Abstract
Background: Clear definitions for septic shock assist clinicians regarding recognition, treatment and standardized reporting of characteristics and outcome of this entity. Sepsis-3 definition of septic shock incorporates a new criterion, a lactate level >2 mmol/L. Differences in epidemiology and outcome of septic shock based upon both definitions were studied in an intensive care (ICU) population of septic patients.
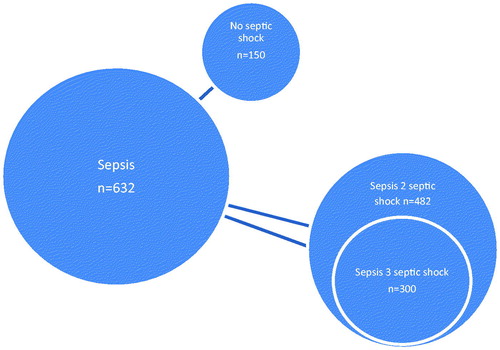
Methods: We analyzed a prospectively collected cohort of data in the ICU of the Maastricht University Medical Centre. 632 septic patients were included. ICU mortality was compared between the patient group fulfilling Sepsis-3 definition for septic shock and those that met Sepsis-2 definition. Furthermore, association between lactate levels and ICU mortality was studied.
Results: Of 632 septic patients, 482 (76.3%) had septic shock according to Sepsis-2 and 300 patients (48.4%) according to Sepsis-3 definition, respectively. Patients meeting Sepsis-3 definition had a higher mortality than patients meeting Sepsis-2 definition (38.9 vs. 34.0%). Serum lactate levels between 2 and 4 mmol/L (25.0 vs. 26.2%, OR 0.94 (0.5–1.5)) and between 4 and 6 mmol/L (23.8 vs. 26.2%, OR 0.88 (0.4–1.7)) compared to levels ≤2 mmol/L were not associated with significantly higher ICU mortality. Serum lactate values ≥6 mmol/L, were significantly associated with increased ICU mortality.
Conclusion: Patients classified according to Sepsis-3 criteria had a higher ICU mortality compared with Sepsis-2 criteria. Lactate levels <6 mmol/L were not able to identify patients with increased ICU mortality. Lactate threshold of 2 mmol/L may be too low to point out patients with actual increased ICU mortality.
Introduction
Sepsis is a life threatening syndrome following a dysregulated host response to infection. It causes major public health concerns [Citation1], has an increasing reported incidence and in-hospital mortality rates greater than 10% [Citation2]. Septic shock is a subset of sepsis in which underlying circulatory and cellular abnormalities are associated with substantially increased ICU mortality rates greater than 40%.
Clear definitions for sepsis and septic shock guide clinicians regarding early recognition and treatment and facilitates standardized reporting of characteristics and outcome leading to greater consistency of epidemiologic studies and clinical trials. In the past, multiple definitions for sepsis and septic shock were in use, resulting from differences in selected clinical variables [Citation3]. Recently the Third International Consensus Definitions Task Force of the Society of Intensive Care Medicine and European Society of Intensive Care Medicine revised the definitions for sepsis and septic shock (Sepsis-3 definition). Sepsis was herein defined as ‘an organ dysfunction characterized by a rise in Sequential Organ Failure Assessment (SOFA) score of more than 2, due to an exaggerated host response to infection’ [Citation4]. Septic shock was defined as a subset of sepsis in which particularly profound circulatory, cellular and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Sepsis-3 definition stated that patients with septic shock are to be clinically identified by a vasopressor requirement to maintain a mean arterial pressure of 65 mmHg or greater and a serum lactate level >2 mmol/L in the absence of hypovolemia . The optimal cut-off point for serum lactate level to determine ICU mortality in septic shock patients seems variable across different cohorts. The 2001 International Sepsis Definitions Conference (Sepsis-2) clinically identified septic shock as a state of acute circulatory failure characterized by persistent arterial hypotension defined as a systolic arterial pressure below 90 mmHg; a mean arterial pressure below 60 mmHg, or a reduction in systolic blood pressure of more than 40 mmHg from baseline, despite adequate volume resuscitation [Citation5]. Treatment goal in the Surviving Sepsis Campaign international guidelines 2012 is a mean arterial blood pressure of higher than 65 mmHg [Citation6]. In addition, in the Sepsis-2 definition of septic shock, the level of the serum lactate has not been part of the definition. The Third ICD Task Force (Sepsis-3) demonstrated that the combination of hypotension and hyperlactatemia is associated with a significantly higher risk-adjusted ICU mortality compared to hypotension alone [Citation3]. Elevated lactate levels reflect cellular dysfunction in sepsis [Citation7]. To compare differences in epidemiology and outcome of septic shock, the effects of both definitions were studied in a septic intensive care population . In addition we assessed the effect of various cut-off values for lactate on the accuracy of the Sepsis-3 criteria for septic shock to identify patients with an actual increased risk of ICU mortality compared with septic patients not fulfilling criteria for septic shock.
