ABSTRACT
People in low- and middle-income countries experience heart disease at alarming rates. As urbanization accelerates, cities can drive innovative partnerships to improve prevention and management of heart disease, bringing government, business and civil society together. Through Better Hearts Better Cities, we pioneered a people-centered and multisector initiative, guided and owned by local city authorities, to address cardiovascular disease and its underlying causes within the context of rapid urbanization, reaching millions of people. Cities across the world can apply its strategy, consisting of six pillars named CARDIO, shorthand for Care, Access, policy Reform, Data and digital, Intersectoral collaboration and local Ownership.
Introduction
Most of the world’s burden of cardiovascular disease falls on low- and middle-income countries (World Health Organization (WHO) Citation2021). At the same time, the trend of rapid, often unplanned urbanization is reshaping the developing world. The proportion of the world’s population living in urban areas rose from 34% in 1960 to 56% in 2019 (The World Bank Citation2021), and the UN Population Division projects that it will reach 68% by 2050 (United Nations (UN) Citation2019). In real terms, the global urban population will grow from 4.2 billion to 6.7 billion by 2050, and the majority of this growth will take place in low- and middle-income countries with Asia and Africa accounting for 90% of the projected increase (UN Citation2019). With urbanization drawing people to cities, urban health systems in low- and middle-income countries have registered new cases of heart disease at alarming rates (Sarki et al. Citation2015). Health officials are struggling to keep up (Elsey et al. Citation2019).
These factors make cities an ideal proving ground for innovative interventions to improve prevention and management of cardiovascular disease. At the same time, emerging digital technologies can help public officials quickly adapt to urban public health and health care ecosystems, making them more responsive to these new demands (WHO Citation2020). The key to success is to re-imagine how the urban built space can be utilized to proactively reach individuals at risk, providing them with convenient access points to cardiovascular health screening followed by referrals to appropriate care.
Through the Better Hearts Better Cities initiative, the Novartis Foundation and its partners have pioneered a new way to address cardiovascular disease and its underlying determinants within the context of rapid urbanization in low- and middle-income countries, reaching millions of people through an initiative guided and owned by local authorities. Working with government and other key stakeholders, managers of health and care programs can apply the initiative’s strategy, consisting of six pillars we have named CARDIO, in other urban contexts where resources are similarly constrained.
Heart health in an urbanizing world
Cardiovascular disease (CVD) is the single leading cause of death worldwide, killing 17.9 million people annually according to the WHO (Citation2017). Around the world 1.13 billion people are estimated to have hypertension – the prime risk factor for fatal CVD events such as heart attack or stroke – with two-thirds of these living in low- and middle-income countries (LMICs) (WHO Citation2021). WHO reports that 75% of the deaths from CVD occur in LMICs (WHO Citation2011).
The connection between urbanization and poor cardiovascular health is clear. Economic activities associated with urbanization, such as manufacturing or office work, tend to be more sedentary than labor-intensive pursuits such as agriculture. Migration from rural areas to cities is also typically accompanied by changing diets, with reduced access to fresh fruit and vegetables and greater intake of processed foods high in fat and sodium – along with a higher likelihood of tobacco and alcohol use (Hawkes et al. Citation2017). Unplanned urban growth characteristics of LMICs typically means spotty coverage with health facilities, poor sanitation (Neiderud Citation2015), and few provisions for active lifestyles, like public green and recreational areas (Ramaiah and Avtar Citation2019). In response, urban design is increasingly informed by health considerations, particularly design impacts on noncommunicable diseases. To promote residents’ health, for example, urban planning is shifting from enabling sprawl, which requires frequent and widespread vehicle use, to promoting higher population density, coupled with a move away from reliance on automobiles to greater utilization of public and active transport (Nieuwenhuijsen Citation2018).
