was made from the ‘master tooth’. The use of additional silicone increased the efficiency and accuracy of the mold. This mold was used to duplicate 15 teeth in polyester resin as shown in . Any excess resin material was removed to prevent inadequate fitting of the duplicated teeth with the assistance of an occlusal stamp as shown in .
Figure 4. (A and B) Occlusal stamp with master tooth. (C) Occlusal stamp with duplicated tooth. (D) Occlusal stamp.
The use of duplicated teeth with the same crown size for all 15 specimens provided standardization for the tooth circumference and preparation in order to reduce any variation in the measurement between all teeth.
Demarcation of the cemento-enamel junction in the duplicated teeth
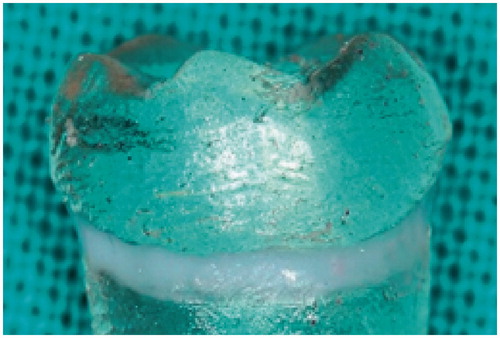
The prepared CEJ in the master tooth was re-demarcated in the duplicated teeth by filling the prepared groove with a blue gingival barrier light curing resin (SDI Limited, Bayswater, VIC, Australia) in to facilitate clearer visual identification of the CEJ margin. The gingival barrier resin was applied according to the manufacturer’s instructions. Any excess material was removed before curing, ensuring the surface was flush. A plastic instrument was used to remove the excess material, which could negatively affect marginal adaptation and discrepancy measurements. The resin was light cured for 30 s using a Demetron LC curing light (Kerr Corp, Orange, CA, USA). In the literature, as reference lines were not used on extracted teeth to simulate the CEJ and ensure clear identification, the researcher could over- or underestimate the SSC marginal adaptation/discrepancy. Clinically, this error does not readily occur, since insufficient marginal trimming results in gingival blanching until the crown has been trimmed, resulting in a SSC margin that is not overextended in the tissue. For this reason, an incorrect finishing line, which does not simulate the clinical tooth-SSC interface, could result in the altered performance of the SSC crown with in vitro studies [Citation32,Citation33].
Seating of the duplicated teeth
An occlusal stamp (shown in ) was made using president silicone impression material (vinyl polysiloxane) to record the position of the master tooth in the phantom head jaw prior to being replaced with the 15 duplicated teeth. This facilitated accurate positioning of each duplicated tooth in the phantom head jaw and ensured reproducibility ().
Selection and adjustment of stainless steel crowns
Clinically, the selection of the appropriate crown size can be done by using a divider to measure the mesio-distal dimension of the tooth itself or using the contralateral tooth if the clinical tooth crown is severely carious, making appropriate crown measurement difficult [Citation34].
In the present study, the mesio-distal width of the typodont tooth was measured in order to record the size before tooth preparation (to create the master tooth). Based on the measurement, 15 SSC’s (size E3) were selected. The crowns were trimmed and shaped according to the manufacturer’s instructions and placed on the duplicated teeth in the mandibular jaw of the phantom head. Performing the placement and adaptation of the SSC on the phantom head in this in vitro study simulated the actual clinical procedure. It was important to adjust the crown margin in relation to the primary tooth gingiva. The marginal extension and fit were assessed. The ideal extension of the crown margin is either 1-mm subgingival or equigingival prevents invasion of the periodontal pocket (biological width) and the subsequent damage to the gingiva and alveolar bone. In the present study, the desired occlusal height and the equigingival extension of the crowns were achieved by adjusting and trimming the gingival area of a crown using the appropriate scissor. The crown curvature was shaped with a Johnson Contouring Pliers #114 and the margin was crimped around the crown circumference to allow maximum marginal adaptation using 3M ESPE (3M ESPE, Seefeld, Germany) crimping pliers (800-421). The crown margin was finished and polished using a large rubber wheel. The correct SSC placement is determined by an audible clicking sound produced during lingual-buccal placement of the crown at the try-in stage, prior to cementation [Citation35].
