Abstract
Background
The World Health Organization has adopted a resolution on sepsis and urged member states to develop national processes to improve sepsis care. In Sweden, sepsis was selected as one of the ten first diagnoses to be addressed, when the Swedish government in 2019 allocated funds for patient-centred clinical pathways in healthcare. A national multidisciplinary working group, including a patient representative, was appointed to develop the patient-centred clinical pathway for sepsis.
Methods
The working group mapped challenges and needs surrounding sepsis care and included a survey sent to all emergency departments (ED) in Sweden, and then designed a patient-centred clinical pathway for sepsis.
Results
The working group decided to focus on the following four areas: (1) sepsis alert for early detection and management optimisation for the most severely ill sepsis patients in the ED; (2) accurate sepsis diagnosis coding; (3) structured information to patients at discharge after sepsis care and (4) structured telephone follow-up after sepsis care. A health-economic analysis indicated that the implementation of the clinical pathway for sepsis will most likely not drive costs. An important aspect of the clinical pathway is implementing continuous monitoring of performance and process indicators. A national working group is currently building up such a system for monitoring, focusing on extraction of this information from the electronic health records systems.
Conclusion
A national patient-centred clinical pathway for sepsis has been developed and is currently being implemented in Swedish healthcare. We believe that the clinical pathway and the accompanying monitoring will provide a more efficient and equal sepsis care and improved possibilities to monitor and further develop sepsis care in Sweden.
Introduction
In 2017, the World Health Organization (WHO) recognised sepsis as a Global Health Priority and adopted a resolution on improving the prevention, diagnosis and management of sepsis [Citation1]. Sepsis is a condition of impaired organ function caused by an infection [Citation2,Citation3] which in Sweden is reported to have an incidence of at least 500/100,000 individuals per year [Citation4,Citation5]. Hospital mortality for sepsis in Sweden has been reported to be around 17% [Citation4].
Patients with sepsis are identified in all areas of healthcare. Most patients develop sepsis outside of hospital, but sepsis is usually detected in the emergency department (ED) or in other inpatient settings. More than half of the patients with sepsis arrive to the hospital by ambulance, a factor typically linked to severity.
Since 2019 the Swedish government has allocated €90,000,000 for patient-centred clinical pathways targeting major diagnoses in Sweden, with the overall intention to achieve equality and effectiveness of care. The WHO sepsis resolution was part of the basis for selecting sepsis as one of the ten first diagnoses to be addressed within this project. The National Program Groups for Infectious Diseases and Emergency Care of the National System for Knowledge-Driven Management within Swedish Healthcare have led the process to develop the patient-centred clinical pathway for sepsis, and in 2019, they appointed a national multi-disciplinary and multi-professional working group (including a patient representative), who developed the clinical pathway.
On 21 May 2021, the Steering Committee of the National System for Knowledge-Driven Management within Swedish Healthcare approved the patient-centred clinical pathway for sepsis, for implementation throughout Swedish healthcare [Citation6,Citation7].
This article is a translation from Swedish [Citation6] of the patient-centred clinical pathway for sepsis, with slightly updated information.
Working process
The national working group consisted of representatives from the six Swedish healthcare regions, and the following areas of expertise were covered: Infectious diseases, Emergency medicine including pre-hospital care, Internal medicine, Primary care, Anaesthesiology and intensive care, Surgery and Clinical microbiology. In addition, a patient representative was included in the working group. All working group participants had provided a declaration of conflict of interests prior to the work.
The group held several meetings between October 2019 and January 2020, during which the clinical pathway was designed. In January–March 2020, the clinical pathway was circulated nationally for commenting, whereby suggestions for improvement were received. Revisions based on the suggestions for improvement were made through multiple digital meetings between August 2020 and March 2021. In May 2021, the clinical pathway was approved for implementation throughout Swedish healthcare.
During the work process, the preliminary design of the clinical pathway was repeatedly presented to the National Program Groups for Infectious Diseases and Emergency Care and to the Sepsis group of the Swedish Society of Infectious Diseases, who were revising the Swedish Sepsis recommendations at the time [Citation8]. The parts of the clinical pathway involving information to patients at discharge and patient follow-up were discussed with the Swedish trust Sepsisfonden [Citation9].
Challenges and needs within sepsis care
The working group started its work by describing a typical pathway for a patient with sepsis starting at home and describing challenges and needs surrounding sepsis care (see ). The patient representative’s perspective was important for the design and contents of this description.