A strategic approach to heart health in urban environments
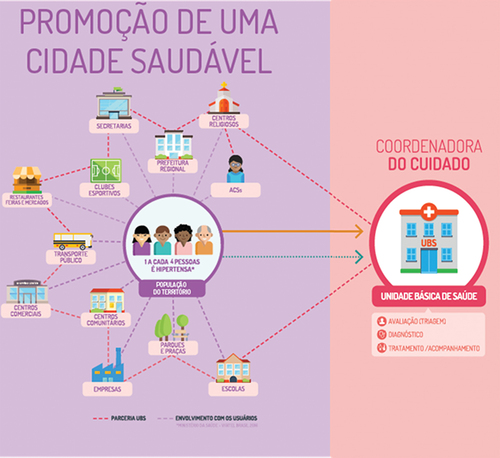
Such important tactical considerations, however, will have limited effect if they are not part of a ‘whole-of-city’ approach that maximizes opportunities to improve heart health at the population level. In 2016, the Novartis Foundation and its partners recognized the need for a new strategy that would integrate disaggregated health initiatives into a structured, urban health ecosystem – one that addresses both the underlying determinants of cardiovascular health and weaknesses in the public health and health care systems, while putting people at the center. This new strategy would also re-imagine how the urban built space could be leveraged to improve cardiovascular health. This means identifying various relevant touch points that individuals have with their urban environment, identifying potential access points to CVD screening, then tailoring outreach activities to engage individuals at risk and support them through the journey from screening into health management and care ().
Figure 1. Concept for creating a whole-of-city, heart-healthy ecosystem in São Paulo. Created by Instituto Tellus, Yara Baxter, Johannes Boch.
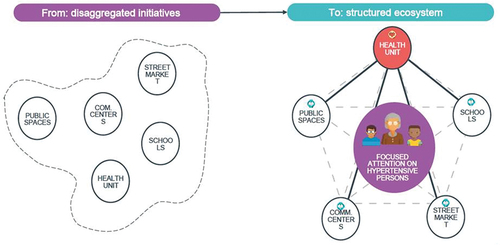
Figure 2. Shifting cities from implementing disaggregated health initiatives to fostering an ecosystem for supporting heart health. Created by Instituto Tellus, Yara Baxter, Johannes Boch.
Acting on a population health emergency of this size requires political support from city authorities and a range of multisectoral partners. Together, we convened city officials and companies from multiple sectors along with health-care providers, NGOs, and individuals from urban communities themselves to identify whole-of-city solutions.
We developed partnerships in three cities – Ulaanbaatar, Mongolia; Dakar, Senegal; and São Paulo, Brazil – cities facing high rates of CVD, to launch Better Hearts Better Cities, an initiative that marshals data and digital technology, previously untapped community resources, and multisector partnerships to make cardiovascular health a locally managed priority in fast-growing urban areas. Ethical clearance was obtained in all three countries for the implementation and evaluation of the Better Hearts Better Cities initiative. Results to date indicate that the approach has the potential for adaptation and replication by other cities around the world.
The urban context
Despite some differences (with over 12 million people, São Paulo is nearly ten times the size of Ulaanbaatar) these three cities have several things in common. Most important is their shared story of rapid, unplanned development. Over the last two decades São Paulo’s population increased by 30% (Macrotrends Citation2021a), Dakar’s by 69% (Macrotrends Citation2021b), and Ulaanbaatar’s by 109% (City Population Citation2021) according to data compiled by the United Nations. Such extreme growth challenges urban development, infrastructure planning and social-service provision. These cities also exhibit similar social trends, including increasingly sedentary lifestyles and changing diets, making them hot spots for hypertension and CVD. In São Paulo one in four adults over 25 suffers hypertension (Campbell et al. Citation2019), similar to rates of 25.6% of adults in Ulaanbaatar (Potts et al. Citation2020) and 24.7% in Dakar (Macia et al. Citation2016).
CARDIO: a six-pillar strategy for reducing heart disease
In collaboration with city authorities and local partners, we developed a strategy that consisted of six pillars that we later branded as CARDIO – shorthand for quality Care, Access, policy Reform, Data and digital technology, Intersectoral collaboration, and local Ownership.
Pillar 1: improve quality of CARE
This means bringing local hypertension protocols and clinical algorithms in line with established guidelines, such as those developed by the European Society of Cardiology or jointly by the American College of Cardiology and the American Heart Association, translating them into clinical decision-making tools and simple treatment algorithms, and providing health workers with technical training on their use.
Pillar 2: ensure ACCESS
Bringing health and care closer to where people live and work requires training non-health actors to perform regular outreach and hypertension screenings at a variety of unconventional, high-traffic public venues across the city. Screening is done with simple-to-use, automated blood pressure measurement tools (). These same actors are then trained to deliver accurate health information and refer people needing follow-up to the health system.
Pillar 3: REFORM policies
Policy reform is essential to ensuring that all have equitable access to improved dietary options and opportunities for exercise, putting heart-healthy choices within reach of all. In Ulaanbaatar, the government introduced tobacco taxes as recommended by the World Health Organization, and the managers of the initiative worked with the national food association to decrease salt in processed food. In all three cities, health advocates worked with local officials and national policymakers to reform policies, boosting the availability of heart-healthy foods and spaces for exercise.