Materials and methods
Setting
The study was performed at the Maastricht University Medical Centre, a tertiary care, 715 bed university hospital in the Netherlands with 18 general ICU beds, 9 cardiothoracic ICU beds, 6 high-dependency care unit beds and approximately 2500 admissions annually.
Patients
All 678 patients that were admitted to our ICUs with a diagnosis of sepsis between 1 January 2013 and 1 January 2016 were entered in a prospectively recorded database. Data on age, gender, reason for admission, co-morbidities, APACHE score, ICU mortality and in-hospital mortality were recorded. Admission with sepsis was defined as any admission to the intensive care unit clinically coded as infection and at least one organ dysfunction [Citation3]. Institutional sepsis guidelines adhere to surviving sepsis campaign guidelines including early fluid resuscitation and antimicrobial therapy. Intravascular volume replacement was guided by either clinical variables and/or pulse contour measurements (Picco©) and/or echocardiography. Norepinephrine is the vasopressor of choice to treat persistent hypotension after adequate fluid resuscitation. Norepinephrine is started when mean arterial blood pressure drops below 65 mmHg. Lactate levels were retrieved from the hospital information system. The highest lactate level within the first 24 hours after admission was used for analysis. Forty-eight patients were excluded from analysis as no lactate measurement was recorded, leaving 632 patient cases available for analysis.
Sepsis definitions
In the Sepsis-2 definition septic shock was defined as sepsis and circulatory failure (mean arterial blood pressure (MAP) < 65 mmHg (according to the treatment goal of Surviving Sepsis Campaign international guidelines 2012), norepinephrine ≥0.1 µg/kg/min). In the Sepsis-3 definition septic shock was defined as sepsis and circulatory failure (MAP <65 mmHg, norepinephrine ≥0.1 µg/kg/min) and lactate level >2 mmol/L.
Statistical analysis
ICU mortality and in-hospital mortality was calculated in patients having septic shock according to the Sepsis-3 definition and in patients having septic shock according to Sepsis-2 definition. As this resulted in two overlapping samples from a single source population no formal statistical analysis could be performed to assess the significance of the different outcomes following these two approaches. In addition throughout the entire study population cohorts were created using increasing cut-off values for serum lactate in steps of 2 mmol/L. The association between lactate levels and ICU mortality was assessed using logistic regression analysis adjusting for age, sex and comorbidity. Outcome data are presented as odds-ratios with 95% confidence intervals. All analyses were performed using SPSS version 22.0 (IBM, Armonk, NY).
Results
Population
A total of 632 patients diagnosed with sepsis between 1 January 2013 and 1 January 2016 were analyzed. Details on patient characteristics are presented in . Patients were predominantly male and 51% of patients were older than 65 years of age. Most frequent sources of infection were the lower respiratory tract (38%) and abdominal sepsis (36%). Mean APACHE II score was 25 and 39% of the septic patients were known to have an active malignancy.
Table 1. Characteristics of the study population.
Sepsis criteria and ICU mortality
482 patients (76.3%) were classified as having septic shock according to the Sepsis-2 definition with a mean APACHE II score of 26.2 (± 7.8). With addition of the criterion of serum lactate level ≥2 mmol/L, according to the Sepsis-3 definition, only 300 patients (47.4%) were classified as having septic shock with a mean APACHE II score of 27 (± 7.7) ( and ). ICU mortality was higher in patients with septic shock as classified according to the Sepsis-3 criteria than in patients classified according to the Sepsis-2 criteria (38.9 vs. 34.0%). As expected, ICU mortality was lower (20.6%) in the 150 septic patients not classified as having septic shock according to any of the two definitions. In-hospital mortality was 43% for patients classified according to Sepsis-2 criteria versus 47% for patients classified according to Sepsis-3 criteria. ICU mortality in the 173 patients meeting Sepsis-2, but not Sepsis-3 definition of septic shock, was 25.6%. No formal statistical analysis could be performed to assess the significance of the different outcomes following these two approaches because here it concerns overlapping patients from a single source population.
Table 2. Number of patients meeting the definitions for septic shock according to the Sepsis-2 and Sepsis-3 definitions and the implications for APACHE II score and ICU mortality.
Effects of active malignancy and serum lactate levels on ICU mortality
Patients with sepsis and a known active malignancy had a higher mortality (43%) than patients without an active malignancy (OR, 2.4, ). When fulfilling Sepsis-3 criteria for septic shock, ICU mortality in patients with a malignancy was 49.6% and when fulfilling Sepsis-2 criteria ICU mortality was 45%. In conclusion, ICU mortality in septic shock patients with cancer is higher than patients without an active malignancy regardless of the definition used to define septic shock.
