Abstract
Introduction
Studies from the first pandemic wave found associations between COVID-19 hospital load and mortality. Here, we aimed to study if mortality of hospitalized COVID-19 patients was associated with the COVID-19 admission rate during a full year of the pandemic in Sweden.
Method
Observational review of all patients admitted to hospital with COVID-19 in Sweden between March 2020 and February 2021 (n = 42,017). Primary outcome was 60-day all-cause mortality related to number of COVID-19 hospital admissions per month/100,000 inhabitants. Poisson regression was used to estimate the relative risk for death by month of admission, adjusting for pre-existing factors.
Results
The overall mortality was 17.4%. Excluding March 2020, mortality was clearly correlated to the number of COVID-19 admissions per month (coefficient of correlation ρ=.96; p<.0001). After adjustment for pre-existing factors, the correlation remained significant (ρ=.75, p=.02). Patients admitted in December (high admission rate and high mortality) had more comorbidities and longer hospital stays, and patients treated in intensive care units (ICU) had longer pre-ICU hospital stays and worse respiratory status on ICU admission than those admitted in July to September (low admission rate and low mortality).
Conclusion
Mortality in hospitalized COVID-19 patients was clearly associated with the COVID-19 admission rate. Admission of healthier patients between pandemic waves and delayed ICU care during wave peaks could contribute to this pattern. The study supports measures to flatten-the-curve to reduce the number of COVID-19 patients admitted to hospital.
Introduction
Mortality in hospitalized COVID-19 patients is reported to differ substantially within and between countries [Citation1,Citation2], and over time [Citation3–6]. Increasing evidence indicates that a high number of hospitalized COVID-19 patients is associated with high mortality [Citation6–8]. Kadri et al. [Citation7] studied COVID-19 inpatients in 558 US hospitals from March to August 2020, and found that the relationship between the number of hospitalized patients and mortality was stronger in June to August than in March to May. The authors proposed additional and more recent studies on the relationship between in-hospital patient load and mortality. Thus, in the present study, we aimed to evaluate if mortality in hospitalized COVID-19 patients in Sweden was associated with admission rate up to February 2021, prior to the major emergence of SARS-CoV-2 variants of concern.
Materials and methods
Study design and participants
This was a nationwide observational cohort study of all patients hospitalized in Sweden between March 2020 and February 2021 with a discharge code for COVID-19 i.e. U07.1 or U07.2 according to the 10th International Statistical Classification of Diseases (ICD-10), and a PCR test or antigen test positive for SARS-CoV-2 14 days before to 5 days after admission. Nationwide register data on demographic factors, country of birth, care dependency, comorbidities, hospitalization, intensive care unit admission, mortality, discharge codes and SARS-CoV-2 positivity was compiled at the Swedish National Board of Health and Welfare, using the unique national personal identification number, as we have described previously [Citation3]. For the present study, we added data on disposable income, education level, and main source of income, obtained from the Swedish Longitudinal Integrated Database for Health Insurance and Labour Market Studies (LISA database) held by Statistics Sweden.
Patients were categorized as intensive care unit (ICU)-treated if admitted to ICU at any time during the hospital stay.
Outcome
The study outcome was 60-day all-cause mortality and the main exposure of interest was month of hospital admission.
Statistical analyses
Coefficient of correlation (ρ) and linear regression parameters between numbers of COVID-19 admissions per month/100,000 inhabitants and 60-day all-cause mortality for month of hospital admission and logarithm of relative risk estimates were calculated.
Relative risk (RR) for 60-day death was estimated using modified Poisson regression models with month of admission as exposure variable of interest [Citation9], using December 2020 as reference. We adjusted the estimates for age (continuous: both a linear and quadratic term), sex (categorical: male/female), Charlson Comorbidity Index (CCI; categorical: 0, 1–2, 3–4, 5+), care dependency (categorical: nursing home, homecare, neither), country of birth (categorical: Sweden, other), income quintile (categorical: by quintiles of the distribution in the total population), source of income (categorical: employed/student/caregiver, disability pension, sick pay/unemployment, retirement pension, or financial aid), education (categorical: primary school, secondary school, university/college <3 years, university/college >3 years) and health care region (North, Uppsala-Örebro, Stockholm-Gotland, West, Sout-East, South), all modelled as main effects.