Pillar 4: leverage DATA and DIGITAL technology
Digital and data-driven technologies in health provide an opportunity to truly reimagine health systems, from being reactive, to becoming proactive, predictive, and ultimately preventative. Yet city authorities face challenges making health decisions based on clinical outcomes and recent data. Data reports produced by the World Health Organization, which can lag real-time information by one or two years, often provide the primary evidence base for decision-making pertaining to CVD. The Better Hearts Better Cities initiative introduced the systematic tracking of progress and data on hypertension diagnosis, treatment and control rates, for use in real-time (Novartis Foundation Citation2021, Boch et al. Citationforthcoming). Data collected during the initiative are currently being used by the health authorities in Ulaanbaatar to further investigate the connection between health indicators, urban structures, and environmental and social components.
Digital technology also allows us to deliver health and care closer to where people live, work, and play. New sensors, Internet of Things solutions, and remote monitoring technologies can help people self-screen for CV risk factors, accelerating detection, and empowering patients to take more responsibility for managing their own health. Ideally, digitized systems will allow people to own their own health data and share it with health providers of their choice.
Pillar 5: Create an INTERSECTORAL coalition
While donors played a catalytic role in Better Hearts Better Cities, public- and private-sector stakeholders from across each of the cities, spanning health, urban planning, finance, technology, education, work, insurance, and food and agriculture, then designed the initiative. In each city, we worked with city authorities to establish a steering committee focused on broad strategic direction, which included the cities’ mayor or other political representatives, and senior public managers with responsibilities for relevant sectors, including health, education, and agriculture. A second, operational committee, comprised of health professionals and technical experts from various sectors, was responsible for implementing strategy and reporting on interventions. We identified individuals to serve on these committees through a comprehensive stakeholder mapping carried out at the start of the initiative. Together, these individuals manage the initiative.
Pillar 6: ensure local OWNERSHIP
Success rests with ensuring that local partners own responsibility for designing, implementing, and monitoring the initiative. In São Paulo, we began by working with the city authorities and local stakeholders through a design-thinking process that identified critical challenges affecting the value chain for hypertension. We then co-created solutions for better preventing and treating hypertension, including promoting healthy lifestyles, empowering patients, and improving the efficiency and quality of care in primary health centers, reducing the list to 30 interventions that were feasible and cost-effective. City authorities became determined to improve the performance of the primary health system when they saw that long wait lists for specialized care had made it impossible to reduce CVD rates.
Mainstreaming built space considerations across the CARDIO strategy
Successfully implementing the CARDIO strategy required leveraging opportunities unique to each of the three physical urban environments. Drawing on lessons from previous public-private partnerships and cardiovascular health programs in LMICs, our teams mapped their local health systems, locating weaknesses in hypertension identification and treatment and identifying the underlying determinants of high blood pressure that we could address. Primary health facilities were outfitted with blood pressure screening corners, and policies were modified to require all clients to screen their blood pressure.
A broader aim was to address living conditions that affect health, bring health and care closer to where people live, and build coordinated care pathways for patients to improve hypertension detection, treatment, and control. This meant decentralizing access to CVD interventions. Working with city authorities and partners, we conducted territory analyses, identifying markets where fresh food was sold (from supermarkets to street markets and vegetable stands), popular fast-food chains, city parks and green spaces, fitness centers, and large commercial areas that could be used for screening, outreach and education, and physical activities. We also mapped local organizations with whom we could partner on program initiatives.
In São Paulo, for example, locally collected data showed men were less likely than women to seek cardiovascular care in health facilities. To address this gender disparity, we reached out through hypertension information and screening access points in physical locales where men tend to congregate on the way to work or during leisure time, including in local markets, the Corinthians professional football club stadium, and metro stations.
To position access points in areas with the highest population touch points, we mapped people flow within the city, identifying district city hall, schools, citizen services organizations, shopping centers, metro stations, the football stadium, samba clubs and competitions, weekly farmers markets, and ad hoc popular events as the most highly trafficked locations. We installed CVD screening access points in these locations, prioritizing areas that would not disrupt people flows. These activities led city health authorities to develop standard operating procedures for community engagement in these locations.