Cementation of the stainless steel crown
The SSC’s were adjusted and the fit and extension were re-assessed before cementation onto the duplicated teeth while the teeth were in the mandibular phantom head. The rationale for using the cement was to secure the crown in a fixed position to allow accurate assessment of the margins. The crowns were cemented with Ketac Chem Easymix (3M ESPE, Seefeld, Germany). One spoon of the powder was mixed with two drops of the liquid according to the manufacturer’s instructions. Rhodamine B isothiocyanate dye (Merck, Darmstadt, Germany, item 283924) at a 0.066% concentration was incorporated into the cement. This served as a contrast medium to enable easier viewing of the marginal adaptation. The material was applied to the inner surface of SSC’s and the crowns were seated over the duplicated teeth by occluding the upper jaw of the phantom head with the lower. Upon completion of the setting time of the cement, excess material was removed using a probe and the teeth were cleaned using a pumice and brush on the typodont. All the teeth were then stored for 48 h at 35 °C and 95% humidity.
Although adhesion was obtained between the Ketac Cem Easymix and the polyester resin, it would not be the same as the ionic bond to tooth structure. However, the adhesion strength is irrelevant in the present study, as adhesion was not investigated.
Measurement of marginal adaptation and discrepancy with the stereomicroscope and digital camera
A stereomicroscope with an integrated digital camera was used. Measurements obtained from the stereomicroscope in conjunction with the digital camera were accurate. The advantage of working with a digital camera is that the image can be easily analyzed [Citation36]. The stereomicroscope with a camera for measuring the marginal accuracy of four different crowns showed a high accuracy [Citation21]. Each specimen was placed under a stereomicroscope (Nikon SMZ-10 Stereophoto, Tokyo, Japan) at 100× magnification. The measurements of the adaptation and discrepancy were recorded around the circumference of each specimen every 2 µm by using a micrometre screw gauge. Forty-eight measurements were recorded per specimen for marginal adaptation (inner surface of SSC to tooth structure) as well as for marginal discrepancy (side of SSC in relation to CEJ). The marginal adaptation and discrepancy of each crown was measured in millimeters using the image transferred from the camera (LEICA DFC 290, Leica Microsystems Ltd, Mannheim, Germany) attached to the stereomicroscope to the computer software (ACD see software V3.1, SPSS Inc., Chicago, IL), where the measurement was completed.
Results
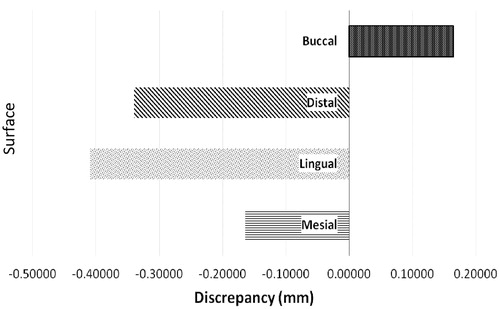
The measurements represented in mm for the circumference of the SSC were divided into four surfaces namely buccal, mesial, distal, and lingual as shown in .
Figure 6. Marginal adaptation of (A) lingual surface. (B) Buccal surface. (C) Mesial surface. (D) Distal surface.