Figure 1. Graphic presentation of current common experiences of healthcare for people with sepsis and challenges and needs for sepsis care.
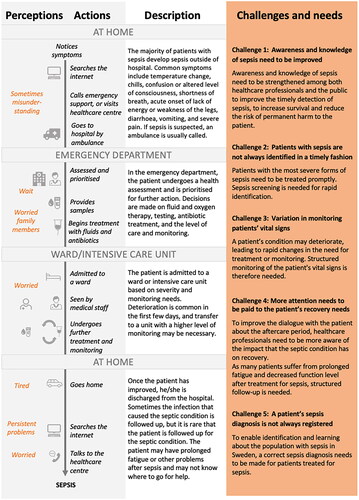
Challenge 1: awareness and knowledge of sepsis need to be improved
There is a need for increasing the awareness and knowledge of sepsis among both healthcare professionals and the public. It should be noted that Sepsisfonden [Citation9] is continuously working for improvement of knowledge of sepsis in the general public.
Challenge 2: patients with sepsis are not always identified in a timely fashion
Evidence supports that rapid intervention is important for survival for the most severely ill sepsis patients, those with septic shock [Citation10,Citation11]. However, even for severely ill patients without septic shock, prompt action can have an impact on outcome [Citation12]. A clear structure for the initial management of the most severely ill patients with sepsis is therefore needed to achieve a consistent quality of care.
In the end of 2019, a survey was sent to the EDs in Sweden regarding their sepsis care. Of 63 responding EDs (in 19 of the 21 Swedish regions), 33 EDs (53%) reported that they had an ongoing sepsis screening and management system with sepsis alert or sepsis track, and 21 EDs (33%) reported that they performed continuous surveillance of patients with sepsis. This survey illustrated current variations of sepsis care at Swedish EDs.
Challenge 3: variation in monitoring patients’ vital signs
Over the past years, the National Early Warning Score 2 (NEWS2) [Citation13] has become broadly implemented for monitoring in Swedish hospitals during in-hospital care, and thus, monitoring of the patients’ vital signs has been improved.
Challenge 4: more attention needs to be paid to the patient’s recovery needs
Many patients experience prolonged fatigue or decreased or impaired functional level after hospitalisation for sepsis [Citation1,Citation14], which has not been recognised among both healthcare professionals and the public. Structured follow-up measures are needed to improve this aspect of sepsis care [Citation15].
Challenge 5: a patient’s sepsis diagnosis is not always registered
Studies have shown that < 20% of patients who fulfil the sepsis criteria receive a sepsis discharge diagnosis code in Sweden [Citation4,Citation16,Citation17]. Thus, the burden of sepsis within Swedish healthcare is underestimated.
Objectives of the patient-centred clinical pathway
The overall objective of the clinical pathway is to improve management and thus reduce morbidity and mortality from sepsis. Based on the challenges and needs (), the working group identified four specific objectives for the clinical pathway:
A larger proportion of severely ill patients with suspected sepsis in the ED should be identified early and receive adequate management.
A larger proportion of patients with sepsis should receive an accurate sepsis diagnosis code, according to the International Classification of Diseases, 10th revision (ICD-10).
A larger proportion of patients with sepsis should receive adequate information upon hospital discharge.
A larger proportion of patients with sepsis should be subjected to follow-up after in-hospital care.
Focus actions of the patient-centred clinical pathway for sepsis
Based on the objectives listed above and international [Citation1,Citation2,Citation18] and national [Citation3,Citation8] guidelines, the working group has developed a flow-chart of the Patient-centred clinical pathway, see . A detailed description of the boxes in the flow-chart is presented in . The clinical pathway is focused on the assessment of patients with suspected sepsis in the ED, on discharge from sepsis care and on follow-up after sepsis care. It includes four specific actions, indicated in red colour in the flow-chart ():
Figure 2. Flow chart of the patient-centred clinical pathway for sepsis. The focus areas of the clinical pathway are indicated in red. Abbreviations: ICU: intensive care unit; ICF: intermediate care facility.
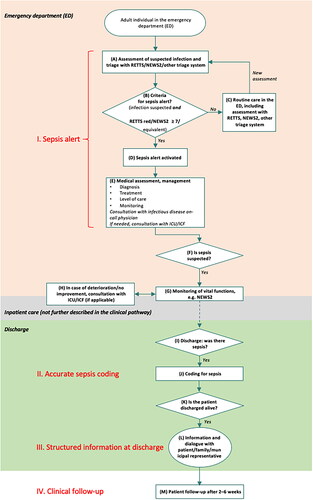
Table 1. Detailed description of the boxes presented in the flow-chart ().