To strengthen the CVD prevention ecosystem, we worked with partners to increase access to healthy foods within city limits and to expand opportunities for healthy physical activities. In Dakar, for example, we worked with agricultural producers from regions outside the city to boost the supply of fresh, healthy foods within the city proper. This engagement began with a workshop titled ‘Agriculture and Urban Health: Consuming Fresh Products in Dakar,’ which brought together 30 leaders from Senegal’s health and agriculture sectors to review dietary habits; models for sustainably increasing production and the supply of fresh, healthy, quality foods; and to ultimately develop a roadmap for operationalizing solutions.
In all cases, we leveraged the built environment to create opportunities for behavior-change education and physical activity. Local health authorities engaged community leaders to make physical health and nutrition education available in city workplaces and schools. As part of this work in Dakar, for example, we supported the establishment of the Dakar Workplace Health Coalition, comprised of 18 companies representing more than 36,000 employees. The coalition’s mandate is to create an enabling environment for introducing healthy foods and physical education opportunities into the workplace, among other interventions aimed at reducing employees’ risk of CVD (Ndione and Aerts et al. Citation2021). In Ulaanbaatar, the Ministry of Health and local partners organized events for various age groups, including dancing in the city square.
Results
Initial results indicate Better Hearts Better Cities is already having a substantial positive impact on population health. Preliminary data indicated an almost three-fold increase in blood pressure control (BP) in São Paulo and Dakar within just one, respectively, 2 years of CARDIO implementation, achieving 31%, respectively, 19% BP control rates (Novartis Foundation Citation2021, Boch et al. Citationforthcoming). Given the existing evidence linking uncontrolled hypertension to the risk of stroke and heart attack, we anticipate a subsequent reduction in the number of people suffering from these life-threatening attacks.
As an output of establishing new information systems, within two years the three cities were collecting real-time, actionable data. Acting on that data saw city authorities shift their mindsets to embrace real-time decision-making, which enabled them to respond more efficiently to their populations’ health needs.
In São Paulo – where interventions reached 1.5 million people – at the start of the initiative, only one in three primary health centers had aggregated reports on the number of hypertensive patients receiving care. A year later, all facilities were maintaining aggregate data, which has become routine for proper hypertension management.
To ensure the initiative remains sustainable after our initial catalytic investment, advocates and policymakers involved from the beginning have continued to strengthen and expand buy-in from government and other partners, in the form of commitments to provide long-term funding. Most notable are policy successes such as in Mongolia’s Ministry of Health where funding for primary care increased significantly between 2017 and 2019, the National Health Insurance fund boosted financial support to primary health centers by about 300% and raised reimbursements for hypertension medications, paid for in part by a nationwide tobacco tax (Saric et al. Citationforthcoming).
Conclusion
The future is clear: humanity is congregating in cities. Urbanization presents broad public health challenges, but, fortunately, cities also provide opportunities to use tools and resources which, with modest investment, will allow health and political leaders to prevent many of urbanization’s negative health impacts. With a comprehensive strategy like CARDIO, city authorities and their partners can take a ‘whole of city’ approach to improving population health. This requires making targeted improvements in the way the health system functions, aided by the adoption of new technology and data analytics. It also requires stakeholder engagement to leverage the urban built space in ways that support the broader strategy. The CARDIO approach demonstrates how a convener and catalyzer, in this case the Novartis Foundation, can transform health and care with strategies that work locally and can be replicated in cities globally, improving health outcomes for millions of people, accelerating the achievement of Sustainable Development Goals.
Readers can find further information on Better Hearts Better Cities here: https://globalhealthprogress.org/collaboration/better-hearts-better-cities/ and here: https://www.novartisfoundation.org/past-programs/better-hearts-better-cities
Acknowledgments
We would like to express our sincere gratitude to all the public authorities and partners involved in this initiative in Ulaanbaatar, Mongolia, Dakar, Senegal, and São Paulo, Brazil.
Catalytic funding for the Better Hearts Better Cities initiative is provided by the Novartis Foundation. In São Paulo, co-funding is provided by the Umane Foundation. We thank Paul Jensen and Phil Coticelli for the editing support.
Disclosure statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Funding
Notes on contributors
Ann Aerts
Ann Aerts is head of the Novartis Foundation, which is committed to transforming the health of low-income populations by leveraging data, technology and artificial intelligence. Dr Aerts holds degrees in medicine and tropical medicine, as well as a masters in public health, and has also authored numerous publications on digital health, innovative approaches and multisector partnerships to address global health challenges.