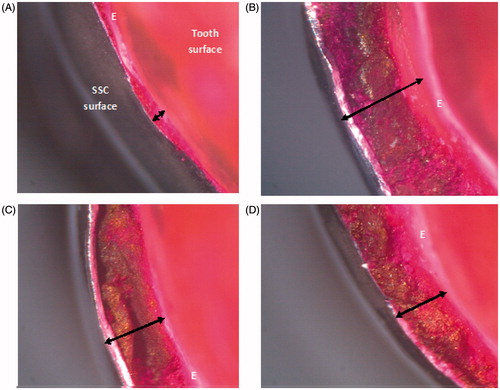
illustrates the mean value for the specific surface. A negative value for the discrepancy measurements illustrates that the margin of the SSC is extended beyond the CEJ. The buccal marginal adaptation was the worst (0.583 mm). The marginal discrepancy (0.164 mm) was significantly different from the other surfaces since it did not extend beyond the CEJ. The best marginal adaptation (0.260 mm) with a significance of p < .0001, as well as the worst discrepancy beyond the CEJ (−0.408) was found on the lingual aspect as shown in .
Table 1. Marginal adaptation and discrepancy per surface of SSCs.
The one-way ANOVA test showed that statistical differences (p < .05) are present. To determine which surface presented with the most optimal adaptation, multiple comparisons between all surfaces were done using the Tukey HSD test ( and ).
Table 2. Multiple comparisons for marginal adaptation.
Table 3. Multiple comparisons for marginal discrepancy.
and indicate no significant difference between the mesial, distal, and buccal surfaces for marginal adaptation.
The validity and reliability was assessed as the intra-observer reliability for the measurement obtained for marginal adaptation and discrepancy. The correlation of the two measurements was evaluated using the paired sample correlation test. This test showed that there was no statistically significant difference between the measurements in the first and second round measurements.
The null hypothesis for the marginal adaptation and discrepancy, which stated that SSC’s have no marginal adaptation/discrepancy and there is no difference in the marginal adaptation/discrepancy of SSC’s between the buccal/lingual surfaces compared with the proximal surfaces (mesial/distal) was rejected.
Discussion
Inadequate marginal adaptation and marginal discrepancy have a negative effect on the longevity and success of SSC’s [Citation11]. It is, therefore, important to assess the factors that influence the adaptation and fit of the crown.
In the present study, the best marginal adaptation of the SSC’s was found on the lingual surface and was statistically significant compared to the other surfaces. Anatomically, the lingual margin was straighter compared to the buccal aspect allowing for better adaptation [Citation37].
Although there was no significant difference between the mesial, distal, and buccal surfaces, the poorest marginal adaptation was reported on the buccal surface. This finding was confirmed by other studies where the mesial and lingual surfaces showed inadequate marginal adaptation and the most common surface with poor marginal fit was the buccal surface [Citation9,Citation22,Citation38]. This is likely due to the presence of the mesio-buccal bulge on the second mandibular primary molar. This mesio-buccal bulge (which is evident with the conventional SSC preparation as well) creates under cuts, which hamper crown adaptation during the crimping procedure, especially for the second mandibular primary molar [Citation38]. A significant reduction in the microleakage was reported upon reduction of the buccal bulge. Accordingly, the study advocated the additional tooth preparation of the buccal surface [Citation9]. Similarly, in the present study, the presence of mesio-buccal bulge contributed to the poor marginal adaptation on the buccal surface. In the event that the mesio-buccal bulge could be removed, the marginal adaptation will improve, since the bucco-lingual placement will not be hampered by the crimped SSC margin [Citation35].
Accurate crown adaptation at the margin around the tooth circumference can be achieved by crimping and curving the margin of the SSC. Radiographs can be used to evaluate the marginal adaptation and extension of the SSC at the interproximal areas before crown cementation [Citation39]. Accurate crown marginal adaptation at the mesial and distal surfaces can be detected by radiographic assessment while assessment of the buccal and lingual surfaces radiographically is difficult due to the radiopacity of the SSC on the radiographs. However, the use of this technique is not always feasible and clinically limited as it exposes the child to additional ionizing radiation [Citation12].
