Abstract
Background
The aim of this study was to compare the outcome of coronavirus disease 2019 (COVID-19) in hospitalised patients with chronic obstructive pulmonary disease (COPD) with the outcome in matched COVID-19 patients without COPD.
Methods
Sixty-three COPD patients hospitalised for acute COVID-19 from March through August 2020 were retrospectively identified and 63 hospitalised COVID-19 patients without COPD were selected and matched for age, gender and month of hospital admission.
Results
COPD patients had a higher rate of comorbidities, especially cardiovascular disease, and a trend towards a higher 30-day mortality than control patients (35% vs. 22%). In the COPD group, high Charlson comorbidity index (p = 0.03) and previous cerebrovascular disease (p = 0.04) were associated with 30-day mortality in univariate analysis. Inhaled corticosteroids maintenance therapy was not associated with lower mortality.
Conclusion
COPD patients hospitalised for acute COVID-19 disease had significantly more comorbidities and a high risk of severe outcome and death within 30 days. Comorbidity, especially cardiovascular diseases, was associated with mortality among COPD patients.
Introduction
Various comorbidities are associated with severe disease and an increased risk of death in coronavirus disease 2019 (COVID-19) [Citation1]. Globally, chronic obstructive pulmonary disease (COPD) was the third most common cause of mortality prior to the pandemic [Citation2]. The frequency of acute exacerbations of COPD is associated with disease progression, impaired pulmonary function and mortality in COPD patients [Citation3,Citation4]. Exacerbations are commonly associated with viral infections, typically caused by agents like human rhinovirus, respiratory syncytial virus and influenza virus [Citation5].
Increased expression of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) receptor ACE-2 in the lung epithelium in patients with COPD has been reported [Citation6,Citation7]. In line with this, COPD has been identified as a risk factor for severe disease and increased mortality in COVID-19 patients [Citation8,Citation9]. However, most original studies have not focussed explicitly on COPD patients, introducing a risk of confounding bias. Inhalation corticosteroid maintenance therapy, in combination with a long-acting β2 adrenergic receptor agonist, is well-documented as prevention of acute exacerbations in COPD patients [Citation10]. Early in the pandemic, it was noticed that chronic pulmonary conditions were underrepresented among patients admitted to hospital. This gave rise to speculations on whether inhaled corticosteroid therapy for these conditions could have a protective effect against severe SARS-CoV-2 infection [Citation11].
The aim of this study was to investigate the outcome of SARS-CoV-2 infection in hospitalised patients with COPD compared with a matched control group of patients with COVID-19 without COPD.
Material and methods
Study population and design
We conducted a retrospective study based on data from medical records retrieved from Sahlgrenska University hospital, a 1700-bed teaching hospital in Western Sweden with a catchment area of approximately 700,000 inhabitants. All patients with a diagnosis of COPD and COVID-19 from March through August 2020 were selected by extracting ICD-10 codes from the hospital patient administration system. A matched control population of hospitalised patients with COVID-19 but without COPD, during the same period, was identified using the same administrative system. Matching of control subjects was conducted rigorously from a list of all hospitalised COVID-19 patients sorted by date of admission, with extracted data on age and gender. Subjects were matched in the following order: (i) gender (absolute criterion), (ii) month of admission or of positive test for SARS-CoV2 infection obtained at the hospital (± one month) and (iii) age (± one year).
Inclusion criteria for COPD patients with Covid-19 were a registered ICD-10 code for COPD (J44.9 or J44.1) and an ICD-10 code for COVID-19 (U07.1) upon discharge. For non-COPD control subjects, inclusion criterion was an ICD-10 code for COVID-19. The diagnosis of COVID-19 was confirmed by PCR testing in all cases.
Exclusion criteria for both groups: (i) symptoms and/or clinical evidence compatible with other diagnoses than COVID-19 during hospital stay and prior laboratory confirmed COVID-19 more than three weeks before hospital admission, (ii) positive SARS-CoV-2 PCR with a CT-value >35 with symptoms and/or clinical evidence compatible with other diagnosis and (iii) positive SARS-CoV-2 screening test by PCR during hospital stay with another primary diagnosis and without relevant COVID-19 symptoms. Patients with uncertain COPD diagnosis according to medical records were excluded.
Data on sex, age, comorbidities, clinical data and outcome variables were retrieved from medical records. Information about time of death was collected from The Swedish Cause of Death Register. Body mass index (BMI), length of hospital stay, 30-day mortality and Charlson comorbidity index were calculated for all patients [Citation12]. Modified Charlson comorbidity index was defined as a reduction of the score by one point for chronic pulmonary disease for patients with COPD. Severity of COVID-19 was classified at discharge by the WHO Clinical Progression Scale for COVID-19 and used as an outcome variable [Citation13]. Severe disease was defined as WHO scale ≥6.
