Abstract
Aim: The use of colored translucent zirconia may enable restorations of a more natural tooth-like appearance than previous opaque white zirconia. The shift from non-colored to colored zirconia may however entail a risk of reduced strength. The aim of the present study was to compare fracture load and fracture mode of fixed dental prostheses frameworks made of colored translucent zirconia to that of non-colored controls.
Methods: A total of forty three-unit FDP frameworks were manufactured from two different high translucent zirconia materials (Zenostar, Wieland Dental, and DD cubeX2, Dental Direkt). Each group contained two subgroups, one colored and one non-colored. Coloring was performed before final sintering using two different infiltration techniques. All FDPs underwent an artificial aging process in the form of heat treatment, thermocycling and preloading whereafter the specimens were subjected to load until fracture. Fracture load and mode was registered.
Results: For one of the zirconia materials, Zenostar, the non-colored frameworks showed significantly higher fracture loads (p < .0001) compared to its colored counterpart. No significant difference (p > .05) was found between colored and non-colored frameworks in the other zirconia material, DD cubeX2. All FDPs fractured through the connector. Some fractures ran through the mesial and some through the distal side of the connector but there were no significant differences in fracture mode between groups.
Conclusion: Coloring before sintering of high-translucent zirconia may decrease the fracture load of FDP frameworks for certain materials and techniques. Fracture mode however, does not appear to be affected.
Introduction
Yttrium-oxide stabilized tetragonal zirconia polycrystals (Y-TZP), often referred to as zirconia, is considered a reliable material for dental restorations such as crowns and fixed dental prostheses (FDPs) [Citation1,Citation2]. The unique transformation toughening properties of Y-TZP give the material excellent mechanical properties, and it was introduced as a stronger and tougher material compared to previous ceramic alternatives [Citation3]. Zirconia has not been used as long as the gold standard, metal ceramics, so there is not yet enough data for long-term comparisons, but several trials present predictable and comparable five-year survival results [Citation1,Citation2,Citation4]. Despite the excellent mechanical properties of zirconia as a core material, superficial chip-off fractures in the veneering porcelain have been reported as a common issue and it is the primary reason for clinical failure of veneered zirconia [Citation1,Citation2,Citation4]. With recent material developments, such as improved translucency and coloring options, there is a possibility today, to make monolithic zirconia restorations without the need for veneering porcelain to cover its previous original opaque, white appearance [Citation5–7]. With monolithic restorations, the risk of veneer fractures is eliminated.
Improved translucency is achieved by reducing porosity size and quantity, reducing impurities, keeping grain sizes small and uniform, and controlling types and amount of dopants [Citation8,Citation9]. To further enable a tooth-like appearance, coloring is necessary [Citation5]. Previously, zirconia restorations were individualized using a staining technique. This method involves painting of the finished restoration and requires a final firing in a traditional dental ceramic furnace, similar to the painting of feldspathic porcelain. This is generally not regarded as coloring, since only the surface of the material is treated and the color effect is sensitive to adjustments such as occlusal grinding and normal wear. To achieve lasting coloring of zirconia, that permeates through the entire core of the material, two different methods may be used [Citation10]. One method involves mixing of metal oxides into the powdered zirconia material before sintering, thus producing pre-colored green-stage blocks. Another method uses an infiltration technique where chloride solutions of rare earth elements are added to machined restorations at the pre-sintered green-stage [Citation10].
The shift from traditional non-colored zirconia to colored translucent zirconia may entail a risk of reduced strength of the material [Citation7,Citation11]. The toughness of zirconia is dependent on its phase-transformation ability [Citation12,Citation13]. At an optimal grain size, the tetragonal grains can expand at the crack tip, and transform to a monoclinic, stable phase and prevent further crack propagation [Citation12,Citation13]. The processes that enhance translucency, and the added coloring elements, have been shown to affect the mechanical properties of the material [Citation7,Citation11]. The influence of coloring on flexural strength and fracture toughness has been debated. Some studies suggest that coloring decreases the flexural strength of the material, while other studies have not found such differences [Citation11,Citation14–16].
Several different zirconia materials have been evaluated using slightly different methods, which makes it difficult to draw clear and definitive conclusions. Most studies have evaluated simplified specimen designs, such as disk- or bar-shaped specimens. The shape and design of the specimens, as well as the type of zirconia material, significantly influence test results [Citation17]. Alghazzawi et al. [Citation17] found that results from bar-shaped specimens differed from those of crown-shaped specimens when analyzing different translucent zirconia materials. They concluded that the mechanical properties of zirconia should be tested using clinically relevant specimen shapes and functional simulated conditions. This recommendation is in agreement with a majority of other publications that emphasize the importance of a test set-up that simulates the clinical situation as far as possible [Citation18–20].