I. Sepsis alert
A sepsis alert was designed to enable early detection and management optimisation of severely ill patients with suspected sepsis in the ED (). The sepsis alert includes screening, activation of the sepsis alert and structured medical assessment, including consultation with infectious diseases physician, and if needed consultation with intensive care and/or intermediate care facility. The routine involvement of different competences facilitates patient-centred optimisation of the management [Citation19,Citation20].
The sepsis alert should be activated for patients with clinical suspicion of infection in combination with the highest triage priority corresponding to the highest level of acuity. The most commonly used triage system in Swedish EDs at the time of the design of the clinical pathway was the Rapid Emergency Triage and Treatment System (RETTS) system [Citation21], in which the colour red corresponds to the highest triage priority and the NEWS2 system [Citation13], in which a score of ≥7 corresponds to the highest triage priority.
The operational criteria for activating the sepsis alert are (all three criteria must be met):
Adult patient (≥ 18 years of age) arriving to the ED
Suspicion of infection (e.g. fever, history of fever, acute onset of general malaise, cough, skin redness or acute onset of urinary or gastrointestinal symptoms)
RETTS red, NEWS2 ≥ 7 or equivalent acuity level with another triage system upon arrival to the ED.
The patients in the ED who do not fulfil the criteria for activating the sepsis alert are continuously re-evaluated (as part of clinical routine) (). If the sepsis alert criteria eventually become fulfilled, the sepsis alert should be activated. It should be noted that the majority of patients fulfilling the criteria for sepsis (according to the Sepsis-3 definition) in the ED will probably not fulfil the criteria for sepsis alert.
II. Accurate sepsis coding
An ICD-10 diagnosis code for sepsis (R65.1) or septic shock (R57.2) should be registered as the secondary code after the primary code of infection, in patients with a Sequential organ failure assessment (SOFA) score increase of at least two due to an infection during hospitalisation. To enable coding based on SOFA score, a national working group is currently developing an automatic SOFA score calculator that will be included in the electronic health record systems in Sweden.
III. Structured information at discharge
It is important to inform the patient about what happened during the in-hospital care and what the patient can expect in the future upon discharge from in-hospital care. In collaboration with Sepsisfonden, the working group has developed a written information sheet for patients who have been hospitalised for sepsis, which can be downloaded from Sepsisfonden’s website [Citation22]. A translated version is presented in Supplementary Materials (information to patients at discharge after in-hospital care for sepsis).
IV. Clinical follow-up
In order to identify persistent and new symptoms and needs for additional healthcare actions, the working group recommends routine telephone follow-up within two to six weeks after hospitalisation for sepsis. A translated instruction for the telephone follow-up is presented in Supplementary Materials (instructions for telephone follow-up two to six weeks after in-patient care for sepsis).
Data monitoring of the patient-centred clinical pathway
To enable monitoring of the sepsis population and the interventions of the Patient-centred clinical pathway, the working group identified quality indicators for follow-up. Three performance indicators () and nine process indicators () were identified, aimed to reflect different parts of the clinical pathway. As national data sources for these quality indicators are not available in Sweden, the indicator data must be extracted from the electronic health records. Currently, a national working group is working on a national system for the extraction of these indicators and on establishing a national electronic SOFA score calculator based on electronic health record data. The goal is to enable monitoring of the quality indicators on adequate populations at hospital level, healthcare region level and national level, to be able to identify inequalities and further develop sepsis care.
Table 2. Performance quality indicators.
Table 3. Process quality indicators.
Populations for monitoring
The working group aims to monitor the following three populations:
The broad sepsis population in the ED. Criteria (all must be met):
Adult patient (≥ 18 years of age) in the ED.
Presumed infection. The criteria for presumed infection have not yet been decided. Preliminary, the criteria from the Centers for Disease Control and Prevention [Citation23] will be used.
A SOFA score increase of ≥ 2 points due to the presumed infection. This part requires automatic calculation of SOFA score in the electronic health record system.
The target population for the sepsis alert. Criteria (all must be met):
Adult patient (≥ 18 years of age) in the ED.
Presumed infection. The criteria for presumed infection have not yet been decided. Preliminary, the criteria from the Centers for Disease Control and Prevention [Citation23] will be used.
RETTS red or NEWS2 ≥ 7 or equivalent acuity level with another triage system upon arrival to the ED.
