Abstract
Introduction
long term suppressive antibiotic treatment may be the only feasible option for patients with infective endocarditis (IE) not suitable for surgery.
Case reports
we present three cases of prosthetic valve endocarditis (PVE) caused by Enterococcus faecalis and Streptococcus gallolyticus which could not undergo surgical intervention due to high risk. Despite this, patients were successfully managed only by medical approach. Following intravenous targeted antimicrobial therapy, patients received chronic suppressive antimicrobial therapy (SAT) for at least twelve months with oral amoxicillin. In all cases, no further febrile episodes nor bacteraemia were observed and in two cases a complete positron emission tomography (PET) response was achieved. Due to a priori uncertainty about antimicrobial exposure during oral SAT, serum bactericidal titres (SBTs) were obtained and compared to those obtained during parenteral therapy.
Conclusions
long term oral amoxicillin was effective and well-tolerated. SBTs after switch to oral therapy were quite heterogeneous, in some cases not reaching the conventionally established titre to assess bactericidal effect (1:8).
endovascular infection in non-suitable-for-surgery patients can be managed with long-term oral suppressive therapy.
serum bactericidal assay confirmed high effectiveness of parenteral antibiotic therapy.
serum bactericidal assay showed highly variable titres during oral therapy.
Key points
Background
Infective Endocarditis (IE) is a potentially life threatening and difficult-to-treat-infection [Citation1] and its management includes prolonged antibiotic course and surgical approach [Citation2] in case of extensive valvular lesion, vegetation size and prosthetic valve disfunction.
In the last years, the epidemiology of IE has changed, shifting to more aged and frail patients with multiple comorbidities, prosthetic valves and implantable devices [Citation3].
Since for such cases surgical removal of infected prosthetic material is often unsuitable due to unfavourable risk-benefit balance, long-term suppressive antibiotic treatment (SAT) seems to be the only feasible option [Citation4]. Early switch to oral antibiotic has been proved to be a safe and effective strategy in stable left-sided endocarditis [Citation5], but clinical outcomes of patients treated with long-term oral SAT has been described only in case reports and small series [Citation6–8].
Given the lack of standard management for such situations and their potentially increasing incidence in clinical practice, we hereby describe three cases of prosthetic valve endocarditis (PVE) for whom surgical approach was considered inappropriate, receiving long-term SAT.
To evaluate PK/PD target attainment of the treatment we measured paired serum bactericidal titres (SBTs) during initial intravenous (i.v.) therapy and after switching to oral therapy.
Case 1
The first case we present is a 72-year-old female. She had a history of biological aortic graft implantation in December 2019 (Bentall procedure), complicated by inflammatory collection around aortic root and a hospital admission in February 2021 for Enterococcus faecalis sepsis. At the time, Positron emission tomography (PET) scan showed diffuse uptake involving proximal ascendent aorta and anterior mediastinum. She was treated with vancomycin for five weeks and a colonoscopy was performed allowing a big polypus detection and removal. She had also chronic kidney disease (KDIGO IV stage), atrial fibrillation and arterial hypertension.
She presented in May 2021 to the emergency department (ED) of our hospital due to relapsing E. faecalis bacteraemia. A TOE showed vegetations adhering to prosthetic aortic valve cuspids as long as atrial septum thickening and pathologic tissue extending to the entire ascending aorta graft. Antimicrobial therapy was started with ampicillin (dosage adjusted for renal function) and ceftriaxone. A surgical approach was considered not suitable due to high surgical risk. A chest CT scan showed fluid collection in subcutaneous tissue above sternal manubrium. SBT performed during intravenous therapy showed high bactericidal titres (); blood cultures resulted negative by day three of admission and subsequent TOE (on day 23) documented disappearance of valvular vegetation. After six weeks of parenteral antibiotic therapy, the patient was discharged on oral linezolid (600 mg bid) for two additional weeks. A follow-up PET showed signs of uncontrolled infection involving aortic root, ascending aorta and anterior mediastinum soft tissues; SAT with oral amoxicillin according to renal function (1 g bid) was preferred to linezolid due to better safety profile. Follow-up blood cultures and TOE were persistently negative for relapse of bacteraemia or endocarditis. After eight months, a PET-CT scan showed a strong reduction of the pathologic enhancement (). SBT repeated after switching to oral amoxicillin revealed decreased bactericidal titres (). After more than fifteen months the patient is still on long-term suppressive antibiotic therapy to prevent further bacteraemia from a newly discovered colon carcinoma, which is undergoing adjuvant chemotherapy.