Few studies have evaluated the most complex type of restoration, fixed dental prostheses, despite available evidence of complex force distributions within FDPs [Citation21]. Attention to the design of an FDP is crucial to avoid failure. Factors such as framework thickness, design of the connectors and the radius of gingival embrasure need to be controlled [Citation22,Citation23].
The aim of the present study was to compare the fracture load and fracture mode of non-colored and colored anterior three-unit high-translucent zirconia FDP frameworks. The null hypothesis was that there would be no differences in fracture load and fracture mode of FDP frameworks made from high-translucent colored and high-translucent non-colored zirconia.
Materials and methods
Abutment preparation, scanning and milling
All procedures were performed by the same operator and according to each respective manufacturer’s recommendations. Abutment preparations were made on a central incisor (21) and a canine (23) on a plastic model of an upper jaw (KaVo Dental, Biberach, Germany) with missing tooth 22. The preparations had a 120-degree chamfer finish line and a 15-degree angle of convergence. A full arch impression was made of the preparations using an A-silicone impression material (Flexitime Mono Phase, Heraeus Kulzer, Hanau, Germany) and poured with die stone (Everest Rock, Type 4 die stone, KaVo Dental) to produce a master cast. The master cast was scanned using a mechanical scanner (Procera Forte, Nobel Biocare, Zurich, Switzerland). The connector dimensions were set to 3 × 3 mm with a minimum abutment core thickness of 0.7 mm. The radius of the curvature of the gingival embrasure set to 0.9 mm. The CAD data for the FDP frameworks were subsequently sent to a milling machine (Wieland Select Hybrid, Wieland Dental, Pforzheim, Germany), and forty FDP frameworks were milled using the appropriate software (CAM V.3.4.029 x64 Advanced, Wieland Dental).
Coloring
Three-unit zirconia FDP frameworks were manufactured from two different high translucent zirconia materials (Zenostar MT0, Wieland Dental, and DD cubeX2, Dental Direkt, Spenge, Germany); 20 in each group. The FDP frameworks were divided into two subgroups of ten. One group of FDP frameworks from each zirconia material went through a coloring process; Zenostar MT0 colored and DD cubeX2 colored. The remaining frameworks were sintered without coloring; Zenostar MT0 non-colored and DD cubeX2 non-colored, and acted as control groups ().
Table 1. Overview of the different groups of specimens.
Coloring was achieved using manual techniques recommended by the manufacturers and the same operator performed the coloring of all specimens. The DD Bio ZX2 monolith zero Dentin A3 (Dental Direkt) coloring liquid was used for DD cubeX2 FDP frameworks. The Wieland Dental Zenostar MT Color (Wieland Dental) coloring liquid was used for the Zenostar MT0 FDP frameworks. DD cubeX2 was colored using an immersion technique, whereas Zenostar MT0 was colored with the brush infiltration technique. Coloring was done in the pre-sintered stage before final sintering in a dental ceramic furnace (Austromat 654, Dekema Dental-Keramiköfen, Freilassing, Germany) according to the manufacturers’ recommendations.
Heat treatment and artificial aging
To keep the design of the FDPs standardized, no veneering porcelain was added. All FDP frameworks were however heat-treated to simulate veneering process. The heat-treatment comprised four programs: a wash bake at 950 °C with 8 min heating and 1 min hold time, dentin 1 at 910 °C with 7 min heating and 1 min hold time, dentin 2 at 900 °C with 7 min heating and 1 min hold time, and a final glaze firing at 900 °C with 5 min heating and 1 min hold time. Starting temperature was 500 °C for all bakes with a 2–6 min predrying time. The firing was done in a calibrated furnace (Programat EP 5000, Ivoclar Vivadent, Schaan, Liechtenstein) according to the Vita VM9 (VITA Zahnfabrik, Bad Säckingen, Germany) firing program. To simulate fatigue, the crowns then underwent 5,000 cycles of thermocycling between two water baths, 5 °C and 55 °C, in a thermocycling device (Thermocycler THE-1100, SD Mechatronics, Feldkirchen-Westerham, Germany). Each cycle lasted 60 s: 20 s in each bath and 10 s to transfer between baths.