We performed a stratified analysis according to ICU admission during hospital stay. Estimates for the ICU-treated strata were further adjusted for SAPS3 (linear) from the first ICU episode.
In the regression models, missing data was handled by complete case analysis. Data was complete for all variables except country of birth (<1% missing), CCI (3%), education (5%), income (2%), source of income (2%) and SAPS3 (1% missing).
In cases with sequential admissions in the National Patient Register, duration of hospital stay was defined as number of days between index admission and final discharge. A sequential admission was defined as readmission within 1 day after discharge.
Ethics
The study was approved by the Swedish Ethics Review Authority, Uppsala (Dnr 2020-04278).
Results
Altogether, 42,017 hospitalized COVID-19 patients were included, with 57% males and median age 67 years. ICU care was given to 11.5%.
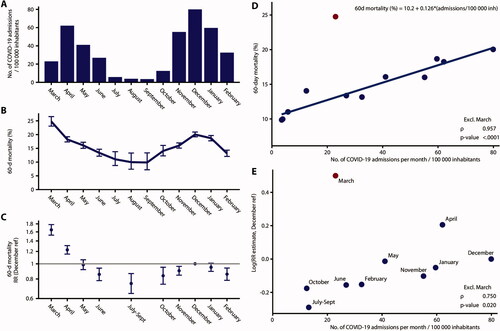
shows the number of COVID-19 admissions per month/100,000 inhabitants. The study period included two national waves, and December was the month with the highest admission rate.
Figure 1. (A) Number of COVID-19 hospital admissions per month/100,000 inhabitants in Sweden; (B) Crude 60-day all-cause mortality in hospitalized COVID-19 patients related to month of hospital admission; (C) Relative risks with 95% confidence intervals (CI) of death from any cause within 60 days after hospital admission related to month of hospital admission. The model included adjustment for sex, age (continuous, linear and quadratic terms, not shown in the plot), Charlson Comorbidity Index score, care dependency, country of birth, education, disposable income quintile, source of income and health care region. (D) Scatter plot of number of COVID-19 hospital admissions/100,000 inhabitants in Sweden (X-axis) and crude 60-day all-cause mortality in hospitalized COVID-19 patients related to month of hospital admission (Y-axis). Regression line parameters and coefficient of correlation calculated excluding March. (E) Scatter plot of number of COVID-19 hospital admissions/100,000 inhabitants in Sweden (X-axis) and logarithm of relative risk estimates of death from any cause within 60 days after hospital admission related to month of hospital admission (Y-axis). Coefficient of correlation calculated excluding March.
shows patient characteristics over time. For April, July–September, December and February, the median age was 63, 61, 71, and 66 years, the proportion of patients with no comorbidity (CCI 0) was 62, 62, 55, and 60%, and the proportion of nursing home residents was 3.7, 5.0, 8.7, and 2.7%, respectively. The proportion of patients admitted to ICU was 15.6, 8.9, 9.6, and 11.9%. Among non-ICU-treated survivors, the median length of hospital stay was 5, 4, 5, and 5 days, respectively.
Table 1. Baseline patient characteristics: as total and stratified by month of admission.
The overall 60-day mortality was 17.4%. show that the overall crude and adjusted 60-day mortality was highest in March, was low during the summer, increased during the autumn to December, and then decreased. shows that the crude mortality was clearly correlated to the number of COVID-19 admissions per month/100,000 inhabitants when March was excluded, coefficient of correlation ρ=.96; p<.0001. (With March included, the coefficient of correlation was ρ=.63; p=.029). After adjustment for pre-existing factors, the correlation remained significant when March was excluded (ρ=.75, p=.02), as seen in . The lower mortality between December and February was not seen ICU-treated patients but in non-ICU-treated patients (Supplementary Figure S1), and most clearly in nursing home residents (Supplementary Figure S2).
shows the characteristics of COVID-19 patients admitted to ICU. This group had an overall 60-day mortality of 27%. Patients admitted to hospital and treated in the ICU in April, July–September, December, and February had median hospital stays prior to ICU of 1, 1, 2, and 1 day, mean ICU admission PaO2/FiO2 ratios of 16, 18, 14, and 14 kPa, and proportions receiving invasive mechanical ventilation of 76, 51, 60, and 60%, respectively.
Table 2. Characteristics of the patient population treated on intensive care units (ICU), by month of hospital admission and survival outcome at 60 days follow-up.
