ABSTRACT
Loneliness is a major social concern with health consequences worldwide for populations across different demographic, cultural, social, economic, geographic, and environmental contexts. In March 2021, we launched Horizon 2020 European Commission-funded project, ‘Reimagining Environments for Connection and Engagement: Testing Actions for Social Prescribing in Natural Spaces (RECETAS)’ to reduce loneliness and promote health-related quality of life. In this paper, we present the project logic model, informed by stakeholder input, that aims to guide the initiative from its design and implementation to its evaluation in six cities across three continents, including Europe (Barcelona, Helsinki, Marseille, Prague), Australia (Melbourne), and South America (Cuenca). This model is being used to guide the implementation and evaluation of nature-based social prescribing interventions. Process and outcome measures will be used to compare outcomes in different settings and population contexts. The use of a logic model with stakeholder input ensures that the interventions are responsive to local needs, sustainable, and transferable to other geographic, social, economic, and cultural contexts. Knowledge translation will be central to maximising impacts on population health, civil society, and health and social systems in urban areas.
Introduction
Loneliness is a major social concern with significant health consequences worldwide and refers to the subjective phenomenon that reflects a gap between an individual’s preferred and actual social relationships (Prohaska et al. Citation2020, Jansson and Pitkälä Citation2021). Loneliness may lead to and/or exacerbate chronic diseases such as cardiovascular disease, diabetes, cerebrovascular disease, and as well as anxiety, depression, cognitive decline, and mental well-being (Luanaigh and Lawlor Citation2008, Hawkley and Cacioppo Citation2010, Holt-Lunstad Citation2017).
In Europe alone, before SARS-CoV-2 pandemic, over 75 million European adults reported meeting with family and friends at most once per month and 30 million European adults frequently felt lonely (Yang and Victor Citation2011). Moreover, loneliness is most prevalent in Eastern and Southern Europe and affects all age groups (Yang and Victor Citation2011, d’Hombres et al. Citation2019). In the United Kingdom, the Office of National Health Statistics found that around 25% of the population sometimes, often or always felt lonely (Figueira et al. Citation2022). The issue is so concerning that in 2018, the Prime Minister of the United Kingdom appointed a ‘minister for loneliness’ to coordinate efforts around loneliness (Yeginsu Citation2018). The Surgeon General of the United States, Dr. Vivek Murthy, recently referred to loneliness as a public-health ‘epidemic’ (Murthy Citation2020). In the United States, a survey by Cigna Health Insurance, showed that almost 50% of adults reported feeling lonely often or always, and, among people aged 18-25 and mothers with young children, 61% and 51%, respectively, reported severe levels of loneliness (Cigna Citation2018). Among older adults, the National Academies of Engineering, Science, and Medicine found that prior to the pandemic, 35% of Americans over 45 years and 42% of respondents over 60 years reported feeling lonely at least sometimes (National Academies of Sciences E, Medicine Citation2020). In Australia, prior to the SARS-CoV-2 pandemic, 25% of Australians reported feelings of loneliness. Moreover, the Young Australian Loneliness Survey (2019) found that over 50% of young people felt they lacked companionship (Australian Institute of Health and Welfare Citation2021, Victorian Health Promotion Foundation SUoT Citation2019).
Loneliness arises from different aspects of life. There are three dimensions of loneliness – social, emotional, and existential – originally explored and defined by Weiss (Citation1975) and Moustakas (Citation2016) that should be examined when addressing loneliness. Moreover, loneliness should be distinguished from other related concepts, such as ‘social isolation’ (Victor Citation2015), which has been used interchangeably with loneliness but objectively represents few ties with others rather than the subjective feeling that one’s expectations about social connections are not fulfilled (Hawkley and Cacioppo Citation2010, Zavaleta et al. Citation2017).
The SARS-CoV-2 pandemic and related confinement and social distancing measures have aggravated the problem and placed the issues of loneliness and mental health at the forefront of communities worldwide (Palgi et al. Citation2020, Killgore et al. Citation2020). For many, mandated confinement and social distancing measures increased loneliness. In Australia, for example, 2020 and 2021 surveys revealed that just over 35% of the population reported feelings of loneliness and that loneliness decreased by 5% between lockdowns. This has underscored how important social contacts are for mental health and well-being (Brooks et al. Citation2020, Australian Institute of Health and Welfare Citation2021).
Communities are seeking effective and efficient solutions to address the array of health concerns that may be rooted in loneliness, given that mental health visits to primary care providers are perceived to be more time-consuming and therefore burdensome for health care providers. In the United Kingdom, Naylor and others of the King’s Fund reported that referrals from primary care to community mental health teams increased by almost 20% between 2010 and 2015 and prescriptions for antidepressants doubled from 2005 to 2015 (Naylor et al. Citation2020). Moreover, in a 2018 survey of 1,000 general practitioners in the United Kingdom, Mind found that approximately 40% of general practitioner appointments involved mental health (Mind Citation2018). Thinking outside of the ‘medical care’ box, solutions that facilitate access to nearby nature in socially supported ways offer a potential strategy for sustaining mental and physical well-being. This notion of nature-based social engagement crystalized during the pandemic as stay-at-home mandates revealed the importance of being outdoors and accessing nature and people’s appreciation of nature in new ways (Rousseau and Deschacht Citation2020).
Social prescriptions offer one mechanism to work outside of the standard biomedical concept of health, providing biopsychosocial person-centred care beyond the healthcare system and addressing risk factors for chronic and mental health conditions. Social prescriptions are defined as non-medical community referral approaches to connect individuals with community resources to support well-being and may offer a solution to address loneliness (Martino et al. Citation2015).
Although the concept is increasingly recognised worldwide (Morse et al. Citation2022, Litt et al. Citation2023a), its roots are strongest in the United Kingdom, where the National Health Service has adopted social prescribing as a creative way to relieve the pressure on health systems and leverage community resources to address the root causes of mental health conditions such as loneliness (Bickerdike et al. Citation2017). In the United Kingdom context, general practitioners are authorized to refer patients experiencing loneliness to community activities and voluntary services through social prescriptions. In Australia, one of the key recommendations from The Royal Commission report on Victoria’s Mental System was to establish community collectives in local regions to facilitate social connection and inclusion to reduce demand on and create an alternative to standard mental health services including social prescribing (Aggar et al. Citation2021, Sharman et al. Citation2022). In the Spanish region of Catalonia, social prescribing has been adopted to promote social participation. Since 2016, the Program Prescripció Social i Salut engages primary health care professionals to prescribe community activities to patients with emotional distress and low social support. Specific training for healthcare professionals (more than 1,900 professionals trained) and support to local social prescribing working groups, are some of the actions that have been shown to facilitate patients’ connections with community activities (Colom Farran et al. Citation2021).
Nature-based social prescribing (NBSP) represents one aspect of social prescribing that aims to address health and wellbeing by connecting people with nature-based activities and experiences that require active participation, are socially supported and generate meaning through these engagements (Leavell et al. Citation2019, Wood et al. Citation2022b, Astell-Burt et al. Citation2023). NBSP, if successful, can bridge the people, places, and institutions that make up strong social networks to access natural spaces and leverage these experiences to alleviate loneliness and promote quality of life (Leavell et al. Citation2019, Mygind et al. Citation2019, Coventry et al. Citation2021, Sachs et al. Citation2022b, Wood et al. Citation2022a).