Table 3. Association between sepsis and mortality in patients with active malignancy.
ICU mortality for patients with a serum lactate ≤2 mmol/L was 26.2% and mortality for patients with serum lactate level between 2 and 4 mmol/L was 25.0%. Following Sepsis-2 criteria, septic shock patients with a serum lactate level between 2 and 4 mmol/L did not have a significant higher ICU mortality compared to patients with a lactate level ≤2 mmol/L (OR 0.94 (0.6–1.7)), ). The same was true for patients with lactate level between 4 and 6 mmol/L (OR 0.88 (0.4–1.7)). Lactate levels ≥6 mmol/L were significantly and increasingly associated with ICU mortality, with mortality rate of 51% in patients with lactate levels between 6 and 8 mmol/L. ICU mortality reached 75.8% in the patient group having lactate levels ≥8. The association of in- hospital mortality of patients with septic shock and with blood lactate level is shown in . In- hospital mortality for lactate levels below 6 mmol/L L did not point out increased risk of dying in the hospital. The in-hospital mortality for septic shock patients with normal blood lactate levels is strikingly high (38.8%), this will be further addressed in the discussion below. We investigated the generalizability of the findings, given the high prevalence of active malignancy, by repeating the lactate analysis, leaving patients with active malignancy out of the analysis. 388 patients with sepsis and no active malignancy were identified, 301 of these patients (78%) were defined as having septic shock according to Sepsis-2 definition and 188 of the patients (48%) fulfilled Sepsis-3 criteria. Lactate levels between 2 and 4 mmol/L showed no significant increase in ICU mortality (19.8%, OR 0.96 (0.5–2.0)) and this was also seen for lactate levels between 4 and 6 mmol/L L (ICU mortality 23.3%, OR 1.49 (0.6–3.7)) ().
Table 4. Association between blood lactate level and ICU mortality in patients with septic shock defined by Sepsis-2 definition after logistic regression (age, sex and co-morbidity).
Table 5. Association between blood lactate level and in-hospital mortality in patients with septic shock defined by Sepsis-2 definition after logistic regression (age, sexand co-morbidity).
Table 6. Association between blood lactate level and ICU mortality in patients with septic shock defined by Sepsis-2 definition and no active malignancy after logistic regression (age, sexand co-morbidity) and no active malignancy.
Discussion
This study compares the recent Third International Consensus Definitions of septic shock with the Sepsis-2 definition in a population of 632 septic patients. In the present study population 76% met Sepsis-2 criteria of septic shock, whereas 47% met Sepsis-3 criteria. ICU mortality as well as in-hospital mortality was higher in patients classified according to Sepsis-3 criteria (ICU mortality 38.9%, in-hospital mortality 47.0%) compared to patients classified according to Sepsis-2 criteria (ICU mortality 34.0%, in-hospital mortality 43.0%) of septic shock. The application of the Sepsis-3 definition in the population of patients with septic shock results in the selection of a smaller but more critically ill subpopulation. These findings are supportive of the aim of the Task Force when designing the consensus definitions to reflect septic shock as a more severe illness with a much higher likelihood of death than sepsis alone. The septic shock definition according to Sepsis-3 definition differs from Sepsis-2 definition mainly by adding the criterion of serum lactate level >2 mmol/L as a marker for cellular abnormality. It is recommended by the Surviving Sepsis Campaign guidelines to obtain a serum lactate measurement within six hours of presentation for all patients with suspected sepsis or septic shock. In the present study population a lactate level ≥6 mmol/L was associated with increased mortality in septic shock patients. However no association with increased mortality was found for patients with septic shock and lactate values between 2 and 4 mmol/L and between 4 and 6 mmol/L L compared to patients with lactate values ≤2 mmol/L. ‘Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality’, stated by the Task Force in the Sepsis-3 definition on septic shock [Citation4]. However in this cohort the cellular/metabolic criterion of serum lactate level substantially increases mortality only when it rises above 6 mmol/L . The association between in-hospital mortality and blood lactate level shows a similar pattern, demonstrating that lactate levels below 6 mmol/L are not associated with increased in-hospital mortality. Striking is the high in-hospital mortality in patients with low lactate levels (< 2 mmol/L). This can be explained by the fact that a large proportion of these patients have underlying malignancy (52%) and 30% of these patients are hematologic patients. Furthermore 54% of these patients left the ICU with treatment restrictions (not to be resuscitate and/or intubate orders). Lack of association between lactate levels below 6 mmol/L and ICU and in-hospital mortality raises the question if lactate level >2 mmol/L is an accurate cut off value when defining septic shock. Similarly, Casserly et al. demonstrated the cut off value of ≥4 mmol/L for lactate in conjunction with hypotension as the only cut off statistically associated with in-hospital mortality in a group of 28,150 severe sepsis and septic shock patients from the Surviving Sepsis Campaign database [Citation8]. Intermediate serum lactate values between 2 and 4 mmol/L were associated with increased mortality, but this did not reach statistical significance in this study. Although these intermediate serum lactate values are of clinical importance because of their linear relationship with mortality [Citation9,Citation10], the primary goal of the contemporary Sepsis-3 septic shock definition is to define, recognize and treat the true high risk patient with significant higher chance of dying than with sepsis alone.