Ethical considerations
The study was approved by the National Ethical Review Board (Etikprövningsmyndigheten Dnr 2019-05916, 2020-01771). Data were recorded and presented in a way that did not permit identification of individuals and retrospective informed consent was not required.
Statistical analysis
Statistical analyses were made using the JMP software package, version 15 (SAS Inc., Cary, NC). Study and control subjects were compared using cross-tabulation, Chi-square test and Fisher’s exact test for categorical variables, as appropriate. Mann–Whitney U-test was used for continuous dependent variables. Analyses of outcome in all patients (with and without COVID-19) and of mortality in COPD patients were made using Chi-square test, Fisher’s exact test and logistic regression.
Results
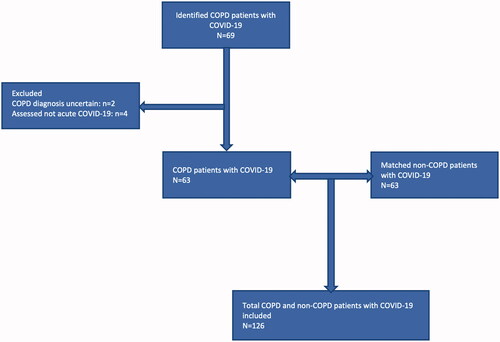
Sixty-three COPD patients with COVID-19 and 63 matched non-COPD patients with COVID-19 were included in the study. A flow-chart of the study design is presented in .
Figure 1. Flow-chart of the selection process of the study group consisting of 63 hospitalised patients with COPD and COVID-19 and a matched control population of 63 patients with COVID-19 without COPD. COPD: chronic obstructive pulmonary disease; COVID-19: coronavirus 2019 disease.
Patient background characteristics are shown in . Median age was 75 years and a majority of the subjects were women (60.3%). The proportion of former and current smoking was higher in the COPD-group. The rates of cardiovascular disease and Charlson comborbidity index score were higher in COPD patients. In the COPD group, 35 patients (56%) had inhaled corticosteroid treatment prior to admission. Only four patients (6%) were on inhaled corticosteroid treatment for asthma in the non-COPD group.
Table 1. Characteristics of 63 hospitalised COPD patients with COVID-19 and 63 matched COVID-19 patients without COPD.
shows the comparison of outcome between COPD and non-COPD patients. There was no significant difference in progression to severe disease, defined as WHO scale grade 6–10 (advanced care and/or death). There was a trend towards higher mortality in the COPD group (35% vs. 22%, p = 0.115). The rates of ICU admission and use of mechanical ventilation were lower in the COPD group than in non-COPD patients but the differences were not statistically significant. At presentation, COPD patients had a lower rate of fever and lower oxygen saturation level, whereas other clinical variables, e.g. CRP levels or lymphocyte count did not differ between groups (data not shown).
Table 2. Outcome of 63 COPD patients and 63 matched non-COPD patients hospitalised with COVID-19.
Age (p = 0.008), chronic heart disease (p = 0.013), cerebrovascular disease (p = 0.027) and dementia (p = 0.006) were associated with mortality in univariate analysis among all patients (with and without COPD). In multivariate analysis, only dementia (p = 0.012; OR = 3.85) and chronic heart disease (p = 0.020; OR = 2.71) remained independently associated with mortality. The only factor associated with ICU admission was male sex (p = 0.046), which remained predictive in multivariate analysis (p = 0.046; OR = 2.99). There were no significant associations between patient characteristics and need for mechanical ventilation or length of hospital stay.
shows analysis of factors associated with increased mortality in the group of COPD patients. Modified Charlson comorbidity index score (p = 0.03) and cerebrovascular disease (p = 0.04) were significantly associated with 30-day mortality in univariate analysis. A trend towards increased mortality was observed for COPD patients on inhaled corticosteroid therapy, 40% (14/35) versus 29% (8/28), p = 0.34.
Table 3. Factors associated with mortality in 63 COPD patients with COVID-19.
Discussion
We performed a retrospective study comparing outcome of acute COVID-19 in hospitalised patients with and without COPD. Our results indicate that comorbidities were more common in hospitalised COPD patients than in the matched control group and that COPD patients had a trend towards higher mortality within 30 days. The difference in mortality (35% vs. 22%) may be clinically relevant although not statistically significant in this study. Also, in COPD patients, high comorbidity index and cerebrovascular disease were associated with increased mortality. Ongoing maintenance therapy with inhaled corticosteroids in COPD patients did not seem to prevent progression to severe COVID-19 or death. Contradictory results regarding the role of inhaled corticosteroid maintenance therapy in COPD patients with COVID-19 were found in two large studies, one with higher mortality in COPD patients on inhaled corticosteroids and another with no difference in mortality [Citation14,Citation15].