The RECETAS project
In March 2021, we launched the European Commission funded project entitled ‘Reimagining Environments for Connection and Engagement: Testing Actions for Social Prescribing in Natural Spaces (RECETAS)’ to enhance the evidence base for addressing loneliness using community- based solutions. The premise of the project is that NBSP can reduce loneliness by engaging people in socially organized activities that are connected to the natural environment where they live, work and play (Bronfenbrenner Citation1979, Bandura Citation1986). It will develop, test, and evaluate interventions that include populations vulnerable to loneliness and who face obstacles to accessing and enjoying public space and group-based outdoor activities. Importantly, solutions tested in RECETAS will link nature-based solutions and green infrastructure with care professionals working inside and outside of local healthcare systems using co-created processes. It will strengthen the evidence examining the relationships between nature-based experiences and social connection to reduce loneliness and improve health-related quality of life.
The theoretical basis for the RECETAS project
The RECETAS approach draws on self-determination theory (Deci and Ryan Citation2017), social cognitive theory (Bandura Citation1986), and socioecological models (Bronfenbrenner Citation1979), focusing on factors that influence loneliness at multiple levels: intrapersonal, interpersonal, and environmental. Understanding intrapersonal processes is critical for combating loneliness. Community gardens provide an example of how NBSP may reduce loneliness and improve well-being. Research suggests that people who garden enjoy the smells, sounds, and feel of the garden (Hale et al. Citation2011). Feeling good originates from the self and links to the idea of intrinsic motivation, a core aspect of self-determination theory (Deci and Ryan Citation2012, Citation2017). Interventions based on what people love and how they feel are more likely to yield and sustain change (Ryan and Deci Citation2000, Litt et al. Citation2011, Citation2015, Citation2023b, Sachs et al. Citation2022a).
Social or interpersonal interactions can be influenced by nature-based experiences (Litt et al. Citation2015, Goldy and Piff Citation2020). Studies have shown that small regular group meetings and groups where members participate actively and are able to influence the content of group meetings are among the most effective interventions at reducing loneliness (Dickens et al. Citation2011, Reinhardt et al. Citation2021, Wakefield et al. Citation2022). When coupled with strong social organizations within the structure of the intervention (e.g. community gardens), social processes that are beneficial for reducing loneliness are strengthened, for example, by increasing opportunities for shared learning, relatedness, and social involvement (Masi et al. Citation2011, Jansson et al. Citation2018).
Environmental structures also influence human behaviors (Bronfenbrenner Citation1979). The design of our built environment and the areas where people live, work, and play are directly related to the amount of time people spend outdoors and how people interact with each other (Sallis et al. Citation2012). The layout of our communities, transportation infrastructure, and access to parks and trails either generate opportunities or obstacles for people to interact with NBSP. These attributes can include the presence or absence of parks (Razani et al. Citation2018), gardens (Hume et al. Citation2022), or farmers markets (Freedman et al. Citation2016). The quality and comfort of these settings also shapes the way in which the environment can facilitate health and wellbeing (van Dillen et al. Citation2012, Zijlema et al. Citation2020). Collectively, these individual, social and environmental processes reflect key pathways to well-being by creating opportunities for individuals to connect, to be active, to take notice, to keep learning, to share, to reciprocate, to feel needed, and to give.
Approaching loneliness and related health outcomes through a person-centred lens draws on the aforementioned theories and a systems-based, multisectoral, multicomponent, and multilevel preventive approach (Leavell et al. Citation2019, Prohaska et al. Citation2020). The RECETAS Consortium leverages social networks at the intersection of nature-based solutions and health care to support this approach and uses co-creation processes to inform the design of nature-based and socially-supported strategies to reduce loneliness and improve health-related quality of life (Aked and Thompson Citation2011). In this paper, we present a logic model to visualize the rationale and pathways by which the RECETAS initiative will address loneliness and generate impact through co-creation, stakeholder engagement, nature-based social intervention studies, health economic analyses and knowledge translation.
Material and methods
The logic model of the RECETAS project
We developed a logic model to illustrate the activities, outputs, and outcomes of the RECETAS initiative more clearly and illustrate how NBSP will influence health and wellbeing by presenting the components of the program and the basis for our evaluation. A logic model represents a standard tool in program evaluation designed at the beginning of a project to illustrate the shared relationships among the resources (inputs), activities, outputs, outcomes, and impact of a program (Frechtling Citation2007, Howarth et al. Citation2020) This model provides the foundation from which we will evaluate the reach, effectiveness, and impact of our actions. All RECETAS partners engaged in the development and review of the logic model to reflect local conditions, disciplinary contributions, and the collective vision for transforming research and innovation activities into outputs, outcomes, and longer-term impacts.
Results
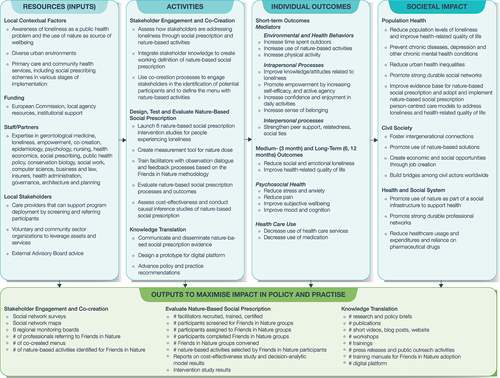
The RECETAS logic model is described here and illustrated in .
Figure 1. Logic model for the RECETAS approach to test nature-based social prescribing interventions to reduce loneliness and improve health-related quality of life (HRQoL).
Inputs
There are several key inputs that are critical for ensuring the success of RECETAS. These inputs are explained under four categories: local contextual factors, funding, staff/partners, and local stakeholders.
Local contextual factors
RECETAS targets diverse populations including people experiencing loneliness across different age groups, languages, socio-economic levels, ethnic groups, cultural contexts, climates, natural resources, and community assets. Each study site is working with particular groups known to be vulnerable to loneliness including, adults (18+) from socio-economically deprived areas (Barcelona), adults over 60 years who live at home and their caregivers (Prague and Cuenca, Ecuador), older adults living in assisted living facilities (Helsinki and Cuenca), immigrants, refugees, asylum seekers, and unemployed people (Marseille and Barcelona), and lesbian, gay, bisexual, trans, intersex, queer, asexual, other diverse sexual orientations, and gender identities (LGBTIQA+) refugees and asylum seekers (Melbourne). Each of the six cities will conduct an independent study and all interventions will follow the same protocol with adaptations relevant to the local context and target populations, as suggested by Kilgarriff and colleagues (Kilgarriff-Foster and O’Cathain Citation2015). Participants will be recruited from primary and social care settings, third-sector organizations, community groups, and volunteer organizations ().
Funding
The consortium was approved for funding by the European Commission through its Horizon 2020 funding research and innovative action (Agreement No. 945095) and the 2020 National Health and Medical Research Council (NHMRC-EU) Collaborative Research Grant (Agreement No. GNT2007059). The project commenced in March 2021 and will conclude in February 2026.