Cementation
The supporting tooth analogs were made from the CAD file used to produce the FDP frameworks. Eighty supporting tooth analogs were produced from a polymer material (Formlabs Black Resin GPBK02, Somerville, MA, USA) using additive manufacturing technique, 3 D printing, (Formlabs 2, Formlabs). The FDP frameworks and the polymer tooth analogs were steam cleaned and air dried, and subsequently treated with a primer (ED primer II A and B Kuraray Dental, Tokyo, Japan) prior to cementation using a dual-cured resin cement (Panavia v5, Kuraray Dental). A load of 15 N was applied for 60 s in the direction of insertion during setting of the cement. The cement was light-cured using a curing lamp (Heraeus Translux Power Blue, Heraeus Kulzer). To prevent desiccation after cementation, the FDP frameworks were kept in a moist environment until load to fracture. A plastic container with a sealable lid and a thin layer of distilled water was used and the containers were stored at a temperature of 37 ± 1 °C stored in an incubator (Memmert Incubator, Memmert, Schwabach, Germany).
Cyclic load and load until fracture
To further simulate fatigue, the FDPs underwent cyclic loading before final load to fracture. The FDP frameworks were mounted at a 10° inclination relative to the vertical plane in a specialized machine (MTI Engineering AB/Pamaco AB, Malmö, Sweden), and subjected to 10,000 cycles between 30–300 N in a sinusoid wave load profile at 1 Hz. The load was applied with a steel indenter (∅ = 2.5 mm) exerted centrally on the pontic, with a 1 mm thick plastic foil (Erkoflex, Erkodent, Pfalzgrafenweiler, Germany) placed between the steel indenter and the FDP frameworks. The process was performed in water. Finally, the FDP frameworks were mounted in a universal testing machine (Instron 4465, Instron, High Wycomde, UK) at an inclination of 10°, with a 1 mm thick plastic foil (Erkoflex, Erkodent) placed between the steel indenter and the incisal edge of the pontic. Load was applied perpendicular to the central part of the incisal edge of the pontic with a stainless steel indenter (∅ = 2.5 mm) at a crosshead speed of 0.255 mm/min. The FDP frameworks were loaded until fracture, which was defined as a visible fracture though the entire construction. Fracture mode was determined by visual inspection.
Statistical analysis
Data on fracture load was analyzed using One-way ANOVA and Tukey’s test. Data from fracture mode observations were analyzed using Fisher’s exact test. The level of significance was set at p < .05.
Results
Fracture load
The non-colored FDP frameworks made from Zenostar MT0 showed the highest fracture loads, significantly higher (p < .0001) compared to the colored ones. No significant difference was found between colored and non-colored FDP frameworks made from DD cubeX2. Non-colored FDP frameworks made from Zenostar MT0 also demonstrated a significantly higher (p < .0001) fracture loads than non-colored FDP frameworks made from DD cubeX2. Regarding the two colored subgroups, Zenostar MT0 colored FDP frameworks showed significantly lower (p < .0001) fracture loads compared to DD cubeX2 colored FDP frameworks ().
Table 2. Fracture strength (N); load at fracture for each specimen, mean and standard deviation (SD) for each group.
Fracture mode
The fractures ran through either the mesial or the distal side of the connector ( and ; ). There were no differences between the groups regarding fracture mode.
Figure 1. Fracture of a non-colored FDP framework propagating from the mesial side of the connector to the site of the indenter. Fracture marked by arrows.
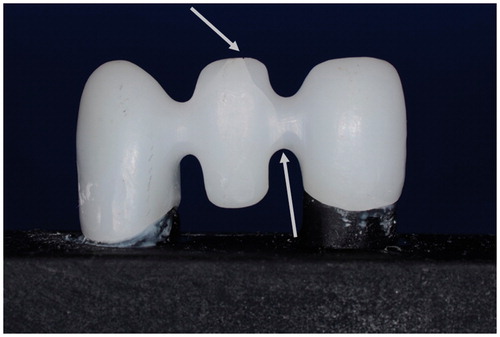
Figure 2. Fracture of a colored FDP framework, propagating from the distal side of the connector to the site of the indenter. Fracture marked by arrows.
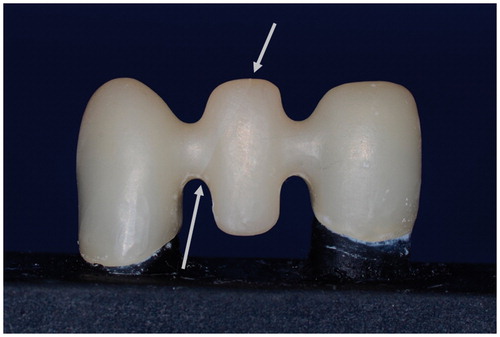
Table 3. The distribution of fracture mode for each group.