The probability of areas of poor adaptation and discrepancy always exists. The seal of the SSC is an important factor to its success. The luting cement has a crucial role in closing the gap between the crown and tooth by forming a tight seal that prevents microleakage. The degree of microleakage between various adhesive and non-adhesive luting cements was reported. The result was a significant reduction in microleakage when RMGIC together with an adhesive agent was used as luting cement as opposed to a RMGIC alone [Citation40]. This may improve the marginal seal and compensate for the marginal defects associated with SSC’s. RMGIC cements were found to have high physical strength and chemically bond to the tooth structure [Citation41].
In the present study, a uniform extension of the SSC margin around the circumference of the tooth was measured. Marginal discrepancies of all SSC’s were reported with two different values (negative and positive) in relation to the CEJ. Negative values were obtained in the discrepancy assessment for the mesial, distal, and lingual surfaces. The crowns, therefore, extended below the CEJ, which has the clinical implication that the crowns were placed more subgingival. The periodontium of a child has a normal pocket depth range between 0.2 and 1.2 mm [Citation42]. Over-extension of the crown’s margin will, therefore, result in invasion of the biological width of the primary tooth periodontium [Citation43]. Gingival bleeding, discomfort, secondary caries, and alveolar bone resorption can be considered signs of SSC failure. These signs of failure occurred due to several predisposing factors, such as poor marginal adaptation, marginal discrepancy, and encroachment of the biological width [Citation44–46]. The ideal crown extension should approximate the location of CEJ or be slightly occlusal to it [Citation11]. Clinically, this is ensured by using gingival blanching as an indicator of the position of the SSC margin. The SSC margin can be detected by using an explorer and periodontal probe [Citation23].
In this study, blanching could not be used as an indicator but an explorer and periodontal probe were used to detect the crown extension prior to cementation. This technique was found to be inaccurate based on the results. It is evident through the negative values obtained on the lingual, mesial, and distal surfaces. These areas are, therefore, clinically relevant to the clinician.
The method of marginal trimming using scissors to reduce the crown to the appropriate height has a negative effect on the crown fit around the tooth circumference as it may lead to under- and over-extended margins and may result in marginal discrepancy due to inaccurate trimming. To achieve good marginal fit with more precise marginal trimming, the use of a large rotary abrasive stone is suggested [Citation11].
The contour of the gingival margin is difficult to follow during the trimming procedure. Clinically, a probe is used to carve a faint line that follows the contour of the gingival margin. This faint line gives an indication of where the crown should be trimmed. However, during the trimming procedure, it is very difficult to follow the curved line accurately. How accurate the crown is trimmed does not depend only on the trimming instrument but also on the ability of the clinician to trim the crown exactly to the line that has been carved into the crown. All of these factors influence the accuracy of the crown extension around the tooth circumference and may contribute to the marginal discrepancy.
All SSCs require further manipulation prior to placement [Citation11]. Accurate marginal adaptation and fit can be achieved by (1) selecting the appropriate size of the crown, (2) trimming the crown margin accurately for appropriate length, (3) crimping the crown edges to approximate the prepared area, and (4) finishing, and polishing the margins of the crown [Citation47]. This is where the learning curve is essential and dependent on the operator’s skill. Follow-up care and oral health practices have been shown to enhance the survival rate with a very low occurrence (0.7%) of gingival inflammation as demonstrated with the placement of preformed stainless steel crowns in a disabled population [Citation48].
The longevity of SSC’s compared with multi-surface amalgam restorations over an eight-year period produced various failure rates over time. The failure rate of SSC’s was 8% after 3 years, 10% after 4.5 years, and 17% after 8 years. The amalgam restorations showed 34% failure after 3 years and 64% after 4.5 years. After 4.5 years, they reported a total of 60% failure for amalgam restorations compared with a 10% failure rate for SSC’s [Citation49]. Hence, the appropriate marginal adaptation to the tooth and a reduced discrepancy beyond the CEJ is essential. The SSC has a highly polished surface that limits bacterial adhesion and biofilm formation [Citation50]. It is, therefore, effective in patients with special needs where routine oral hygiene is impaired [Citation51]. For the same reason, SSC’s are recommended for children with high caries risk [Citation7].