Staff/Partners
We have established a strong research and innovation foundation with 13 partners in nine countries and three continents (Europe, Australia, and South America). This partnership is highly interdisciplinary, bringing together experts in gerontology, loneliness science, empowerment, co-creation, epidemiology, psychology, nursing, health economics, social prescribing, public health policy, social work, architecture, planning, conservation biology, law, computer science, health insurance, and business. Moreover, these partners represent public, private and non-profit sectors, which provides a multi-sectoral framework for informing the design, implementation, and evaluation of the NBSP interventions.
Local stakeholders
In addition to our diverse set of partners engaged in RECETAS, our project is aligned with ongoing efforts at the local levels to provide person-centred care in each of our pilot cities. We will work closely with the network of care providers addressing loneliness at the community level. Additionally, we will engage voluntary and community sector organisations to leverage assets and services that may be part of the NBSP model tested within the RECETAS project. Collectively, this network of partners and stakeholders provides the capacity to identify, examine, and monitor trends and patterns of loneliness, enumerate nature-based resources in each respective RECETAS city and region, test social prescribing interventions, and inform all aspects of the RECETAS scope of work. RECETAS also draws on knowledge from our External Advisory Board, with expertise in nature-based solutions, business innovation and development, ethics, and equity.
Activities
The RECETAS project aims to understand the patterns and experience of loneliness and nature-based solutions to address these in cities, provide novel, participative, viable, and cost-effective solutions, and push the implementation of novel NBSP worldwide through knowledge translation. Stakeholder engagement, co-creation, and intervention deployment and evaluation will be central to achieving our planned outputs, outcomes, and long-term impacts.
Stakeholder engagement and co-creation
It is essential to develop solutions that reach vulnerable populations, promote resilience among community members in disadvantaged areas, and are available during critical episodes, such as the SARS-CoV-2 pandemic. With that in mind, the RECETAS project is informed by participatory processes and social network principles, with an emphasis on informing and engaging diverse multisectoral stakeholders in decision-making throughout the project. Target groups with whom we are cultivating relationships include health service providers, policymakers, decision makers, agency personnel, community and voluntary organizations, national and European policy makers, academic and other research entities, research and policy networks in Europe, Latin America and Australia, and the technology, business, finance, asset management and insurance sectors. The design of specific methodological tools and the evaluation of findings will be open to input from all stakeholders with a particular focus on engaging voluntary and community sector organizations oriented towards loneliness, mental health, and nature-based solutions. Such engagement will lead to informed decision-making and pathways to innovation. Moreover, the RECETAS project will further extend its reach through the European Urban Health Cluster, involving six projects funded under the Horizon 2020 topic SC1-BHC-29-2020, ‘Innovative actions for improving urban health and wellbeing -addressing environment, climate and socioeconomic factors’. The European Urban Health Cluster is fostering cooperation and coordination across ongoing initiatives on urban issues and health across the European Commission.
Social network analysis
Social network analytic methods are used to illustrate the ecosystem of socio-spatial resources (people, places, organizations, institutions, and policies) in each of the six cities that currently address loneliness and well-being through nature-based activities. Network science and social network analysis methods are a proven approach to understand a community ecosystem (Borgatti et al. Citation2009). The social network analysis involves several steps. First, research teams in each city identified and consulted with key local informants: Barcelona, Cuenca, Helsinki, Marseille, Melbourne, and Prague (see ). Additionally, each team conducted a review of the scientific and grey literature to identify practices and policies that have been used in each of the six cities. Additionally, the networks identified through this process were invited to participate in co-creation processes to create the specific menus of nature-based activities in each of the six cities. These stakeholders were also involved in local feasibility studies of the planned interventions and invited to support recruitment and retention of participants in the intervention studies.
Co-creation processes
Local stakeholders engaged through the social network analyses were invited to participate in co-creation to generate the menu for NBSP activities and test its feasibility with local actors (experts, technical and political staff, social organizations, and citizens) involved in each city project. The participatory approach elicits knowledge held by key stakeholders and facilitates the exchange of information to identify activities. Engaging a range of end-users to co-develop interventions increases the potential to achieve successful change because outputs are developed with local knowledge, expertise, and relationships in mind (Greenhalgh et al. Citation2016).
This co-creation process combines quantitative techniques, such as surveys, with qualitative techniques, such as individual or group interviews, participatory observations, community workshops, drawings, and community mapping exercises. During the co-creation process, participants collectively discuss and define a common understanding of the goals and crucial elements of RECETAS. Furthermore, participants learn about issues related to urban health, social assets, gender equality, nature-based solutions, loneliness, and social prescription. Moreover, the research team can learn about people’s preferences for nature contact, for example, where they go to experience nature and what they like to do when they are in a natural environment or what is missing in their everyday environments, as well as their perceptions of the availability, safety, and quality of nature-based solutions. Each team utilises similar participatory processes but adapts the techniques to reflect the demographic and social contexts in each pilot city.
Through these activities, each pilot city generates local NBSP menus that include a list and map of places, services, and activities available to study participants. These processes also inform the identification of intervention and evaluation indicators (both quantitative and qualitative). Indicators include mental health outcomes, social processes, participation levels, frequency, and intensity of nature use, experiences at each site, perceptions of inclusion, safety, belonging, awe, and so forth. The co-created menus and indicators represent the interests of different audiences (clinicians, provider services, group facilitators, and participant perspectives), and the indicators help track the impact of the interventions.
Design, test, and evaluate NBSP
The group intervention, Friends in Nature (FIN), is modified from the Circle of Friends (CoF) methodology developed by partners at the University of Helsinki (Pitkälä et al. Citation2009, Routasalo et al. Citation2009, Jansson et al. Citation2018) and is informed by the social network analyses, stakeholder perspectives, and co-creation processes. Central components of the intervention include one individual interview plus meetings in closed groups facilitated by two trained facilitators over a defined period (e.g. nine weeks). During week 1, all participants undergo a one-to-one interview or pre-focus group session with a pair of trained facilitators to get acquainted and to assess participants’ needs and wishes concerning the group process. Following this individual meeting, participants receive an empowerment letter and then begin the weekly intervention based on closed groups with activities aimed at promoting the accessibility and engagement with nature available in their city. During the group process, participants review ground rules and what makes a good group, reflect on their experiences of loneliness, build relationships, learn about loneliness alleviation, receive peer support, and participate in nature-based activities and excursions. As the group process progresses, the facilitators gradually step back and give power to the participants. Also, because cohorts come from different cultural and demographic backgrounds, the initial focus group meeting will adapt the approach to include an intercultural briefing. This briefing aims to improve communication and reduce misconceptions by raising awareness about differences in language, communication styles, and cultural conventions. Participants will be supported to develop authentic and lasting relationships by increasing awareness about other cultures and learning to connect across cultural barriers and communicate clearly. More generally, local adaptations to the FIN protocol can be made at each site to ensure the NBSP interventions are appropriate for the target cohort.
Those who receive the intervention will be guided to build supportive relationships and learn about the ways they can alleviate loneliness. Moreover, the group will learn about nature-based activities and share their experiences and interests. Participants are expected to develop new social ties and enhance their self-efficacy and sense of active agency in their lives to cope with and alleviate loneliness. Through the group process, the participants will increase their social support and emotional wellbeing as they participate in socially supported nature-based activities, learn more about the local nature-based and social resources near where they live, and increase their understanding of how nature can influence wellbeing and social relationships.
