ABSTRACT
Emerging trends show declines in maternal and perinatal mortality and morbidity in urban populations might be slower than in rural areas in a variety of contexts. This is happening at a critical juncture in time when urban populations are rapidly increasing and might be partly driven by specifics of vulnerability of the urban poor in Low-income countries and High-income countries alike. Poor maternal and perinatal health outcomes are largely preventable but focusing solely on healthcare interventions misses critical opportunities to reduce ill-health. Social and environmental determinants such as poverty and the impact of climate change must be integrated into policy decisions, especially to benefit poor urban dwellers. Integrating data on the social determinants of health into policy decisions can help multisectoral stakeholders embrace a more Health-in-all-policy approach creating opportunities for better outcomes for these urban poor women and their offspring. We provide examples of two cities – Rotterdam and Kampala – to show that successful multi-sectoral approaches that can address urban maternal and perinatal inequalities should focus on interventions in which healthcare and non-healthcare determinants are integrated.
Introduction
Globally, maternal deaths have dropped substantially over the past three decades, from 500,000 in 1990 to about 295,000 in 2017. However, the current global maternal mortality ratio of 211 deaths per 100,000 live births is nearly triple the level envisioned by the Sustainable Development Goals (SDG) target of 70 by 2030 (World Health Organization Citation2019). In addition, the burden of perinatal mortality (stillbirths and newborn deaths) contributes 4.5 million deaths annually (Hug et al. Citation2019, Citation2021). The majority of the reasons why women and babies die and the high burden of mortality on the most vulnerable within societies can be addressed by integrating evidence-based interventions in addition to strong health systems (Graham et al. Citation2016).
The main determinants of maternal and perinatal survival – living conditions and access to good quality care – are closely linked to place of residence. One of the sentinel determinants of conditions of living space is urbanicity. Urban population grows by an estimated 60 million every year (World Health Organization Citation2010); in 1990, 4 in 10 people lived in an urban area compared to more than half in 2010 and a projected 7 out of 10 people in 2050 (United Nations Citation2019). Therefore, the majority of the world’s women, and their children, will be living in cities in coming decades. This strongly suggests that potential for improving maternal and perinatal survival and wellbeing is intricately connected to the characteristics of urban life. Any approach aiming to reduce maternal and perinatal mortality must consider the features of the urban environment which can contribute to these causes of death.
Furthermore, there are several features of urban living that can contribute to inequities in maternal and perinatal morbidity and mortality. While urban areas are characterized by positive health on many dimensions, a substantial proportion of urban residents are exposed to unsafe working conditions, social exclusion, poverty, lack of access to clean water, poor housing, air pollution, poor sanitation, and vulnerability to extreme climate-related events, all of which are associated with maternal and perinatal health outcomes (Africa Progess Panel Citation2010). Compounding the contribution of these factors are under-resourced health systems. For example, women who live in slums or poor parts of cities and experience an obstetric emergency might choose to bypass the nearest public hospital due to uncertainties about quality of care, but experience catastrophic delays en route another health facility due to traffic and insecurity on the roads (Banke-Thomas et al. Citation2019, Babajide et al. Citation2021). This can be seen as was addressed in the case of Kampala (.)
Box 1. Harmonised Decision-making: Urban Health Strategy in the City of Kampala
For decades, research and policies on maternal and perinatal health have focused on disadvantages that emerge from living in rural settings and issues related to the quality of care within health facilities in rural areas (Channon et al. Citation2010). However, with rapidly evolving global urbanization, research and policies must broaden their focus to also the specificities of collecting data and informing action in urban areas. Examples from around the world show that a multisectoral policy approach which takes into account both medical and social sectors can help address some of these challenges. Such approaches were used in Rotterdam, the Netherlands (.) to address context-specific issues. Further, we suggest that without a global effort to share, learn from, and implement such multisectoral policy approaches, improvements in maternal and perinatal survival and wellbeing will not keep pace with global urbanization and SDG targets.