Conclusion
The present study concluded that marginal discrepancies occur during the trimming procedure and assessment of the gingival approximation of the SSC margin. More attention should be paid to the crimping procedure and a pre-cementation radiograph can assist in ensuring that maximum adaptation will be achieved at the mesial and distal interdental areas.
It was determined that the crown morphology of the primary tooth plays an important role in the marginal adaptation of the crown. Crown bulges create areas of undercuts that may compromise SSC adaptation. Although crimping of the crown margin is used in all dental practices as a standard protocol for SSC placement and approximation of the crown margin to the tooth surface, this study showed that, when using only a probe as a guide to determine the adaptation and discrepancy, a significant marginal gap exists between the SSC and the tooth structure.
Additionally, the marginal discrepancies occur purely due to the use of a scissor during trimming.
Knowledge and skill level of the operator contribute to the success of SSC’s. Educating clinicians regarding adequate marginal adaptation and proper crown fit are likely to result in greater SSC success.
Recommendations for clinical application
Crimping and adaptation procedures have been used extensively for pre-formed crowns. However, based on the results of this study, marginal adaptation and discrepancy remains an issue. Certain clinical recommendations for adaptation and cementation can be made to guide clinicians and increase the chances of success of SSC placement:
Based on the results of this study, modification of the conventional SSC tooth preparation technique could be considered by reducing the buccal bulge [Citation9] somewhat and ensuring adequate crimping to improve the marginal adaptation of the SSC.
Considering the adaptation and discrepancy illustrated in the present study, RMGIC is preferred to GIC cements, which are prone to hydrolytic degradation, thereby compromising the marginal integrity. RMGIC together with the use of an adhesive is highly recommended to seal the gap between the crown and tooth in order to prevent microleakage and improve the marginal seal [Citation40]. The use of self-adhesive resin or self-adhesive RMGIC cements will reduce the number of steps required [Citation42].
Limitations of the study
Although this study was conducted to simulate the intra-oral procedure for SSC placement, some shortcomings were detected. Due to the presence of the thick plastic gingiva in the phantom head, marginal extension of the crown could not be detected as readily as in the clinical setting, which is indicated by gingival blanching.
Additionally, this study did not evaluate the significance of this marginal gap in the presence of luting cements in relation to microleakage.
Acknowledgements
This study formed part of a Masters project.
Disclosure statement
Authors have no relevant financial or non-financial relationship to disclose. All authors have made substantive contribution to this manuscript, and all have reviewed the final paper prior to its submission.
References
- Innes NP, Ricketts D, Chong LY, et al. Preformed crown for decayed primary molar teeth. Cochrane Database of Syst Rev. 2015;12:CD005512.
- Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. Am J Public Health. 1992;82:1663–1668.
- Tinanoff N, Douglass JM. Clinical decision-making for caries management in primary teeth. J Dent Educ. 2001;65:1133–1142.
- Ilie N, Hickel R. Mechanical behavior of glass ionomer cements as a function of loading condition and mixing procedure. Dent Mater J. 2007;26:526–533.
- Lenters M, van Amerongen WE, Mandari GJ. Iatrogenic damage to the adjacent surface of primary molars in three different ways of cavity preparation. Eur Arch Paediatr Dent. 2006;1:6–10.
- Hickel R, Kaaden C, Paschos E, et al. Longevity of occlusally-stressed restorations in posterior primary teeth. Am J Dent. 2005;18:198–211.
- American Academy of Paediatric Dentistry. Guideline on Paediatric Restorative Dentistry. Ref Man 2016/17;38:250–262.
- Humphrey WP. Chrome alloy in children’s dentistry. St. Louis Dent Soc 1950;21:15–16.