The intervention study methods will vary by city. We will use randomized controlled trials in Barcelona, Helsinki, and Prague and pre-post intervention studies in Cuenca, Marseille, and Melbourne. Registration for the trials occurred in 2022. Trial registration numbers: Barcelona Trial: NCT05488496; Prague Trial: NCT05522140; Helsinki Trial: NCT05507684. The dual approaches to research reflect the needs and desires of our respective partners and their recommendations for which methodologies are appropriate for the communities with whom they work.
For the three randomized controlled trials (RCTs), individuals will be randomly allocated to the intervention arm or usual care (control arm). For the intervention arm, individuals will undergo the following steps. First, they will be assigned to a closed group located conveniently for the participant. Two trained facilitators will be assigned to each group facilitating discussion and feedback among group members and making better use of group dynamics. Second, an interview or pre-focus group session with facilitator(s) will be scheduled to build trust in participants. Facilitators will support the group dynamics by fostering empowerment and independence from the facilitator. The group-based sessions will follow, including 5-12 persons per group, with an average of 8 groups in the three trial cities with a goal to recruit and randomize 316 participants per city. These groups will include participants from the same local area who will get to know each other through social opportunities and participation in nature-based activities available in their respective communities during nine sessions. Participants’ preferences and a collaborative mapping of nature-based community assets (as part of the co-creation process described earlier) will guide the group to the activities that they want to explore using the co-created menu as the starting point. Participants will receive phone and text reminders, information about the nature-based activities, and prompts to evaluate their experiences after each activity through a short questionnaire. Participants in the control group will receive usual care, which is the co-created menu including a map with a list of nature-based resources in the city area. Professionals will recommend specific assets according to the participant’s characteristics and preferences. Usual care is the appropriate comparison rather than a placebo for this complex intervention (O’Cathain et al. Citation2019). Expected sample sizes in each of the RCT studies is 316, for a total of 948 participants across the three studies. A protocol detailing the RCTs is described elsewhere (Coll-Planas et al. Citation2023).
Non-controlled exploratory complex intervention studies with a pre – post design, with one-year follow-up will be conducted in Cuenca (Ecuador), Marseille (France) and Melbourne (Australia). The three sites will apply the same intervention framework described above and tailor it to the local context and the target population. Expected sample sizes in each of the non-RCT studies is 50-75, for a total of 150-225 participants across the three studies.
Measurement of nature dose
Key to understanding the mechanisms linking different NBSP activities to wellbeing will be the characterization of the natural environment for each of the nature-based activities and how participants experience nature (Bratman et al. Citation2019, Marselle Citation2019). Different natural space designs and nature experiences can deliver diverse benefits with respect to wellbeing. For example, higher levels of species diversity in parks have been linked to improved mental wellbeing benefits (Cameron et al. Citation2020); different sensory experiences such as sounds, smells and tactile sensations have a variety of pathways to wellbeing (Franco et al. Citation2017) and the participant experience can also affect wellbeing, from adventure-based activities to seated relaxation (Mygind et al. Citation2019).
We will use in-group assessments and objective audits to characterize three components of the nature experience that have previously been linked to mental wellbeing. First, the actual biodiversity of the natural space will be recorded by trained auditors. Actual species diversity will be characterized as the number of species present and their functional characteristics, for example, the species richness and abundance of street trees in a park (Marselle Citation2019). Data will be derived from fieldwork, remote sensing, or existing surveys of the environment in which the intervention takes place. Additionally, short questionnaires will be administered each week, following the group session. In that questionnaire, we will ask about 1) perceived biodiversity, which will measure the biodiversity people think is at a location (Cameron et al. Citation2020); 2) exposure to nature, which will be recorded as a measure of the time and/or proximity to nature during the intervention; and 3) the type of nature experience, which will be measured as either incidental (e.g. observing nature on a walk), or experiential (e.g. planting trees).
Design and disseminate facilitator training program
The role of facilitators is central to the FIN intervention, and their training is a key contribution of the project. Specifically, the facilitator training program is informed by the CoF methodology (Pitkälä et al. Citation2009, Routasalo et al. Citation2009, Jansson et al. Citation2018). On average, facilitators will participate in five one-day workshops over a 5-month period. During the training, facilitators receive mentorship to support the facilitation. They will write a learning diary of each group meeting, and mentors will give supportive feedback for the facilitators, based on the diaries and progression of the group process. The facilitators will learn about the intervention group model, loneliness and its alleviation, group processes and dynamics, how to plan the FIN group, and how to interview group participants. The training is informed by reflective and active learning cycles, beginning with a vignette presentation and then will continue with thematic café group style discussions delving into facilitators’ experiences of the different topics (Kolb et al. Citation2014). From these experiences and trainer feedback, facilitators will form their own integrated knowledge based on theory, personal experience, and active reflection (Pitkälä et al. Citation2004, Jansson et al. Citation2018). This model, if successful, will be disseminated beyond the RECETAS studies to support NBSP and the integration of a group-based model with trained facilitators to support its implementation, including the diffusion of the FIN model to local practitioners.
Evaluate NBSP interventions
All randomized participants will be included in intention-to-treat analyses. We will compute statistical comparisons between the groups using t-tests, Mann Whitney U tests, or Chi-Square tests when appropriate. Repeated measures will be analysed using mixed models, with appropriate distribution and link functions, and an unstructured correlation structure, with treatment groups, time, and their interactions as fixed factors. In addition to the intention-to-treat analysis, a causal inference-based per-protocol analysis will be performed as a sensitivity analysis using a structural nested model with g-estimation (Hernán and Robins Citation2017, Latimer et al. Citation2020). Several secondary and subgroup analyses will be performed (e.g. for stage of dementia, type of loneliness, etc.) to identify effect modification.
Ethnography, focus groups, interviews, reflections, and photo elicitation will be used across pilot cities to engage participants and evaluate how program participants experienced the interventions. This mixed-methods approach is particularly beneficial when studying complicated social interactions and processes that are difficult to document in a survey or laboratory. Focus groups will be useful to gather in-depth information on participants’ attitudes, opinions, and experiences linked to a certain issue (Wilson Citation2012). These group-based reflections offer a technique for looking at and assessing one’s own experiences, ideas, and emotions in relation to the NBS interventions. Additionally, to spark conversation and elicit thoughts and experiences from research participants, photo elicitation will be used to incorporate images or other visual elements obtained by participants. In general, photo elicitation is a helpful research technique for delving into sensitive and difficult subjects as well as for getting a more holistic and engaging understanding of participants’ experiences and opinions (Reavey Citation2012).
Cost-effectiveness studies
To evaluate the long-term benefit-harm and cost-effectiveness relations, we will develop a decision-analytic model systematically integrating short- and long-term evidence on all consequences. This approach allows us to create the specific pathway for each intervention, to use multiple sources for the population of the model with input parameters, to account for uncertainty, and to predict and compare patient- and society-relevant long-term consequences (Kuntz et al. Citation2013). The model will be sufficiently complex to integrate relevant health states and outcomes but also simple enough to ensure its face validity and feasibility, to enhance transparency and to communicate its results and health policy recommendations to lay persons, health professionals and health policy decision makers. Finally, the model will be validated and analysed. Evaluated outcomes will include life expectancy, quality-adjusted life expectancy, costs, and incremental cost-effectiveness ratios. Social prescribing’s complexity suggests that we undertake attribution, displacement, and deadweight analysis. To test the robustness of our model and the influence of uncertain parameters on the results, we will perform comprehensive uncertainty analyses.