Figure 1. Case 1 PET-CT scan performed after 8 weeks of therapy is displayed in the upper part of the figure, showing focal increased uptake surrounding the aortic valve. In the lower part, follow-up PET CT after 8 months of SAT shows reduction of the uptake.
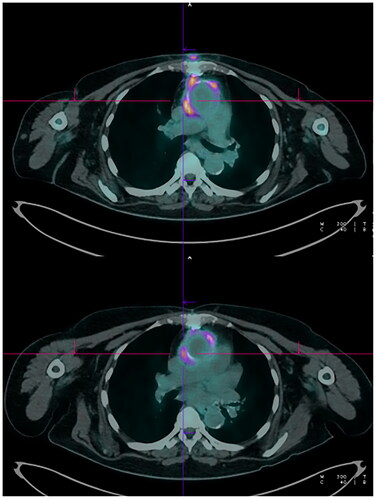
Table 1. Summary of clinical and microbiological characteristics.
Case 2
A 72-year-old male presented to the ED of our hospital in May 2021 due to persistent fever.
He previously underwent ascending aorta substitution, abdominal aorta aneurysm (AAA) repair, ascending aorta grafting (Elephant trunk procedure), aortic valve substitution (Bentall procedure) and endovascular thoracic aorta grafting due to Marfan syndrome.
Other relevant medical conditions included type II diabetes, arterial hypertension, thalassaemia minor and a previous trans-urethral resection of the bladder (TURB) for a neoplasm. Blood cultures and TOE revealed mechanical aortic PVE caused by Streptococcus gallolyticus and therapy with ceftriaxone (2 g bid) was started. Colonoscopy revealed a polypus as the probable source of infection. PET-CT scan showed enhanced metabolism involving the prosthetic material up to the thoracic aorta, while the vegetation was cleared at a follow-up TOE and subsequent blood cultures resulted negative. Surgical intervention aimed to obtain infection control was considered not feasible. A follow-up CT scan showed progression of AAA, therefore the patient underwent endovascular exclusion through Candy plug technique after six weeks of antibiotic treatment. He was discharged on long-term SAT with oral amoxicillin 1 g tid. He remained afebrile with persistently negative blood cultures and paired SBTs showed good bactericidal activity (). One year after the discharge, PET scan revealed absence of visible uptake along prosthetic material and antibiotic therapy was stopped without further relapses.
Case 3
The third case is a 78-year-old male who previously underwent aorto-coronary bypass, aortic valve substitution (biological prosthesis) and cardiac pacemaker (PM) implantation due to severe coronary artery disease, severe aortic stenosis and sinus-atrial and left branch bundle block. Other relevant medical conditions included hypertension and colon diverticulosis. He had three subsequent bacteraemia episodes caused by E. faecalis in May 2020 (treated with ampicillin, negative transthoracic echocardiogram for endocarditis), August 2020 (treated with ampicillin/ceftriaxone, complicated by prosthetic endocarditis) and in October 2020 (treated with fosfomycin, ampicillin and ceftriaxone for PVE). During this last episode, surgical reintervention was excluded due to lack of prosthetic disfunction and high surgical risk. He presented in December 2020 for relapsing E. faecalis bacteraemia 20 d after antibiotic discontinuation: a TOE confirmed relapse of IE (vegetation size < 5 mm) and linezolid (600 mg bid) therapy was started. Soon after the patient was discharged on linezolid and amoxicillin (1 g tid) SAT. Four weeks later PET scan was negative for prosthetic valve or PM pathologic uptake and linezolid was stopped but oral amoxicillin was maintained as an attempt of preventing further relapses. SBT performed on oral amoxicillin showed suboptimal bactericidal activity (), but the patient remained afebrile, monthly blood cultures were negative and one year after SAT was discontinued. He is still going well.