- Ramazani M, Ramazani N, Honarmand M, et al. Gingival evaluation of primary molar teeth restored with stainless steel crowns in Pediatric Department of Zahedan-Iran Dental School – a retrospective study. J Mash Dent Sch. 2010;34:125–134.
- Sajjanshetty S, Patil PS, Hugar D, et al. Pediatric preformed metal crowns – an update. J Dent Allied Sci. 2013;2:29–32.
- Croll TP, Epstein DW, Castaldi CR. Marginal adaptation of stainless steel crowns. Pediatr Dent. 2003; 25:249–252.
- Randall RC. Preformed metal crowns for primary and permanent molar teeth: review of the literature. Pediatr Dent. 2002;24:489–500.
- Seale NS. The use of stainless steel crowns. Pediatr Dent. 2002;24:501–505.
- Seale NS, Randall R. The use of stainless steel crowns: a systematic literature review. Pediatr Dent. 2015;37:147–162.
- Moskowitz M, Sammara H, Holan G. Success rate of root canal treatment in primary molars. J Dent. 2005;33:41–47.
- Tonmukayakul U, Martin R, Clark R, et al. Protocol for the Hall technique study: a trial to measure clinical effectiveness and cost-effectiveness of stainless steel crowns for dental caries restoration in primary molars in young children. Contemp Clin Trials. 2015;44:36–41.
- Guelmann M, Shapira J, Silva DR, et al. Esthetic restorative options for pulpotomized primary molars: a review of literature. J Clin Pediatr Dent. 2011; 36:123–126.
- Holmes JR, Bayne SC, Holland GA, et al. Considerations in measurement of marginal fit. J Prosthet Dent. 1989;62:405–408.
- Mously HA, Finkelman M, Zanparsa R, et al. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J Prosthet Dent. 2014; 112:249–256.
- Rector JA, Mitchell RJ, Spedding RH. The influence of tooth preparation and crown manipulation on the mechanical retention of stainless steel crowns. ASDC J Dent Child. 1984;52:422–427.
- Amin BM, Aras MA, Chitre V. A comparative evaluation of the marginal accuracy of crowns fabricated from four commercially available provisional materials: an in vitro study. Contemp Clin Dent. 2015;6:161–165.
- Erdemci ZY, Çehreli SB, Tirali RE. Hall versus conventional stainless steel crown techniques: in vitro investigation of marginal fit and microleakage using three different luting agents. Pediatr Dent 2014; 36:286–290.
- Bader JD, Rozier RG, McFall WT, et al. Effect of crown margins on periodontal conditions in regularly attending patients. J Prosthet Dent. 1991;65:75–79.
- Webber DL. Gingival health following placement of stainless steel crowns. ASDC J Dent Child. 1974;41: 186–189.
- Durr DP, Ashrafi MH, Duncan WK. A study of plaque accumulation and gingival health surrounding stainless steel crowns. ASDC J Dent Child. 1981; 49:343–346.
- Hutcheson C, Seale NS, McWhorter A, et al. Multi-surface composite vs stainless steel crown restorations after mineral trioxide aggregate pulpotomy: a randomized controlled trial. Pediatr Dent. 2012;34: 460–467.
- Groten M, Axmann D, Pröbster L, et al. Determination of the minimum number of marginal gap measurements required for practical in-vitro testing. J Prosthet Dent. 2000;83:40–49.
- Lee KB, Park CW, Kim KH, et al. Marginal and internal fit of all-ceramic crowns fabricated with two different CAD/CAM systems. Dent Mater J. 2008;27:422–426.
- Gonzalo E, Suárez MJ, Serrano B, et al. A comparison of the marginal vertical discrepancies of zirconium and metal ceramic posterior fixed dental prostheses before and after cementation. J Prosthet Dent. 2009;102:378–384.
- Nawafleh NA, Mack F, Evans J, et al. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: a literature review. J Prosthodont. 2013;22:419–428.