No abutment failure was observed.
Discussion
The hypothesis that there was no difference in fracture load between colored and non-colored material was rejected for one of the translucent zirconia materials, Zenostar MT0, but not for the other, DD cubeX2. The results from the present study thus indicate that the effect of coloring on fracture loads differs between materials from different manufacturers using different coloring techniques. The results are in agreement with similar studies that analyze coloring effect on translucent zirconia and found coloring to negatively affect strength [Citation14,Citation15]. In contrast, another study reported no negative effects of coloring, but that paper analyzed traditional non-translucent zirconia[Citation16].
The differences between the two zirconia materials in the present study is likely explained by two factors; chemical composition of the coloring liquids, and coloring technique. The use of coloring metal oxides has the potential to cause microstructural and crystallographic changes, which in turn can alter the mechanical properties of the material. For instance, coloring oxides can alter the grain size and decrease the materials ability of phase transformation, or render it less stable with an increase of the monoclinic phase [Citation14]. Different metal oxides have been shown to be more or less prone to cause a decrease of the fracture strength [Citation14]. Shah et al concluded that the effect on flexural strength varied depending on the different coloring elements, cerium or bismuth salts [Citation14]. Furthermore, differences in concentration of coloring elements may also influence fracture strength [Citation14]. The flexural strength decreased linearly with increasing concentration and the decrease was attributed to an increase in porosities at higher concentrations of metal oxides [Citation14]. The study further concluded that coloring with cerium or bismuth salts produced perceptible color differences even at the lowest concentrations [Citation14]. There is thus no need for excessive concentrations of coloring elements which risk introducing negative effects on strength. A limitation in the present study was that the composition of the coloring liquids was not examined. Furthermore, the manufacturers did not provide the exact composition of the coloring liquids.
Differences in coloring technique of the two zirconia materials may provide an additional explanation of the results. DD cubeX2 was colored using an immersion infiltration technique, whereas Zenostar MT0 was colored with the brush infiltration technique. The brush infiltration technique requires precise application of a number of consecutive brush strokes. The technique is more operator-dependent and precise replication of application for all specimens is complicated [Citation10]. This could lead to changes in mechanical properties of the material, contributing to the difference in fracture loads observed between the colored and non-colored Zenostar MT0 zirconia. A previous study has recommended the immersion technique over the brush infiltration technique since it provides better control of value, and has the ability to more closely replicate the natural tooth shade [Citation10]. It is possible that the immersion technique has better potential as a coloring technique. With the immersion technique, it is important to control the immersion time. Hjerppe et al. [Citation15] performed coloring using immersion times according to the manufacturer’s recommendations, as well as prolonged immersion times. The authors found only a slight decrease in flexural strength at the correct immersion time, but prolonged immersion times caused significant decreases in flexural strength [Citation15]. In the present study, the manufacturers’ recommendations were strictly followed.
There were no significant differences concerning fracture mode. All fractures occurred around the connector. This is in accordance with previous laboratory studies that have found the highest stresses in ceramic FDPs located in the connector areas [Citation19–22]. Most clinical failures of zirconia FDPs originate in this area [Citation1,Citation2,Citation4].
Despite the noted differences between groups of FDP frameworks in the present study, all FDP frameworks sustained a fracture load that may be considered sufficient for clinical use as recommended by the manufacturers’, i.e. single tooth restorations and 3-unit FDPs. It is however important to remark that there was a significant difference in fracture loads between the two control groups of this study, Zenostar MT0 non-colored and DD cubeX2 non-colored, yet again highlighting that there are differences concerning material composition and processing techniques between different manufacturers.
Strengths and limitations
The fact that one operator, a skilled and experienced dental technician, performed all procedures in all test groups is a strength in the present study. Furthermore, all frameworks were subjected to artificial aging procedures. Thermocycling in water and heat treatment e.g. may affect fracture resistance negatively [Citation13]. Although some reports have failed to show significant effects of artificial aging, it may be prudent to perform these pretesting procedures to avoid creating unrealistically high in-vitro fracture loads.
The manufacturer’s first hand choice of primer/adhesive in combination with the dual-cured cement was not used, instead another of the primers from the manufacturer was used. This is however unlikely to have significantly influenced the results. This study evaluated a limited number of materials and specimens. In order to establish recommendations and clinical guidelines for the dental practitioner, further studies need to be performed comparing different zirconia materials, coloring elements and techniques.