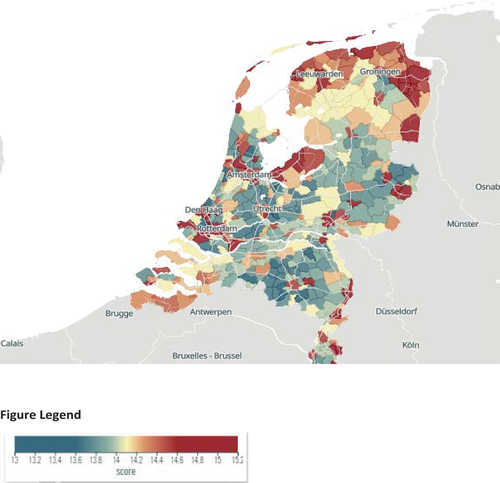
Box 2. Heatmaps (Vulnerability Atlas) in the Netherlands
Achieving this will require a broader understanding of the complex interconnected determinants that affect the life and health of women in cities, and mechanisms to make sure that understanding informs decision-making. The example of Rotterdam shows that basic improvements to housing and social protection, income, and food security has the potential to transform perinatal survival among vulnerable populations, even in high-income settings with mortality rates below global average. This strategy recognized that improving health and reducing inequities starts at the beginning of life (the first 1,000 days). It also argued for availability and improved use of data on social determinants of maternal health that can contribute to a Health-in-all-Policy approach in cities. This was done in the Netherlands through heat maps on perinatal mortality, prematurity, and low birth weight, This resulted in the national programs ‘Healthy Pregnancy for All’ and ‘Solid Start’ (Schreiber Citation2020, Waelput et al. Citation2017, Citation2022).
A way forward
We are beginning to see action on some of these challenges in several sectors. The World Health Organization recently launched a special initiative for Action on Social Determinants of Health for Advancing Equity which focuses on demonstrating a reduction in health inequities by improving the social circumstances that promote health and access to quality healthcare for at least 20 million disadvantaged people in at least 12 countries by 2028 (Working Group for Monitoring Action on the Social Determinants of Health Citation2021). Urban cities’ decision-makers will benefit from data about the social determinants of urban maternal and perinatal health. Technical capacity must be nurtured to allow public health practitioners and non-healthcare stakeholders to inform policy and decision-making on urban maternal and perinatal health and the social determinants affecting it. Strong consideration should be given to providing data on the social determinants of health to decision-makers. The report of the 3-D commission provided recommendations about how this could be achieved and may offer a template for the adoption of approaches to data gathering that can inform decision-making (3-D Commission Citation2021, Martins et al. Citation2021).
Researchers can contribute through generating evidence that can help document the spatial magnitude of maternal and perinatal inequities in cities. Priorities include: understanding which determinants of maternal and perinatal health are most relevant, which multisectoral maternal health policies exist, and how they are formulated and implemented.
Policy making should be informed by the actions targeting maternal health and safe motherhood that have been implemented in a few cities (Africa Progess Panel Citation2010, Waelput et al. Citation2022). While some similar policies have met with local success in few countries (Mwoka et al. Citation2021) as policy makers took into consideration social and environmental determinants in policy decisions to improved population health and closed gaps of inequities, many questions remain. Do these policies make provision for women in underserved parts of the cities? Is there an in-depth understanding through disaggregated data of the challenges of varying social groups of women in the city? What data on social determinants inform the policy process? Exploring policy-making cycles specific to how cities are positioned for optimum maternal health and capturing the use of non-healthcare data in growing cities will advance understanding for city-level decision-makers on adaptation of data on social factors to maternal health policies.
Figure 1. Sample heatmaps showing clusters of vulnerable mothers and children in the Netherlands (https://kwetsbaarheid.kansenkaart.nl/kwetsbaarheidsindex#7.2/52.241/5.285). The project is financed by the Bernard van Leer Foundation.