- Meyer DR, Bell RA, Arenie JT. The effect of cement type and tooth preparation on the retention of stainless steel crowns. J Pedod. 1981;5:275–280.
- Seraj B, Shahrabi M, Motahari P, et al. Microleakage of stainless steel crowns placed on intact and extensively destroyed primary first molars: an in vitro study. Pediatric Dentistry. 2011;33:525–528.
- Krämer N, Rudolph H, Garcia-Godoy F, et al. Effect of thermo-mechanical loading on marginal quality and wear of primary molar crowns. Eur Arch Paediatr Dent. 2012;13:185–190.
- Fayle SA. UK national clinical guidelines in paediatric dentistry. Int J Paediatr Dent. 1999;9:311–314.
- Goldberg NL. The stainless steel crown in pediatric dentistry. Dent Dig. 1969;75:352–355.
- De Santi Alvarenga FA, Pinelli C, Loffredo LDCM. Reliability of marginal microleakage assessment by visual and digital methods. Eur J Dent. 2015;9:1–5.
- McDonald RE, Avery DR. Development and morphology of the primary teeth. In McDonald and Avery Dentistry for the Child and Adolescent. 8th ed. Mosby: JA Elsevier Health Sciences; 2004. pp. 50–58.
- Woo JH, Jang CH, Kim JW, et al. Marginal adaptation of stainless steel in posterior primary tooth. J Korean Acad Pediatr Dent. 2007;34:27–35.
- More FG, Pink TC. The stainless steel crown: a clinical guide. J Mich State Dent Assoc. 1973;55: 237–242.
- Memarpour M, Derafshi R, Razavi M. Comparison of microleakage from stainless steel crowns margins used with different restorative materials: an in vitro study. Dent Res J. 2016;13:7–12.
- Li Y, Lin H, Zheng G, et al. A comparison study on the flexural strength and compressive strength of four resin-modified luting glass ionomer cements. BME. 2015;26:S9–S17.
- Pathak A, Nandlal B. Clinical evaluation of gingival sulcus depth in primary dentition by computerized, pressure-sensitive Florida Probe. GMJ. 2016;5: S43–S51.
- Sharma A, Rahul GR, Gupta B, et al. Biological width: no violation zone. Eur J Gen Dent. 2012;1: 137–141.
- Sharaf AA, Farsi NM. A clinical and radiographic evaluation of stainless steel crowns for primary molars. J Dent. 2004;32:27–33.
- Atieh M. Stainless steel crown versus modified open-sandwich restorations for primary molars: a 2-year randomized clinical trial. Int J Paediatr Dent. 2008;18:325–332.
- López DM, Buendía EMV, Sánchez MRR, et al. Predisposing factors for gingival inflammation associated with steel crowns on temporary teeth in the pediatric population. A systematic literature review. Rev Fac Odontol Univ Antioq. 2014;26:152–163.
- Afshar H, Ghandehari M, Soleimani B. Comparison of marginal circumference of two different pre-crimped stainless steel crowns for primary molars after re-crimping. J Dent. 2015;12:926–931.
- Martinez-Cerecero ER, Ponce-Gallegos JA, Pozos-Guillen A, et al. Clinical success of preformed steel crowns in disabled pediatric population: an 11-year retrospective study. Pedaitr Dent J. 2017;27:142–146.
- Einwag J, Dünninger P. Stainless steel crown versus multisurface amalgam restorations: an 8-year longitudinal clinical study. Quintessence Int. 1996;27: 321–323.
- Bin Alshaibah WM, El-Sehaby FA, El-Dokky NA, et al. Comparative study on the microbial adhesion to preveneered and stainless steel crowns. J Indian Soc Pedod Prev Dent. 2012;3:206–211.
- Kindelan SA, Day P, Nichol R, et al. UK national clinical guidelines in paediatric dentistry: stainless steel performed crowns for primary molars. Int J Paediatr Dent. 2008;18:20–28.