A relatively large subpopulation of the study population had an active malignancy (39%) and this was an independent risk factor for ICU mortality with an odds ratio of 2.4. There are limited epidemiologic data of cancer among septic patients. Cancer is known to be the most common comorbid medical condition in patients with sepsis and septic shock, occurring in 16.8 and 11.6% of patients, respectively [Citation11,Citation12]. Danai et al. reported higher mortality rates in a large population of 1784,445 septic patients with cancer, with a mean case fatality rate of 31.7 vs. 18.8% in non-cancer sepsis patients [Citation13]. Increased mortality in this subpopulation of septic patients may be explained due to the fact that patients are often immune compromised because of the use of chemotherapy or other immune modulating therapy.
In conclusion, the epidemiology and outcome of septic shock patients are influenced by the new Sepsis-3 definition and its application results in as a smaller but more severely ill subpopulation of septic patients compared to application of the Sepsis-2 definition. This will have influence on inclusion and outcome of clinical trials in septic shock patients.
Strength of the current study is that the study population represents a ‘true’ septic shock population with corresponding high APACHE scores and mortality rate. Furthermore mortality rates in association with varying serum lactate levels are comparable with the Surviving Sepsis Campaign database [Citation4]. A large subpopulation of 39% of septic patients had an active malignancy with increased ICU mortality, further defining our population as a more severely ill group of patients.
A limitation of the present study is its observational design and the retrospective nature of the analysis, although data were collected prospectively. Nevertheless it should be acknowledged that observational studies can provide valuable and accurate information on real life practice. Secondly, in our sepsis database, started in 2013, we applied a cut-off value of mean arterial blood pressure lower than 65 mmHg to define septic shock, following the Surviving Sepsis Campaign Guidelines in 2012. Although this differs from the 2001 Sepsis-2 definition (mean arterial blood pressure lower than 60 mmHg), there will only be a limited yield of patients with a mean arterial pressure between 60 and 65 mmHg without vasopressor. Moreover our study population is limited in the number of patients included. Furthermore an elevated serum lactate level is not specific for cellular dysfunction in sepsis and factors such as accelerated aerobic glycolysis and reduced hepatic clearance can also contribute [Citation14]. However the combination of hyperlactatemia and fluid resistant hypotension is known to identify a patient group with high mortality [Citation15].
In conclusion, patients classified according to Sepsis-3 criteria had a higher ICU mortality than patients meeting Sepsis-2 criteria. Serum lactate levels <6 mmol/L were not able to identify patients with a decreased chance of ICU survival. The lactate threshold of >2 mmol/L may be too low to point out patient with an actual increased chance of ICU and in-hospital mortality. Future prospective studies should further validate the proposed clinical criteria of septic shock and may give new insights on cut off values, as well as its generalizability to other comparable university hospitals.
Acknowledgements
The authors would like to thank Bjorn Winkens for his help with statistics.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Torio CM, Andrews RM. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011: Statistical Brief #160. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006.
- Gaieski DF, Edwards JM, Kallan MJ, et al. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41:1167–1174.
- Shankar-Hari M, Harrison DA, Rowan KM. Differences in impact of definitional elements on mortality precludes international comparisons of sepsis epidemiology-a cohort study illustrating the need for standardized reporting. Crit Care Med. 2016;44:2223–2230.
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–810.
- Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29:530–538.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228.
- Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:775–787.
- Casserly B, Phillips GS, Schorr C, et al. Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med. 2015;43:567–573.
- Mikkelsen ME, Miltiades AN, Gaieski DF, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37:1670–1677.
- Nichol AD, Egi M, Pettila V, et al. Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Crit Care. 2010;14:R25.
- Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310.
- Danai P, Martin GS. Epidemiology of sepsis: recent advances. Curr Infect Dis Rep. 2005;7:329–334.
- Danai PA, Moss M, Mannino DM, et al. The epidemiology of sepsis in patients with malignancy. Chest. 2006;129:1432–1440.
- Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014;371:2309–2319.
- Cecconi M, De Backer D, Antonelli M, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1795–1815.