Societal valorization of knowledge through collaboration between academics, government, and non-profit organizations is equally essential (Steegers et al. Citation2016). There is tremendous potential for research that engages multi-stakeholders across diverse sectors. New knowledge from multidisciplinary research should be used to improve the health and wellbeing of the general population with a view to addressing health inequities. Researchers can also identify policies that influence decision-makers on urban maternal and perinatal health as well as what measure of multisectoral collaboration is integrated into the process. A combination of qualitative methods, Delphi techniques and policy analysis can be used to investigate how different cities are positioned to improve the health of urban poor women of reproductive ages. This should include focusing on the effectiveness of newly designed interventions, in which medical and social care are integrated. Cross-cities and cross-national comparative case studies can be helpful to provide a clear picture of a feasible health-in-all policy in action in not different settings. Multi-city selection should consider diversity- multicultural, high, middle, and low-income settings, as well as varying socio-economic groups. Findings can inform new strategies for urban maternal and perinatal health approaches and could provide multisectoral stakeholders with a framework for action to accelerate progress in maternal and perinatal morbidity and mortality.
Author contributions
All Authors have contributed significantly to this manuscript. OB and LB were responsible for the initial conceptualization of this commentary. IOA, SMA and SG provided suggestions and comments to refine the content. PW and EAPS provided expert information for Box 1 and 2, respectively. OB has led the drafting process, with input from all authors. All authors have approved the final manuscript.
Acknowledgments
We would like to acknowledge Dr. Guillermo Hegel for his views and suggestions. We would like to also appreciate the 3-D Commission Project Director – Salma M Abdalla and the Commission Chair - Dean Sandro Galea, for ground-breaking work for the future of population health, creating opportunities for better scholarship and practice among diverse multi-stakeholders.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Opeyemi Babajide
Opeyemi Babajide is an urban health researcher based at the Urban Health Collaborative of the Dornsife School of Public Health at Drexel University. She is interested in how data translates to decision-making, and she seeks to ensure that science drives programs to benefit the underserved and close the gaps of health disparities. At the 3-D Commission, she is a research fellow interested in issues of global population health at the intersection of the social determinants of health and data science. She brings over ten years of experience in multistakeholder management and participatory intervention.
Lenka Beňová
Lenka Beňová is a reproductive and maternal health researcher based at the Sexual and Reproductive Health Group at the Institute of Tropical Medicine in Antwerp, Belgium. She applies mainly quantitative methods from epidemiology and demography to primary and secondary data to understand and address issues of access to and provision of health care and its quality. She is leading a portfolio of work aiming to identify and tackle the unique challenges of ensuring maternal health and wellbeing in urban areas.
Ibukun-Oluwa Omolade Abejirinde
Dr. Ibukun-Oluwa Omolade Abejirinde is an applied researcher with a particular interest in digital innovation in healthcare, health systems and policies, and maternal health. Her research applies a trans-disciplinary approach anchored in the field of global health and lies at the nexus of systems thinking, theory-driven inquiry and implementation science. In addition to her appointment as a Scientist at Women’s College Hospital Institute of Health System Solutions and Virtual Care, Dr. Abejirinde is an Assistant Professor at the Dalla Lana School of Public Health, University of Toronto.
Eric A.P. Steegers
Eric A.P. Steegers is professor and chair of Obstetrics and Gynaecology at the Erasmus MC in Rotterdam, The Netherlands. His translational research interests include (a) the etiology of adverse pregnancy outcome in relation to suboptimal embryogenesis and first trimester placentation, and (b) maternal cardiovascular health after complicated pregnancies. He leads innovative local and national programs of renewed risk selection and intervention both before (preconception care) and in early pregnancy integrating collaborations with local and national governments with particular focus on vulnerable families in deprived districts.
Peter Waiswa
Peter Waiswa is an Associate Professor of Health Policy Planning and Management of the School of Public Health at Makerere University College of Health Sciences. He is a member of the WHO Strategic and Technical Advisory Group of Experts (STAGE) for Maternal, Newborn, Child and Adolescent Health and Nutrition which currently provides independent advice to the WHO Director General. He started and leads the Makerere University Maternal Newborn and Child Health Centre of Excellence and the INDEPTH Network Maternal, Newborn and Child Health Research Group.
Sandro Galea
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He serves as chair of the Boston Board of Health and is past chair of the board of the Association of Schools and Programs of Public Health.