Knowledge translation
Communicate and disseminate NBSP evidence to inform policy and practice
The RECETAS team will use the evidence generated through its research activities to advance policy recommendations through briefs, workshops, and protocols of interventions. Furthermore, it will develop health policy recommendations drawing largely from its intervention studies, innovative causal inference analyses, and decision-analytic modelling results. Additionally, a calendar of strategic events will be created along with a talk series about social connections in partner cities in coordination with local authorities and other stakeholders to share research findings and lessons learned. Policy roundtables targeting different levels of stakeholders (local communities, local government, the European Commission, urban platforms, and advocacy groups) will be convened to contemplate NBSP implementation on a broader scale and the linkage between social prescribing and nature-based solutions to address loneliness. Finally, curated art exhibits, produced by participants, and radio spotlights in the six cities will be leveraged to showcase stories from participants engaged in RECETAS.
Develop prototype for a digital platform
A digital platform will be designed and prototyped to support NBSP by connecting helping professionals, third sector organizations, and individuals who experience loneliness and/or seek ways to connect with others outdoors in safe, respectful, and meaningful ways. The primary function of the platform will be to make matches between users and activities that are based on user-generated data about likes and dislikes as they relate to social experiences, hobbies, time spent outdoors and so forth. The digital platform will be important in the implementation of NBSP beyond the RECETAS studies. It will be designed for people who want to connect online and who desire in-person experiences and for prescribing professionals to standardize the approach, track processes and outcomes related to prescribing, and facilitate patient participation in NBSP programs.
Outputs
In relation to the activities of the RECETAS consortium, the outputs represent early measures for impact related to stakeholder engagement, intervention implementation, and knowledge translation. As a result of the project, we will quantify the number of stakeholders engaged in the different phases of the project and the experiences of these stakeholders as they interface with the project activities. We will monitor the number of facilitators recruited and trained in the FIN intervention, the number of participants screened, consented, and retained in the FIN groups, the number of groups organized for FIN, the number of referrals over time by care providers, the number of menus created and disseminated in study neighbourhoods and beyond, the adoption of these programs following the end of the interventions, the number and types of nature-based activities supporting the FIN interventions, and the production of FIN training materials. Moreover, knowledge translation will be seminal to extending program reach and amplifying impact. We will use a diverse set of tools to communicate and disseminate the RECETAS outputs and outcomes including, but not limited to, research publications and presentations, research, and policy briefs to highlight key findings and recommendations, social media posts, including blogs and short videos, workshops, trainings, and policy summits.
Outcomes
The RECETAS project will capture individual-level changes at three-, six- and 12-months post intervention and longer-term impacts related to health, society, economy, programmes, and policy. These outcomes and impacts are referenced in and described below.
Individual outcomes
Outcomes will be informed by quantitative assessments and the qualitative inquiry including interviews, direct observations, and photo elicitation to explore the perceived experiences of participants and professionals involved and triangulate this information, which will be elicited from study participants, group facilitators, and medical records. Specifically, these data will capture perceived impacts and the mechanisms underlying the differences found in loneliness between intervention and usual care arms, and to assess maintenance of outcome changes over time. We will also seek to examine how participants currently understand loneliness and experience access and barriers to NBS within urban spaces. Motivation and contextual issues for participation, time spent in NBS, and mental well-being will be assessed.
The main quantitative outcomes shared by the six studies of the NBSP studies are loneliness as measured by the De Jong Gierveld Loneliness Scale (Gierveld and Tilburg Citation2006) and health-related quality of life as measured by the 15 D scale (Sintonen Citation2001). Secondary outcomes will vary according to the study and population and will measure psychosocial health (e.g. increased subjective wellbeing, improved mood, cognition, reduced stress, anxiety, and depression, and reduced pain); environmental and health behaviours (e.g. increased physical activity, increased time spent outdoors, and increased use of NBS); intrapersonal processes (e.g. increased knowledge, attitudes, and beliefs related to the alleviation of loneliness; increased awareness of nature, increased self-efficacy and active agency; increased confidence and enjoyment; and increased sense of belonging); and interpersonal processes (e.g. increased peer support, relatedness, and social ties).
Societal impacts
RECETAS is a full chain project that includes a deep understanding of the health challenges due to rising levels of loneliness in the population, and the need for a collaborative design, testing, and evaluation of solutions and policy and exploitation tools to ensure the embedding and sustainability of solutions in Europe and beyond. Through a strengthened evidence base, strong and expansive partnerships, science translation for policy and practice, and investments in digital technological solutions, RECETAS will be positioned to generate a range of impacts across health, social, economic, policy, and environmental domains and ultimately advance the adoption and implementation of NBSP as a solution to address loneliness and as a legitimate health investment.
Population health
If successful, the RECETAS approach will lead to reductions in loneliness and improvements in health-related quality of life as well as related physical and mental health conditions. Additionally, through NBSP, participants will increase connections and strengthen social ties. Moreover, because of NBSP, communities will have a cost-effective and accessible way to promote the use of nature as an antidote to loneliness and related health conditions.
Through the deployment of NBSP, local and regional health systems can have the potential to spark economic and social opportunities through job creation by creating a new line of trained professionals to facilitate NBSP peer groups. Moreover, such an approach will have the potential to reduce urban health inequalities in the treatment and management of loneliness. NBSP may reduce barriers to the access of innovative healthcare solutions and natural environments.
The RECETAS Consortium will promote strong and durable social networks working at the nexus of mental well-being and nature-based solutions. As a result of RECETAS, we will engage voluntary and community sector organizations to ensure that the co-design, delivery, and scale-up of interventions to address loneliness are more inclusive of marginalized communities. Such solutions should enhance community resilience, particularly in disadvantaged urban areas and more generally during critical health-related episodes. Moreover, we will work with our networks of stakeholders to link research with practice and policy and foster city-to-city learning about NBSP, enabling citizens, providers, and decision makers to optimally implement and scale-up NBSP interventions.
Civil society
NBSP, adopted and implemented widely, has the potential to connect people to non-medical resources in the voluntary and community sectors to meet the needs of individuals beyond the capacity of local health systems. Building community capacity is essential to meeting individual needs. By combining community engagement and co-creation, organizational change, and individual-level practice, localities will be on a trajectory to improve both community and individual health and wellbeing. The RECETAS model recognises the reciprocity between individuals and community and the need to strengthen local capacity to connect individuals with community-based resources at the theoretical, policy and practice levels. For NBSP to work, it should recognise the inherent role of civil society organisations in the design and delivery of NBSP-related programs and practices and the need for financing of these activities to ensure voluntary and community sector participation over time. The involvement of such organisations can promote the needed intergenerational connections necessary for a less lonely society across the lifespan, engagement with nature-based solutions to alleviate loneliness and promote wellbeing, create economic and social opportunities through job creation among third-sector organisations, and build bridges among civil actors worldwide.