Jo Ivey Boufford
Jo Ivey Boufford is an expert in urban health, disease prevention, healthy aging, health promotion and health disparities. Her extensive experience in medicine, international affairs, health policy and public administration has seen her take leadership positions in numerous organizations, including; the US Department of Health and Human Services, the World Health Organization, the International Women's Health Coalition, the National Academy of Medicine, the Commonwealth Fund, and New York University, to name a few. Dr Boufford holds a degree in Psychology and received her Doctorate in Medicine, with distinction, both earned from the University of Michigan.
References
- Boch, J., et al., forthcoming. A multisector initiative to reduce hypertension in urban populations: an observational study on cascade of care outcomes. (Manuscript submitted).
- Campbell, N., et al., 2019. São Paulo call to action for the prevention and control of high blood pressure: 2020. Journal of clinical hypertension, September, 21, 1744–1752. doi:10.1111/jch.13741
- City Population, 2021. Ulaanbaatar. City Population. Available from: https://www.citypopulation.de/en/mongolia/admin/511__ulaanbaatar/ [Accessed 25 May 2021].
- Elsey, H., et al., 2019. Rethinking health systems in the context of urbanization: challenges from four rapidly urbanizing low-income and middle-income countries. BMJ global health, June, 4 (3), e001501. doi:10.1136/bmjgh-2019-001501
- Hawkes, C., Harris, J., and Gillespie, S. 2017. “Changing diets: urbanization and the nutrition transition.” Global Food Policy Report 2017. Washington, DC: International Food Policy Research Institute, 34.
- Macia, E., Gueye, L., and Duboz, P., 2016. Hypertension and obesity in Dakar, Senegal. PLOS one, September, 11 (9), e0161544. doi:10.1371/journal.pone.0161544
- Macrotrends, 2021a. São Paulo, Brazil Metro area population 1950-2021.” Macrotrends. Available form: https://www.macrotrends.net/cities/20287/sao-paulo/population [Accessed 25 May 2021].
- Macrotrends, 2021b. Dakar, Senegal Metro Area population 1950-2021. Macrotrends. Available from: https://www.macrotrends.net/cities/22439/dakar/population [Accessed 25 May 2021].
- Ndione, I., et al., 2021. Fostering cardiovascular health at work–case study from Senegal. BMC public health, June, 21 (1), 1–11. doi:10.1186/s12889-021-11109-9
- Neiderud, C.-J., 2015. How urbanization affects the epidemiology of emerging infectious diseases. Infection ecology & epidemiology, June, 5 (1), 27060. doi:10.3402/iee.v5.27060
- Nieuwenhuijsen, M., 2018. Influence of urban and transport planning and the city environment on cardiovascular disease. Nature, (15), 432–438. doi:10.1038/s41569-018-0003-2
- Novartis Foundation, 2021. Urban population health toolkit. Novartis Foundation. Available from: https://www.novartisfoundation.org/urban-population-health-toolkit [Accessed 25 August 2021].
- Potts, H., et al., 2020. Hypertension prevalence and control in Ulaanbaatar, Mongolia. Journal of clinical hypertension, January, 22 (6), 1–8. doi:10.1111/jch.13784
- Ramaiah, M. and Avtar, R., 2019. Urban Green Spaces and Their Need in Cities of rapidly urbanizing India: a review. Urban science, August, 3 (3), 94. doi:10.3390/urbansci3030094
- Saric, J., et al., forthcoming. Assessing the contributions of the Better Hearts Better Cities initiative to shift political priority towards cardiovascular health in Brazil, Mongolia and Senegal. (Manuscript submitted).
- Sarki, A., et al., 2015. Prevalence of hypertension in low- and middle-income countries: a systematic review and Meta-analysis. Medicine, December, 94 (50), e1959. doi:10.1097/MD.0000000000001959
- UN, 2019. World urbanization prospects: the 2018 revision. United Nations, Department of Economic and Social Affairs, Population Division. New York, NY: United Nations.
- The World Bank, 2021. Urban population (% of total population). United Nations Population Division, cited by The World Bank. Available from: https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS [Accessed 25 May 2021].
- World Health Organization, 2011. World Health Organization. Global status report on noncommunicable diseases 2010. Geneva: World Health Organization.
- World Health Organization, 2017. Cardiovascular diseases (CVDs). World Health Organization, May 17. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- World Health Organization, 2020. Digital health: transforming and extending the delivery of health services. World Health Organization, September 9. Available from: https://www.euro.who.int/en/health-topics/Health-systems/digital-health/news/news/2020/9/digital-health-transforming-and-extending-the-delivery-of-health-services
- World Health Organization, 2021. Hypertension. World Health Organization, May 17. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension.