Thus, COPD patients hospitalised due to COVID-19 seem to be at risk of severe disease, either due to compromised pulmonary function or due to significant comorbidity. The COPD patients in this report had higher mortality but a lower rate of mechanical ventilation than non-COPD patients. The average mortality within 60 days in Swedish hospitalised COVID-19 patients from March to September 2020 was 17.2% of more than 17,000 patients with a median age of 64 years in a nation-wide observational study [Citation16]. In our study, the 30-day mortality was 34.9% in COPD-patients, although with a higher median age (75 years), suggesting that COPD patients may be at higher risk of severe outcome. Indeed, more severe disease and higher mortality in COPD patients with COVID-19 have been confirmed in several reports [Citation17–19]. Thus, the trend towards higher mortality in COPD patients in our study is in agreement with the current literature. However, the difference in hospital mortality could to some extent be explained by a higher degree of associated cardiovascular disease as implicated in our study.
The COPD patients in this study had a lower rate of mechanical ventilation. This might reflect that COPD patients may not have been eligible for mechanical ventilation, due to expected poor outcome of such therapy. A lower rate of mechanical ventilation in COPD patients with COVID-19 was also seen in a large prospective study from Great Britain [Citation14]. Varying results in different reports may reflect variations in clinical practice regarding the indication for invasive ventilation in COPD-patients.
The strength of this study is its primary focus on COPD patients and the strictly age- and gender-matched control group, providing basic adjustment for confounding bias and giving insights into the nature of the difference in characteristics between COVID-19 patients with and without COPD. The first and major limitation is the small sample size, which does not provide sufficient power for significant conclusions regarding disease severity and outcome. Second, we had incomplete data on grading of COPD severity by the GOLD classification, making comparisons of COPD outcome based on pulmonary function and degree of symptoms difficult. Third, there were missing patient characteristics data and incomplete data on reasons for clinical decisions regarding ICU admission and/or indication for mechanical ventilation.
In conclusion, COPD patients hospitalised for acute COVID-19 had significant comorbidity and a high risk of severe disease and death within 30 days. Comorbidity, especially cardiovascular diseases, was associated with mortality among COPD patients.
Acknowledgements
The authors thank Johanna Petersson Viir for assistance with data extraction.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436.
- Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. The Lancet. 2018;392(10159):1736–1788.
- Halpin DM, Decramer M, Celli B, et al. Exacerbation frequency and course of COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:653–661.
- Soler-Cataluna JJ, Martinez-Garcia MA, Roman Sanchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931.
- Linden D, Guo-Parke H, Coyle PV, et al. Respiratory viral infection: a potential "missing link" in the pathogenesis of COPD. Eur Respir Rev. 2019;28(151):180063.
- Leung JM, Yang CX, Tam A, et al. ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur Respir J. 2020;55(5):2000688.
- Higham A, Mathioudakis A, Vestbo J, et al. COVID-19 and COPD: a narrative review of the basic science and clinical outcomes. Eur Respir Rev. 2020;29(158):200199.
- Xiao WW, Xu J, Shi L, et al. Is chronic obstructive pulmonary disease an independent predictor for adverse outcomes in coronavirus disease 2019 patients? Eur Rev Med Pharmacol Sci. 2020;24(21):11421–11427.
- Lippi G, Henry BM. Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19). Respir Med. 2020;167:105941.
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582.
- Halpin DMG, Faner R, Sibila O, et al. Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection? Lancet Respir Med. 2020;8(5):436–438.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020;20(8):e192–e7.
- Bloom CI, Drake TM, Docherty AB, et al. Risk of adverse outcomes in patients with underlying respiratory conditions admitted to hospital with COVID-19: a national, multicentre prospective cohort study using the ISARIC WHO clinical characterisation protocol UK. Lancet Respir Med. 2021;9(7):699–711.
- Schultze A, OpenSAFELY Collaborative, Walker AJ, MacKenna B, Morton CE, Bhaskaran K, Brown JP, et al. Risk of COVID-19-related death among patients with chronic obstructive pulmonary disease or asthma prescribed inhaled corticosteroids: an observational cohort study using the OpenSAFELY platform. Lancet Respir Med. 2020;8(11):1106–1120.
- Strålin K, Wahlström E, Walther S, et al. Mortality trends among hospitalised COVID-19 patients in Sweden: a nationwide observational cohort study. Lancet Reg Health Eur. 2021;4:100054.
- Rabbani G, Shariful Islam SM, Rahman MA, et al. Pre-existing COPD is associated with an increased risk of mortality and severity in COVID-19: a rapid systematic review and Meta-analysis. Expert Rev Respir Med. 2021;15(5):705–716.
- Dorjee K, Kim H, Bonomo E, et al. Prevalence and predictors of death and severe disease in patients hospitalized due to COVID-19: a comprehensive systematic review and Meta-analysis of 77 studies and 38,000 patients. PLoS One. 2020;15(12):e0243191.
- Izcovich A, Ragusa MA, Tortosa F, et al. Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review. PLoS One. 2020;15(11):e0241955.