Discussion
Long-term suppressive antimicrobial therapy (SAT) with amoxicillin allowed to achieve a clinical and radiological improvement without microbiological relapse in three cases of PVE in whom source control through surgical intervention was deemed inappropriate due to elevated surgical risk and/or technical unfeasibility and absence of severe valve disfunction.
Side effects due to amoxicillin were negligible. In two out of three patients, treatment was stopped guided by resolution of PET signs of infection, similarly to what has been previously described in other series [Citation6, Citation9].
Patients with a prosthetic infection unsuitable for surgery often need to be treated with a long-lasting antimicrobial treatment, and the concern about tolerability and safety remain pivotal in the management as well as efficacy. Therefore, the prescription of an antimicrobial regimen which is both well tolerated and effective remains crucial, despite the absence of clinical trial addressing this issue.
Data on long-term treatment with amoxicillin for E. faecalis PVE are few [Citation6]. A trial for partially oral therapy for penicillin-susceptible streptococcal native valve IE conducted by Stamboulian et al. in 10 patients treated with oral amoxicillin (1 g q6h) showed a peak SBTs >1:8 and clinical cure [Citation10]. Oral absorption of amoxicillin is saturable, resulting in a nonlinear increase in Cmax with dosage. Therefore, lower doses administered with a reduced interval are as effective as higher doses but with lower risk of adverse events [Citation11].
We evaluated SBT in these patients since it has been extensively used for monitoring efficacy of IE therapy in the past and should ensure the theoretical advantage of combining in an easy-to-read result many factors involved in treatment success such as host humoral defences, susceptibility of the bacterial strain, changing antibiotic concentrations during dosing interval and drug-drug PD interactions [Citation12]. SBTs were obtained both during parenteral antibiotic therapy (among day 5 and day and 21) and on prolonged oral antibiotic therapy (after 6 months of therapy).
In each case initial parenteral therapy demonstrated a killing effect of patient sera during the whole dosing interval highly above SBTs critical values of ≥1:8 for peak levels and ≥ 1/2 for trough levels, consistent with a minimal 40% drug time above MIC () [Citation12, Citation13].
SBT was performed according to in-home methods: a standardised inoculum of the patient’s isolate is prepared into a tube containing 5.0 mL of Mueller–Hinton broth either directly from colonies of a single type or from an overnight pure culture. The bacterial suspension is then incubated for 18 h at 35 °C. The turbidity of growing broth culture is adjusted to obtain a turbidity visually comparable to that of a 0.5 McFarland turbidity standard. The adjusted culture is then diluted in broth so that after inoculation, each well will contain approximately 5 × l0 s CFU/mL. At this moment, 0.05 mL of the bacterial dilution are added to each well. The microtitre plate is then incubated at 35 °C for 18–24 h. After incubation, the inhibitory titre is defined as the highest dilution that prevented visual turbidity. To assess the bactericidal activity, 10 µL are removed from each clear well, plated onto Mueller–Hinton agar and incubated at 35 °C for 18 h. The serum bactericidal titre is defined as the highest dilution that resulted in ≥ 99.9% killing of the starting inoculum. Antimicrobial susceptibility tests on isolates from positive blood cultures were performed according to manufacturer instructions (Phoenix 100™ system (BD Dickinson and Company, Franklin Lakes, NJ).
We expected these values as IE treatment schemes are intended to ensure a high exposure to antibiotics [Citation14]. On the other hand, SBTs during oral antibiotic therapy are heterogeneous as shown in .
The most cumbersome result of SBT in our series is Case 3 because both peak and through SBTs were = < 1:2, far below the 1:8 threshold. Despite that, it was decided not to change the antibiotic regimen due to the good clinical and microbiologic.
How to ‘save the phenomena’? It’s possible that previous parenteral combination antibiotic courses managed to reduce bacterial burden, making relatively low concentrations of amoxicillin to achieve a good clinical result as is suggested by Gatti et al. reporting in 10 of 11 patients with E. faecalis BSI or IE the opportunity to reduce by 50% the initial dose of iv ampicillin using TDM [Citation15]. Therefore, in the SAT phase clinical success may be achieved despite SBTs several times lower compared to that obtained with parenteral therapy. This is supported by PK/PD models of amoxicillin in enterococcal infections, showing a discrete probability of achieving bactericidal effect (T > MIC 40%) even at low dosages [Citation16], particularly when MICs for beta lactams are low, as in our cases (). Consequently, lower threshold to establish bactericidal effect of long-term oral suppressive therapy may be needed.