Health and social systems
The evidence generated in RECETAS will inform policy and practice related to reducing loneliness and improving health-related quality of life and in doing so, reduce health care usage, promote cost effective interventions, and avoid unnecessary costs. The methodologies and programmes developed in RECETAS will be disseminated to ensure that health systems more broadly can monitor programmatic implementation and evaluation by tracking chronic comorbidities, medications, use of medical services, quality-of-life, life expectancy, and costs. The benefit-harm analysis and cost-effectiveness analysis will inform our understanding of the short- and long-term health, social and economic impacts of these interventions, drawing on the indicators to be collected and assessed (Siebert Citation2003, Siebert et al. Citation2012). Additionally, social value analyses including the application of well-being scales will be explored to understand the social return on NBSP investments (Kimberlee Citation2018).
Discussion
This logic model provides a holistic view of the RECETAS project and the ways in which RECETAS will make a significant and needed contribution to the evidence base about nature-based social prescribing and the prevention and treatment of loneliness (Husk et al. Citation2019). Details about each study will be examined in subsequent manuscripts. The main objective of the RECETAS project is to devise, validate, and leverage solutions that address loneliness through nature-based social prescribing, by linking nature-based solutions and green infrastructure with care professionals working inside and outside of local healthcare systems. We will deploy a mixed methods approach to allow for a robust implementation and evaluation of nature-based social prescribing in diverse settings. These methods should lead to validation of the effectiveness of nature-based social prescribing (including identification of the economic burden associated with nature-based social prescribing) in supporting populations at risk of loneliness and reduced health-related quality of life via engagement in socially oriented opportunities in safe, inclusive, and accessible green and blue outdoor urban spaces (Husk et al. Citation2019, Leavell et al. Citation2019, Fixsen and Barrett Citation2022, Griffiths et al. Citation2022, Sandhu et al. Citation2022).
Strengths and limitations
RECETAS will address loneliness, a growing public health concern in diverse contexts among diverse populations by promoting a holistic approach to care and improving the alleviation of loneliness in an affordable and accessible way. RECETAS will strengthen the evidence base for nature-based solutions to address loneliness by employing randomised controlled trials and cost-benefit analyses to test intervention effectiveness. The initiative is rooted in co-creation processes that will be used to inform the design of the interventions and their evaluations, increasing acceptability among stakeholders and participants, and thus expediting and facilitating implementation and improving conditions for dissemination and diffusion of study findings and intervention best practices. Given the taboo associated with people identifying as lonely, recruitment and retention may be difficult, which may affect study sample size and study power to evaluate intervention effectiveness. However, the co-creation processes will identify and address these concerns in the design and implementation of the nature-based social prescribing interventions, offsetting the potential limitations related to the stigma of loneliness.
Conclusion
Nature-based social prescribing represents a low-cost, creative means to strengthen social networks, reduce stress, and facilitate social connectedness among participants and providers in cities. We believe that investments in nature-based social prescribing will lead to improved urban health and well-being by promoting aesthetic experiences, increasing active citizenship, strengthening neighbourhood ties, and fostering social connections across diverse social and economic groups. Such interventions will leverage social processes that are critical to improving social support and fostering and sustaining behaviour changes necessary to reduce loneliness and improve health-related quality of life. Such changes present important targets for improving mental well-being and physical health and will inform urban policy, planning, and practice-based actions to promote benefits beyond the reach of the RECETAS communities.
Acknowledgements
On behalf of the entire RECETAS consortium we thank each partner for their contributions to the development of this project. A special acknowledgement to Ms. Laura Hidalgo of the Barcelona Institute for Global Health for assistance in the graphic design of the logic model.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Kaisu H. Pitkälä
The authors contributing to this manuscript represent the core membership of the RECETAS Consortium. The authors bring together a vast array of experience and technical backgrounds ranging from, but not limited to, medicine, public health, epidemiology, psychology, anthropology, sociology, nursing, conservation biology, architecture, planning, law, business, urban policy, and knowledge translation. The RECETAS partners represent academia, government, third-sector organizations, technological and business sectors.
All authors contributed to the preparation of the manuscript. JSL, LCP, and ALS drafted this manuscript based on the grant proposal conceived and written by JSL, LCP, SBA, AC, RK, SG, SB, KJ, GG, US, UR, KP, AJ, CD, JC, and DV. All the authors made contributions to the methods section of the manuscript and reviewed the entire manuscript. Specifically, JSL and LCP constructed the logic model; DV, AB, KB prepared the social network analysis section; MG, SBA, GG, JA, SB, KJ, NH and NO prepared the co-creation and menu development section; LCP, SBA, KP, AJ, VD, and AB prepared the Intervention Studies section; ALS, SB, NH, NO, and KJ prepared the nature dose section, US, UR, and RK prepared the health Economics section, VD, ALS, MK, IH, drafted the discussion. All authors read and approved the final manuscript.
References
- Aggar, C., et al., 2021. Social prescribing for individuals living with mental illness in an Australian community setting: a pilot study. Community mental health journal, 57 (1), 189–195. doi:10.1007/s10597-020-00631-6.
- Aked, J. and Thompson, S., 2011. Five ways to wellbeing: new applications, new ways of thinking. London: New Economics Foundation.
- Astell-Burt, T., et al., 2023. Need and interest in nature prescriptions to protect cardiovascular and mental health: a nationally-representative study with insights for future randomised trials. Heart, lung and circulation, 32 (1), 114–123. doi:10.1016/j.hlc.2022.11.008.
- Australian Institute of Health and Welfare, 2021. Social isolation and loneliness. Canberra: Australian Institute of Health and Welfare.
- Bandura, A., 1986. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall.
- Bickerdike, L., et al., 2017. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. British medical journal open, 7 (4), e013384. doi:10.1136/bmjopen-2016-013384.
- Borgatti, S.P., et al., 2009. Network analysis in the social sciences. Science, 323 (5916), 892–895. doi:10.1126/science.1165821.
- Bratman, G.N., et al., 2019. Nature and mental health: an ecosystem service perspective. Science advances, 5 (7), eaax0903–eaax0903. doi:10.1126/sciadv.aax0903.
- Bronfenbrenner, U., 1979. The ecology of human development. Cambridge, MA: Harvard University Press.
- Brooks, S.K., et al., 2020. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet, 395 (10227), 912–920. doi:10.1016/S0140-6736(20)30460-8.
- Cameron, R.W., et al., 2020. Where the wild things are! Do urban green spaces with greater avian biodiversity promote more positive emotions in humans? Urban ecosystems, 23 (2), 301–317. doi:10.1007/s11252-020-00929-z.
- Cigna, 2018. Cigna US loneliness index: survey of 20,000 Americans examining behaviors driving loneliness in the United States. Cigna, 1–61.
- Coll-Planas, L., et al., 2023. RECETAS: Rationale and design of nature-based social interventions to address loneliness: A protocol for multi-city randomized controlled trials of RECETAS in Barcelona, Spain, Helsinki, Finland, and Prague, Czech Republic. BMC Public Health, 24 (1); DOI: 10.1186/s12889-023-17547-x.
- Colom Farran, J., et al., 2021. Guia de Prescripció d’actius comunitaris: Programa Prescripció Social i Salut (PSS). Barcelona, Spain: Agència de Salut Publica de Catalunya.
- Coventry, P.A., et al., 2021. Nature-based outdoor activities for mental and physical health: systematic review and meta-analysis. SSM - population health, 16, 100934. doi:10.1016/j.ssmph.2021.100934.
- d’Hombres, B., et al., 2019. Loneliness across Europe—an unequally shared burden in Europe. Belgium: European Commission.