The population for which sepsis alert was activated.
Consequence analysis and health-economic analysis
The working group has developed a separate consequence analysis regarding the patient-centred clinical pathway [Citation24]. This is focused on ethical aspects and displacement effects of the proposed interventions sepsis alert and telephone follow-up. As the sepsis alert is activated for patients with the highest triage priority, i.e. patients who are already prioritised, we believe that the risk for displacement effects of the sepsis alert on other diagnoses is small. On the other hand, the telephone follow-up is a new healthcare intervention that requires personnel resources. If it is not possible to hire new staff, this measure will have to be prioritised above other healthcare work. This could lead to a displacement effect. However, we consider the telephone follow-up to be ethically justifiable, as it fulfils a previously unmet medical need [Citation15].
In the consequence analysis [Citation24], there is also a health-economic analysis, which has been developed in collaboration with Center for Health Economics, Informatics and Healthcare Research, Region Stockholm, Sweden. This health-economic analysis shows that the increased costs associated with the sepsis alert, i.e. costs for coordination and increased involvement of different competences, are relatively small in comparison to the potential cost savings of shorter length of stay, that can be expected from the early identification and management optimisation of the sepsis alert [Citation16]. The healthcare analysis indicates that the increased costs of telephone follow-up can potentially be covered if outpatient deterioration can be detected and outpatient healthcare measures can be initiated to avoid re-admissions, that commonly occur after sepsis care [Citation25,Citation26].
Conclusion
A national patient-centred clinical pathway for sepsis has been developed and is currently being implemented throughout Swedish healthcare. At present, a national system for monitoring the sepsis population and the interventions of the clinical pathway, based on quality indicators from the electronic health records, is under construction.
We believe that the clinical pathway and the accompanying monitoring will provide a more efficient and equal sepsis care and improved possibilities to monitor and further develop sepsis care in Sweden.
Supplemental Material
Download MS Word (18 KB)Acknowledgment
The authors thank Christina Holmström, at the Swedish Association of Local Authorities and Regions, for review of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Reinhart K, Daniels R, Kissoon N, et al. Recognizing sepsis as a global health priority – a WHO resolution. N Engl J Med. 2017;377(5):414–417. doi: 10.1056/NEJMp1707170.
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287.
- Brink M, Cronqvist J, Fagerberg A, et al. Nu gäller sepsis-3 for definitioner och diagnostiska kriterier - De nya internationella begreppen ska användas i svensk sjukvard - bland annat ska ≫SIRS≪ och ≫svår sepsis≪ skrotas. Läkartidningen. 2018;115:E3W9.
- Mellhammar L, Wullt S, Lindberg A, et al. Sepsis incidence: a population-based study. Open Forum Infect Dis. 2016;3(4):ofw207.
- Ljungström L, Andersson R, Jacobsson G. Incidences of community onset severe sepsis, sepsis-3 sepsis, and bacteremia in Sweden – a prospective population-based study. PLoS One. 2019;14(12):e0225700. doi: 10.1371/journal.pone.0225700.
- Nationellt system för kunskapsstyrning Hälso- och sjukvård. Personcentrerat och sammanhållet vårdförlopp sepsis. Nationellt system för kunskapsstyrning Hälso- och sjukvård; 2021 [cited 2023 Jun 21]. Available from: https://d2flujgsl7escs.cloudfront.net/external/Personcentrerat_och_sammanhallet_vardforlopp_Sepsis.pdf
- Strålin K, Kurland L. Personcentrerat och sammanhållet vårdförlopp för sepsis hos vuxna: sepsislarm, korrekt diagnos och telefonuppföljning i fokus. Läkartidningen. 2021;118:21197.
- Svenska infektionsläkarföreningen. Vårdprogrammet för sepsis och septisk chock. Svenska infektionsläkarföreningen; 2022 [cited 2023 Jun 21]. Available from: https://infektion.net/knowledge/vardprogrammet-for-sepsis-och-septisk-chock/
- Sepsisfonden. Lund (Sweden): Sepsisfonden. [cited 2023 Jun 21]. Available from: https://sepsisfonden.se/
- Seymour CW, Gesten F, Prescott HC, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–2244. doi: 10.1056/NEJMoa1703058.
- Liu VX, Fielding-Singh V, Greene JD, et al. The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med. 2017;196(7):856–863. doi: 10.1164/rccm.201609-1848OC.