Discussion
Mortality in hospitalized COVID-19 patients in Sweden varied substantially over time but was clearly associated with the COVID-19 admission rates per month between April 2020 and February 2021. These findings are concordant with studies from other countries with shorter study periods [Citation6–8]. March 2020 appeared as an outlier in our analysis, with moderately high admission rate, but with very high mortality. We speculate that the high mortality in March was probably attributed to the absolute novelty of the COVID-19 disease, with uncertainties regarding management and care, in combination with rapidly increased load of patients.
Although the reasons for the association between admission rate/load and mortality in hospitalized COVID-19 patients are unclear, the present study provides support to two potential explanations.
First, the characteristics of admitted COVID-19 patients changed over time. Those admitted in July to September had lower median age, fewer comorbidities, less likelihood of being nursing home residents and had shorter hospital stays than those admitted in December, indicating that they were healthier. Accordingly, in a Swedish study of 1,785 hospitalized geriatric COVID-19 patients [Citation10], the proportion of patients with oxygen saturation <90% on admission decreased from 13% in March 2020 to 1.4% in July 2020, in parallel to decreasing mortality. Selection of healthier COVID-19 patients for hospital care may thus be a major reason for low mortality between pandemic waves.
Second, in ICU-treated COVID-19 patients, the number of hospital days prior to ICU admission was higher and the PaO2/FiO2 ratio at ICU admission was lower in December than in July to September, indicating that ICU care may have been delayed in December. Delayed ICU admission in severely ill COVID-19 patients requiring intensive care may lead to increased mortality during wave peaks.
However, several additional factors most likely contribute to the association between admission rate and mortality. The decreasing mortality during the first wave may to some extent be due to improvements in management and care, as we have discussed previously [Citation3]. The decreasing mortality in non-ICU treated patients between December and February was probably largely due to the anti-SARS-CoV-2 vaccination which started in late December 2020 and initially focussed on nursing home residents in Sweden.
In conclusion, mortality in hospitalized COVID-19 patients was clearly associated with COVID-19 hospital admission rate, even after adjustment for pre-existing factors. This result stresses the importance of measures to flatten-the-curve [Citation11] in order to reduce the number of patients in hospital care in this pandemic, and also in future pandemics.
Supplemental Material
Download EPS Image (570.2 KB)Supplemental Material
Download EPS Image (516.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data underlying this article cannot be shared publicly due to regulations under Swedish law. According to the Swedish Ethics Review Act, the General Data Protection Regulation, and the Public Access to Information and Secrecy Act, patient data can only be made available, after legal review, to researchers who meet the criteria for access to this type of confidential data. Requests regarding data in this report may be made to the senior author.
Additional information
Funding
References
- Madahar P, Wunsch H, Jha P, et al. Trends in COVID-19-related in-hospital mortality: lessons learned from nationwide samples. Lancet Respir Med. 2021;9(4):322–324.
- Ranzani OT, Bastos LSL, Gelli JGM, et al. Characterization of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407–418.
- Strålin K, Wahlström E, Walther S, et al. Mortality trends among hospitalized COVID-19 patients in Sweden: a nationwide observational cohort study. Lancet Reg Health Eur. 2021;4:100054.
- Asch DA, Sheils NE, Islam MN, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021;181(4):471–478.
- Navaratnam AV, Gray WK, Day J, et al. Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: an observational study using administrative data. Lancet Respir Med. 2021;9(4):397–406.
- Rossman H, Meir T, Somer J, et al. Hospital load and increased COVID-19 related mortality in Israel. Nat Commun. 2021;12(1):1904.
- Kadri SS, Sun J, Lawandi A, et al. Association between caseload surge and COVID-19 survival in 558 U.S. Hospitals, march to august 2020. Ann Intern Med. 2021;6:M21–1213.
- Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US department of veterans affairs hospitals during the COVID-19 pandemic. JAMA Netw Open. 2021;4(1):e2034266.
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706.
- Xu H, Garcia-Ptacek S, Annetorp M, et al. Decreased mortality over time during the first wave in patients with COVID-19 in geriatric care: data from the Stockholm GeroCovid study. J Am Med Dir Assoc. 2021;22(8):1565–1573.e4.
- Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates- an ecological analysis of 65 countries. J Infect. 2020;81(1):e98–e99.