Salma M Abdalla
Salma M Abdalla, a physician by training, is a Research Fellow at Boston University School of Public Health. Dr Abdalla is the Director of the Rockefeller-Boston University 3-D Commission on Determinants of health, Data science, and Decision making. Her research focuses on the social determinants of health and the health of populations. She also studies the effects of mass trauma on the mental health of populations. She has both scholarship and practice experience working on issues related to gender-based violence and mental health in Sudan.
References
- Africa Progess Panel, 2010. Maternal health: investing in the lifeline of healthy societies and economies.
- Babajide, O., Martins, D.C., Maani, N., et al., 2021. Improving decision-making for population health in nonhealth sectors in urban environments: the example of the transportation sector in three megacities—the 3-D Commission. Journal of Urban Health, 98 (S1), 60–68. doi:10.1007/s11524-021-00561-y
- Banke-Thomas, A., Wright, K., and Collins, L., 2019. Assessing geographical distribution and accessibility of emergency obstetric care in Sub-Saharan Africa: a systematic review. Journal of global health, 9 (1). doi:10.7189/jogh.09.010414
- Channon, A., et al., 2010. Examining the “urban advantage” in maternal health care in developing countries. PLoS medicine, 7 (9). doi:10.1371/journal.pmed.1000327
- Graham, W., Woodd, S., Byass, P., et al., 2016. Diversity and divergence: the dynamic burden of poor maternal health. The Lancet, 388 (10056), 2164–2175. doi:10.1016/S0140-6736(16)31533-1
- Hug, L., et al., 2019. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. The Lancet Global Health, 7 (6), e710–e720. doi:10.1016/S2214-109X(19)30163-9
- Hug, L., et al., 2021. Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: a systematic assessment. The Lancet, 398 (10302), 772–785. doi:10.1016/S0140-6736(21)01112-0
- Martins, D.C. et al., 2021. Integrating social determinants in decision-making processes for health: insights from conceptual frameworks—the 3-D Commission. Journal of urban health, 98, 51–59. https://link.springer.com/article/10.1007/s11524-021-00560-z
- Mwoka, M. et al., 2021. Housing as a social determinant of health: evidence from Singapore, the UK, and Kenya: the 3-D Commission. Journal of urban health, 98 (Suppl 1), 15–30. doi:10.1007/s11524-021-00557-8
- Rockefeller Foundation-Boston University 3-D Commission, 2021. Social determinants, and better decision-making for health - the report of the 3-D Commission Boston. Boston.
- Schreiber, L., et al., 2022. A solid start for every child: The Netherlands integrates medical and social care, 2009–2022. Innovations for Successful Societies. Innovations for Successful Societies, Princeton University. https://successfulsocieties.princeton.edu/publications/solid-start-every-child-netherlands-integrates-medical-and-social-care-2009-2022
- Steegers, E.A.P., et al., 2016. Societal valorisation of new knowledge to improve perinatal health: time to act. Paediatric and perinatal epidemiology, 30 (2), 201–204. doi:10.1111/ppe.12275
- United Nations, Department of Economic and Social Affairs - Population Division, 2019. World urbanization prospects: the 2018 revision. https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf
- Van der Hulst, M., De Groot, M.W., De Graaf, J.P., et al., 2018. Targeted social care for highly vulnerable pregnant women: design of the Mothers of Rotterdam cohort study. International journal of integrated care, 18 (s2), 288. doi:10.5334/ijic.s2288
- Waelput, A.J.M., Rijlaarsdam, C.W., and Steegers, E.A.P., 2022. Preconception health and choices: tailored solutions for prospective parents. International Journal of Birth and Parental Education, 9 (2).
- Waelput, A.J.M., et al., 2017. Geographical differences in perinatal health and child welfare in the Netherlands: Rationale for the healthy pregnancy 4 all-2 program. BMC pregnancy and childbirth, 17 (1), 1–13. doi:10.1186/s12884-017-1425-2
- Working Group for Monitoring Action on the Social Determinants of Health, 2021. It is time to build a fairer, healthier world for everyone, Everywhere by taking action on the social determinants of health to advance equity.
- World Health Organization, 2010. Hidden cities-unmasking and overcoming health inequities in urban settings. https://www.who.int/publications/i/item/9789241548038
- World Health Organization, 2019. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/