- Andersson M, Östholm-Balkhed Å, Fredrikson M, et al. Delay of appropriate antibiotic treatment is associated with high mortality in patients with community-onset sepsis in a Swedish setting. Eur J Clin Microbiol Infect Dis. 2019;38(7):1223–1234. doi: 10.1007/s10096-019-03529-8.
- Löf (Löf regionernas ömsesidiga försäkringsbolag). National early warning score 2. Löf (Löf regionernas ömsesidiga försäkringsbolag); 2018 [cited 2023 Jun 21]. Available from: https://lof.se/filer/NEWS2-broschyr.pdf
- Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794. doi: 10.1001/jama.2010.1553.
- Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319(1):62–75. doi: 10.1001/jama.2017.17687.
- Rosenqvist M, Bengtsson-Toni M, Tham J, et al. Improved outcomes after regional implementation of sepsis alert: a novel triage model. Crit Care Med. 2020;48(4):484–490. doi: 10.1097/CCM.0000000000004179.
- Valik JK, Ward L, Tanushi H, et al. Validation of automated sepsis surveillance based on the sepsis-3 clinical criteria against physician record review in a general hospital population: observational study using electronic health records data. BMJ Qual Saf. 2020;29(9):735–745. doi: 10.1136/bmjqs-2019-010123.
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2021. Crit Care Med. 2021;49(11):e1063–e1143. doi: 10.1097/CCM.0000000000005337.
- Viale P, Tedeschi S, Scudeller L, et al. Infectious diseases team for the early management of severe sepsis and septic shock in the emergency department. Clin Infect Dis. 2017;65(8):1253–1259. doi: 10.1093/cid/cix548.
- Madaline T, Wadskier Montagne F, Eisenberg R, et al. Early infectious disease consultation is associated with lower mortality in patients with severe sepsis or septic shock who complete the 3-hour sepsis treatment bundle. Open Forum Infect Dis. 2019;6(10):ofz408. doi: 10.1093/ofid/ofz408.
- Mellhammar L, Linder A, Tverring J, et al. Scores for sepsis detection and risk stratification - construction of a novel score using a statistical approach and validation of RETTS. PLoS One. 2020;15(2):e0229210. doi: 10.1371/journal.pone.0229210.
- Sepsisfonden. Utskrivning efter vård av sepsis. Lund (Sweden): Sepsisfonden; 2021 [cited 2023 Jun 21]. Available from: https://sepsisfonden.se/wp-content/uploads/2022/06/utskrivning_broschyr_v1_220617.pdf
- Centers for Disease Control and Prevention. Hospital toolkit for adult sepsis surveillance. Atlanta (GA): Centers for Disease Control and Prevention; 2018 [cited 2023 Jun 21]. Available from: https://www.cdc.gov/sepsis/pdfs/sepsis-surveillance-toolkit-mar-2018_508.pdf
- Nationellt system för kunskapsstyrning Hälso- och sjukvård. Konsekvensbeskrivning för Personcentrerat och sammanhållet vårdförlopp Sepsis. Nationellt system för kunskapsstyrning Hälso- och sjukvård; 2021 [cited 2023 Jun 21]. Available from: https://kunskapsstyrningvard.se/download/18.7a95dc2f1818012627d1e44e/1655982720195/Vardforlopp-sepsis-konsekvensbeskrivning.pdf
- Prescott HC, Langa KM, Iwashyna TJ. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA. 2015;313(10):1055–1057. doi: 10.1001/jama.2015.1410.
- Dahlberg J, Linder A, Mellhammar L. Use of healthcare before and after sepsis in Sweden: a case-control study. BMJ Open. 2023;13(2):e065967. doi: 10.1136/bmjopen-2022-065967.
- Rosenqvist M, Fagerstrand E, Lanbeck P, et al. Sepsis alert - a triage model that reduces time to antibiotics and length of hospital stay. Infect Dis. 2017;49(7):507–513. doi: 10.1080/23744235.2017.1293840.
- Levy MM, Gesten FC, Phillips GS, et al. Mortality changes associated with mandated public reporting for sepsis. The results of the New York state initiative. Am J Respir Crit Care Med. 2018;198(11):1406–1412. doi: 10.1164/rccm.201712-2545OC.
- Socialstyrelsen. Anvisningar för kodning av sepsis och septisk chock. Koder ur ICD-10-SE samt exempel på kodning enligt Sepsis-3. [cited 2023 Jun 21]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/klassifikationer-och-koder/2021-10-7599.pdf