- Deci, E. and Ryan, R., 2017. Self-determination theory: basic psychological needs in motivation, development, and wellness. New York: Guildford Press.
- Deci, E.L. and Ryan, R.M., 2012. Self-determination theory in health care and its relations to motivational interviewing: a few comments. International journal of behavioral nutrition and physical activity, 9 (1), 1–6. doi:10.1186/1479-5868-9-24.
- Dickens, A.P., et al., 2011. Interventions targeting social isolation in older people: a systematic review. BMC public health, 11 (1), 647. doi:10.1186/1471-2458-11-647.
- Figueira, C., et al., 2022. Opinions and LIfestyle survey: public opinions and social trends, Great Britain: 27 April to 8 May 2022. UK: Office of National Statistics.
- Fixsen, A. and Barrett, S., 2022. Challenges and approaches to green social prescribing during and in the aftermath of COVID-19: a qualitative study. Frontiers in psychology, 13. doi:10.3389/fpsyg.2022.861107.
- Franco, L.S., Shanahan, D.F., and Fuller, R.A., 2017. A review of the benefits of nature experiences: more than meets the eye. International journal of environmental research and public health, 14 (8), 864. doi:10.3390/ijerph14080864.
- Frechtling, J., 2007. Logic modeling methods in program evalaution. San Francisco, CA: Jossey-Bass.
- Freedman, D.A., et al., 2016. Systematic review of factors influencing farmers’ market use overall and among low-income populations. Journal of the academy of nutrition and dietetics, 116 (7), 1136–1155. doi:10.1016/j.jand.2016.02.010.
- Gierveld, J.D.J. and Tilburg, T.V., 2006. A 6-item scale for overall, emotional, and social loneliness: confirmatory tests on survey data. Research on aging, 28 (5), 582–598. doi:10.1177/0164027506289723.
- Goldy, S.P. and Piff, P.K., 2020. Toward a social ecology of prosociality: why, when, and where nature enhances social connection. Current opinion in psychology, 32, 27–31. doi:10.1016/j.copsyc.2019.06.016.
- Greenhalgh, T., et al., 2016. Achieving research impact through co‐creation in community‐based health services: literature review and case study. The Milbank quarterly, 94 (2), 392–429. doi:10.1111/1468-0009.12197.
- Griffiths, C., Hina, F., and Jiang, H., 2022. Social prescribing through primary care: a systematic review of the evidence. Open journal of preventive medicine, 12 (2), 31–58. doi:10.4236/ojpm.2022.122003.
- Hale, J., et al., 2011. Connecting food environments and health through the relational nature of aesthetics: gaining insight through the community gardening experience. Social Science & Medicine, 72 (11), 1853–1863. doi:10.1016/j.socscimed.2011.03.044.
- Hawkley, L.C. and Cacioppo, J.T., 2010. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Annals of behavioral medicine, 40 (2), 218–227. doi:10.1007/s12160-010-9210-8.
- Hernán, M.A. and Robins, J.M., 2017. Per-protocol analyses of pragmatic trials. The new England journal of medicine, 377 (14), 1391–1398. doi:10.1056/NEJMsm1605385.
- Holt-Lunstad, J., 2017. The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public policy & aging report, 27 (4), 127–130. doi:10.1093/ppar/prx030.
- Howarth, M., et al., 2020. What is the evidence for the impact of gardens and gardening on health and well-being: a scoping review and evidence-based logic model to guide healthcare strategy decision making on the use of gardening approaches as a social prescription. British medical journal open, 10 (7), e036923. doi:10.1136/bmjopen-2020-036923.
- Hume, C., et al., 2022. Community gardens and their effects on diet, health, psychosocial and community outcomes: a systematic review. BMC public health, 22 (1), 1247. doi:10.1186/s12889-022-13591-1.
- Husk, K., et al., 2019. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health & social care in the community. doi:10.1111/hsc.12839.
- Jansson, A. and Pitkälä, K., 2021. Loneliness is a serious risk in COVID-19 lockdown. European geriatric medicine, 12 (3), 663–664. doi:10.1007/s41999-021-00466-8.
- Jansson, A.H., Savikko, N.M., and Pitkälä, K.H., 2018. Training professionals to implement a group model for alleviating loneliness among older people–10-year follow-up study. Educational gerontology, 44 (2–3), 119–127. doi:10.1080/03601277.2017.1420005.
- Kilgarriff-Foster, A. and O’Cathain, A., 2015. Exploring the components and impact of social prescribing. Journal of public mental health, 14 (3), 127–134. doi:10.1108/JPMH-06-2014-0027.
- Killgore, W.D., et al., 2020. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry research, 290, 113117. doi:10.1016/j.psychres.2020.113117.
- Kimberlee, R., 2018. Whither social prescribing? Journal of holistic healthcare, 15 (3), 1–3.
- Kolb, D.A., Boyatzis, R.E., and Mainemelis, C., 2014. Experiential learning theory: previous research and new directions. In: R.J. Sternberg and L. Zhang, eds. Perspectives on thinking, learning, and cognitive styles . New York: Routledge, 227–248.
- Kuntz, K., et al., 2013. Decision and simulation modeling alongside systematic reviews. In: Decision and simulation modeling in systematic reviews [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US).
- Latimer, N., et al., 2020. Improved two-stage estimation to adjust for treatment switching in randomised trials: g-estimation to address time-dependent confounding. Statistical methods in medical research, 29 (10), 2900–2918. doi:10.1177/0962280220912524.
- Leavell, M., et al., 2019. Nature-based social prescribing in urban settings to improve social connectedness and mental wellbeing: a review. Current environmental health reports, 6 (November), 297–308.
- Litt, J., et al., 2023a. Current trends and future directions in urban social prescribing. Current environmental health reports. doi:10.1007/s40572-023-00419-2.
- Litt, J., et al., 2023b. The effects of a community gardening intervention on diet, physical activity, and anthropometry outcomes: a two-arm, observer-blind, randomised controlled trial (CAPS trial). The lancet planetary health, 7 (1), 1–13. doi:10.1016/S2542-5196(22)00303-5.
- Litt, J.S., et al., 2015. Exploring ecological, emotional and social levers of self-rated health for urban gardeners and non-gardeners: a path analysis. Social science & medicine, 144 (November), 1–8. doi:10.1016/j.socscimed.2015.09.004.
- Litt, J.S., et al., 2011. The influences of social involvement, neighborhood aesthetics and community garden participation on fruit and vegetable consumption. The American journal of public health, 101 (8), 1466–1473. doi:10.2105/AJPH.2010.300111.
- Luanaigh, C.Ó. and Lawlor, B.A., 2008. Loneliness and the health of older people. International journal of geriatric psychiatry, 23 (12), 1213–1221. doi:10.1002/gps.2054.
- Marselle, M., 2019. Theoretical foundations of biodiversity and mental well-being relationships. Environment international, 133–158.
- Martino, J., Pegg, J., and Frates, E.P., 2015. The connection prescription: using the power of social interactions and the deep desire for connectedness to empower health and wellness. American journal of lifestyle medicine, 11 (6), 466–475. doi:10.1177/1559827615608788.
- Masi, C.M., et al., 2011. A meta-analysis of interventions to reduce loneliness. Personality and social psychology review, 15 (3), 219–266. doi:10.1177/1088868310377394.