Conclusions
Within the limitations of this study, the following statements are made:
Fracture loads differ between different manufacturers and coloring techniques.
Coloring of translucent zirconia FDP frameworks using brush infiltration technique may decrease fracture load.
Coloring of translucent zirconia FDP frameworks with immersion infiltration technique does not appear to affect fracture load.
Fracture mode does not appear to be influenced by coloring.
Disclosure statement
The authors declare no conflict of interest.
References
- Le M, Papia E, Larsson C. The clinical success of tooth- and implant-supported zirconia-based fixed dental prostheses. A systematic review. J Oral Rehabil. 2015;42:467–480.
- Pjetursson BE, Sailer I, Makarov M, et al. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part II: Multiple-unit FDPs. Dent Mater. 2015;31:624–639.
- Guazzato M, Albakry M, Ringer SP, et al. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II. Zirconia-based dental ceramics. Dent Mater. 2004;20:449–456.
- Heintze SD, Rousson V. Survival of zirconia- and metal-supported fixed dental prostheses: a systematic review. Int J Prosthodont. 2010;23:493–502.
- Vichi A, Louca C, Corciolani G, et al. Color related to ceramic and zirconia restorations: a review. Dent Mater. 2011;27:97–108.
- Wang F, Takahashi H, Iwasaki N. Translucency of dental ceramics with different thicknesses. J Prosthet Dent. 2013;110:14–20.
- Zhang Y. Making yttria-stabilized tetragonal zirconia translucent. Dent Mater. 2014;30:1195–1203.
- Harianawala HH, Kheur MG, Apte SK, et al. Comparative analysis of transmittance for different types of commercially available zirconia and lithium disilicate materials. J Adv Prosthodont. 2014;6:456–461.
- Zhang H, Li Z, Kim BN, et al. Effect of alumina dopant on transparency of tetragonal zirconia. J Nanomaterials. 2012;2012:1–5.
- Hassan AA, Torabi A, Mahdavi F, et al. The effect of two shading techniques on value of zirconia-based crowns. J Dent. 2015;16:129–133.
- Aboushelib MN, de Jager N, Kleverlaan CJ, et al. The influence of pigments on the slow crack growth in dental zirconia. Dent Mater. 2012;28:410–415.
- Hannink RHJ, Kelly PM, Muddle BC. Transformation toughening in zirconia-containing ceramics. J Am Ceram Soc. 2000;83:461–487.
- Rekow ED, Silva NRFA, Coelho PG, et al. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011;90:937–952.
- Shah K, Holloway JA, Denry IL. Effect of coloring with various metal oxides on the microstructure, color, and flexural strength of 3Y-TZP. J Biomed Mater Res Part B Appl Biomater. 2008;87:329–337.
- Hjerppe J, Narhi T, Froberg K, et al. Effect of shading the zirconia framework on biaxial strength and surface microhardness. Acta Odontol Scand. 2008;66:262–267.
- Sedda M, Vichi A, Carrabba M, et al. Influence of coloring procedure on flexural resistance of zirconia blocks. J Prosthet Dent. 2015;114:98–102.
- Alghazzawi T, Janowski GM. Correlation of flexural strength of coupons versus strength of crowns fabricated with different zirconia materials with and without aging. J Am Dent Assoc. 2015;146:904–912.
- Anusavice KJ, Kakar K, Ferree N. Which mechanical and physical testing methods are relevant for predicting the clinical performance of ceramic-based dental prostheses? Clin Oral Implants Res. 2007;18:218–231.
- Kohorst P, Dittmer MP, Borchers L, et al. Influence of cyclic fatigue in water on the load-bearing capacity of dental bridges made of zirconia. Acta Biomater. 2008;4:1440–1447.
- Mahmood DJ, Linderoth EH, Vult Von Steyern P. The influence of support properties and complexity on fracture strength and fracture mode of all-ceramic fixed dental prostheses. Acta Odontol Scand. 2011;69:229–237.
- Glantz PO, Strandman E, Svensson A, et al. On functional strain in fixed mandibular reconstructions. An in vitro study. Acta Odontol Scand. 1984;42:241–249.
- Oh WS, Anusavice KJ. Effect of connector design on the fracture resistance of all-ceramic fixed partial dentures. J Prosthet Dent. 2002;87:536–542.
- Bahat Z, Mahmood DJ, Vult von Steyern P. Fracture strength of three-unit fixed partial denture cores (Y-TZP) with different connector dimension and design. Swed Dent J. 2009;33:149–159.