Furthermore, in this case the possibility of a false negative PET result after four weeks of antibiotic treatment should be considered.
In conclusion, our experience supports the use of amoxicillin as single drug long-term SAT in patients with endovascular infections unsuitable for surgery. Further robust and possibly prospectively collected data are needed to evaluate the outcomes relative to length and tolerability of antimicrobial therapy in patients with prosthetic valve infection that are not candidate to surgery. SBTs could be used in these patients to evaluate efficacy of SAT, in the absence of standard therapeutic schemes.
Acknowledgements
Authors contributed equally to ideation, data collection and interpretation and to the writing of the article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Holland TL, Baddour LM, Bayer AS, et al. Infective endocarditis HHS public access. Nat Rev Dis Primers. 2017;2:1–49.
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis. Eur Heart J. 2015;36(44):3075–3128.
- Fernández-Hidalgo N, Almirante B. Estado actual de la endocarditis infecciosa: nuevas poblaciones de riesgo, nuevos retos diagnósticos y terapéuticos. Enferm Infecc Microbiol Clin. 2018;36(2):69–71.
- Utili R, Durante-Mangoni E, Tripodi MF. Infection of intravascular prostheses: how to treat other than surgery. Int J Antimicrob Agents. 2007;30(1):42–50.
- Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med. 2019;380(5):415–424.
- Camazon NV, Mateu L, Cediel G, et al. Long-term antibiotic therapy in patients with surgery-indicated not undergoing surgery infective endocarditis. Cardiol J. 2021;28(4):566–578.
- Baddour LM. Long-term suppressive antimicrobial therapy for intravascular device-related infections. Am J Med Sci. 2001;322(4):209–212.
- Tan EM, DeSimone DC, Sohail MR, et al. Outcomes in patients with cardiovascular implantable electronic device infection managed With chronic antibiotic suppression. Clin Infect Dis. 2017;64(11):1516–1521.
- Puerta-Alcalde P, Cuervo G, Simonetti AF, et al. PET/CT added to Duke criteria facilitates diagnosis and monitoring of long-term suppressive therapy of prosthetic endocarditis. Infect Dis (Lond). 2017;49(9):698–701.
- Stamboulian D, Bonvehi P, Arevalo C, et al. Antibiotic management of outpatients with endocarditis due to Penicillin-Susceptible streptococci. Rev Infect Dis. 1991;13(2):13.
- de Velde F, de Winter BCM, Koch BCP, et al. Non-linear absorption pharmacokinetics of amoxicillin: consequences for dosing regimens and clinical breakpoints. J Antimicrob Chemother. 2016;71(10):2909–2917.
- Stratton CW. Serum bactericidal test. Clin Microbiol Rev. 1988;1:19–26.
- Zaghi I, Gaibani P, Campoli C, et al. Serum bactericidal titres for monitoring antimicrobial therapy: current status and potential role in the management of multidrug-resistant gram-negative infections. Clin Microbiol Infect. 2020;26(10):1338–1344.
- Macheda G, el Helali N, Péan de Ponfilly G, et al. Impact of therapeutic drug monitoring of antibiotics in the management of infective endocarditis. Eur J Clin Microbiol Infect Dis. 2022;41(9):1183–1190.
- Gatti M, Tedeschi S, Trapani F, et al. A proof of concept of the usefulness of a TDM-Guided strategy for optimizing pharmacokinetic/pharmacodynamic target of continuous infusion Ampicillin-Based regimens in a case series of patients with enterococcal bloodstream infections and/or endocarditis. Antibiotics. 2022;11(8):1037.
- Jimenez-Toro I, Rodriguez CA, Zuluaga AF, et al. A new pharmacodynamic approach to study antibiotic combinations against enterococci in vivo: application to ampicillin plus ceftriaxone. PLoS One. 2020;15(12):e0243365.