- Mind, 2018. 40 per cent of all GP appointments about mental health. London: Mind.
- Morse, D., et al., 2022. Global developments in social prescribing. BMJ global health, 7 (5), e008524. doi:10.1136/bmjgh-2022-008524.
- Moustakas, C.E., 2016. Loneliness. Pickle Partners Publishing.
- Murthy, V.H., 2020. Together. New York, NY: Harper Collins Publishers.
- Mygind, L., et al., 2019. Immersive nature-experiences as health promotion interventions for healthy, vulnerable, and sick populations? A systematic review and appraisal of controlled studies. Frontiers in psychology, 10 (943). doi:10.3389/fpsyg.2019.00943.
- National Academies of Sciences E, Medicine, 2020. Social isolation and loneliness in older adults: opportunities for the health care system. Washington, DC: The National Academies Press.
- Naylor, C., et al., 2020. Mental health and primary care networks. London: The King’s Fund.
- O’Cathain, A., et al., 2019. Guidance on how to develop complex interventions to improve health and healthcare. British medical journal open, 9 (8), e029954. doi:10.1136/bmjopen-2019-029954.
- Palgi, Y., et al., 2020. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. Journal of affective disorders, 275, 109. doi:10.1016/j.jad.2020.06.036.
- Pitkälä, K.H., et al., 2004. Leading groups of older people: a description and evaluation of the education of professionals. Educational gerontology, 30 (10), 821–833. doi:10.1080/03601270490507268.
- Pitkälä, K.H., et al., 2009. Effects of psychosocial group rehabilitation on health, use of health care services, and mortality of older persons suffering from loneliness: a randomized, controlled trial. Journals of gerontology: series A, 64A (7), 792–800. doi:10.1093/gerona/glp011.
- Prohaska, T., et al., 2020. Consensus statement: loneliness in older adults, the 21st century social determinant of health? British medical journal open, 10 (8), e034967. doi:10.1136/bmjopen-2019-034967.
- Razani, N., et al., 2018. Effect of park prescriptions with and without group visits to parks on stress reduction in low-income parents: SHINE randomized trial. PLoS one, 13 (2), e0192921. doi:10.1371/journal.pone.0192921.
- Reavey, P., 2012. Visual methods in psychology: using and interpreting images in qualitative research. New York: Routledge.
- Reinhardt, G.Y., Vidovic, D., and Hammerton, C., 2021. Understanding loneliness: a systematic review of the impact of social prescribing initiatives on loneliness. Perspectives in public health, 141 (4), 204–213. doi:10.1177/1757913920967040.
- Rousseau, S. and Deschacht, N., 2020. Public awareness of nature and the environment during the COVID-19 crisis. Environ resour econ (Dordr), 76 (4), 1–11. doi:10.1007/s10640-020-00445-w.
- Routasalo, P.E., et al., 2009. Effects of psychosocial group rehabilitation on social functioning, loneliness and well‐being of lonely, older people: randomized controlled trial. Journal of advanced nursing, 65 (2), 297–305. doi:10.1111/j.1365-2648.2008.04837.x.
- Ryan, R.M. and Deci, E.L., 2000. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American psychologist, 55 (1), 68–78. doi:10.1037/0003-066X.55.1.68.
- Sachs, A., et al., 2022a. “To me, it’s just natural to be in the garden”: a multi-site investigation of new community gardener motivation using self-determination theory. Wellbeing, space and society, 100088. doi:10.1016/j.wss.2022.100088.
- Sachs, A.L., et al., 2022b. Rationale, feasibility, and acceptability of the Meeting in Nature Together (MINT) program: a novel nature-based social intervention for loneliness reduction with teen parents and their peers. International journal of environmental research and public health, 19 (17), 11059. doi:10.3390/ijerph191711059.
- Sallis, J.F., et al., 2012. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation, 125 (5), 729–737. doi:10.1161/CIRCULATIONAHA.110.969022.
- Sandhu, S., Alderwick, H., and Gottlieb, L.M., 2022. Financing approaches to social prescribing programs in England and the United States. The Milbank quarterly, 100 (2), 393–423. doi:10.1111/1468-0009.12562.
- Sharman, L.S., et al., 2022. Social prescribing link workers—A qualitative Australian perspective. Health & social care in the community, 30 (6). doi:10.1111/hsc.14079.
- Siebert, U., 2003. When should decision-analytic modeling be used in the economic evaluation of health care? The European journal of health economics, formerly: HEPAC, 4 (3), 143–150. doi:10.1007/s10198-003-0205-2.
- Siebert, U., et al., 2012. State-transition modeling: a report of the ISPOR-SMDM modeling good research practices task force–3. Medical decision making, 32 (5), 690–700. doi:10.1177/0272989X12455463.
- Sintonen, H., 2001. The 15D instrument of health-related quality of life: properties and applications. Annals of medicine, 33 (5), 328–336. doi:10.3109/07853890109002086.
- van Dillen, S.M.E., et al., 2012. Greenspace in urban neighbourhoods and residents’ health: adding quality to quantity. Journal of epidemiology & community health, 66 (6), e8. doi:10.1136/jech.2009.104695.
- Victor, C.R., 2015. Loneliness and later life: concepts, prevalence, and consequences. In: A. Sha’ked and A. Rokach, eds. Addressing loneliness. New York: Psychology Press, 207–226.
- Victorian Health Promotion Foundation SUoT, 2019. The Young Australian Loneliness Survey: understanding loneliness in adolescence and young adulthood. Victoria, Australia.
- Wakefield, J.R.H., et al., 2022. Social prescribing as ‘social cure’: a longitudinal study of the health benefits of social connectedness within a social prescribing pathway. Journal of health psychology, 27 (2), 386–396. doi:10.1177/1359105320944991.
- Weiss, R., 1975. Loneliness: the experience of emotional and social isolation. Cambridge, MA: MIT press.
- Wilson, V., 2012. Research methods: interviews. Evidence based library and information practice, 7 (2), 96–98. doi:10.18438/B89P5B.
- Wood, C.J., et al., 2022b. Therapeutic community gardening as a green social prescription for mental Ill-health: impact, barriers, and facilitators from the perspective of multiple stakeholders. International journal of environmental research and public health, 19 (20), 13612. doi:10.3390/ijerph192013612.
- Wood, C.J., Barton, J.L., and Wicks, C.L., 2022a. The impact of therapeutic community gardening on the wellbeing, loneliness, and life satisfaction of individuals with mental illness. International journal of environmental research and public health, 19 (20), 13166. doi:10.3390/ijerph192013166.
- Yang, K. and Victor, C., 2011. Age and loneliness in 25 European nations. Ageing & society, 31 (8), 1368–1388. doi:10.1017/S0144686X1000139X.
- Yeginsu, C., 2018. Britain tackles loneliness. The New York Times, 17 Jan.
- Zavaleta, D., Samuel, K., and Mills, C.T., 2017. Measures of social isolation. Social indicators research, 131 (1), 367–391. doi:10.1007/s11205-016-1252-2.
- Zijlema, W.L., et al., 2020. Understanding correlates of neighborhood aesthetic ratings: a European-based four City comparison. Urban forestry & urban greening, 47, 126523. doi:10.1016/j.ufug.2019.126523.

