Abstract
Lingual thyroid occurs when the thyroid fails to descend embryologically. Case presentation of a 20-year old morbidly obese female with obstructive sleep apnea (OSA) and hypothyroidism diagnosed with a lingual thyroid measuring 4 × 4.5 × 3.4 cm, treated with long-term flap tracheotomy and transoral laser microsurgical excision. Lingual thyroids have the potential to result in acute airway compromise. Lingual thyroids can appear asymptomatic due to gradual airway adaptation but show airway narrowing on imaging studies. This patient’s OSA and hypothyroidism symptoms improved significantly post removal of lingual thyroid. Spontaneous hypothyroidism and OSA should be investigated and managed for optimal outcomes.
Background
The thyroid gland, an endocrine organ primarily responsible for the regulation of metabolism, develops on the 24th day of gestation originating from the primitive pharynx and neural crest, between the first and second pharyngeal pouches.[Citation1] During development, the thyroid migrates caudally from the foramen cecum to its anatomical location anterior to the larynx and upper trachea.[Citation2] Incomplete descent during development has an incidence of one in 200,000 normal subjects and causes pathology through ectopic thyroid tissue located anywhere along the thyroglossal duct.[Citation3]
A lingual thyroid occurs when the entire gland fails to descend from the base of the tongue. Ninety percent of ectopic thyroid development results in a lingual thyroid whereas the remaining 10% of cases are positioned along the thyroglossal duct. Lingual thyroid affects females more often than males at a ratio of 4:1.[Citation4] The presenting symptoms depend on the size of the ectopic thyroid which ranges from a few millimeters to 3–4 cm2. Lingual thyroid can be found incidentally in an asymptomatic patient or present with dysphagia, dysphonia, upper airway obstruction, hemorrhage, or hypothyroidism.[Citation5] Asymptomatic patients do not require therapy, surgical intervention is rarely indicated for lingual thyroid; however, treatment is indicated when severe obstructive symptoms are present.[Citation6] If the patient is euthyroid, it is important to determine the presence of properly located and functional thyroid tissue through a radioactive iodine uptake test. In order to treat a lingual thyroid, surgical excision is typically performed by the trans-oral route due to limited exposure.[Citation6]
Case report
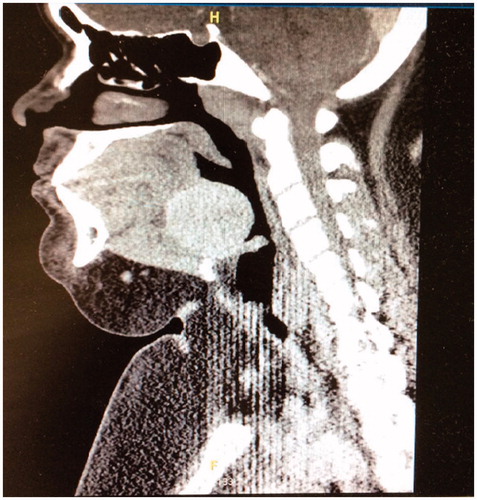
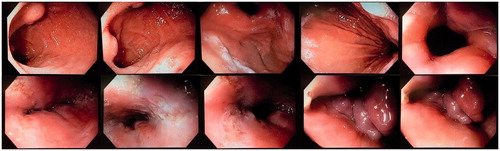
A 20 year old female with a BMI of 48 kg/m2, obstructive sleep apnea (OSA) intolerant to CPAP with RDI of 120 and oxyhemoglobin desaturation to 61%, diabetes mellitus, and uninvestigated hypothyroidism since an early age presented to the emergency department for hematemesis and sharp neck pain associated with difficulty swallowing. Esophagogastroduodenoscopy grossly revealed multiple ulcerations in the lower esophagus, biopsy positive for benign ulcerated squamous mucosa with acute inflammation and herpes virus, negative for intestinal metaplasia (). CT of the neck revealed a posterior tongue base mass at the level of the lingual tonsils, above the hyoid bone with no bony invasion, measuring 4 cm AP by 4.5 cm transverse by 3.4 cm CC without tissue anterior to the larynx (). Based on the endoscopy findings, CT scan, as well as a lack of risk factors for head and neck malignancy, the clinical diagnosis was ectopic lingual thyroid. The patient’s acute episode of hematemesis with anemia was diagnosed as HSV esophagitis treated with acyclovir. The HSV esophagitis irritated the mass resulting in the sharp neck pain.
Figure 1. Esophagogastroduodenoscopy with of abnormal-appearing ulcerations in the lower esophagus and a lobulated, edematous abnormal-appearing epiglottis.
The patient followed up at clinic two weeks later for evaluation of the tongue base mass. The patient was unaware of the mass prior to the emergency room visit. She denied dysphagia, dyspnoea, and difficulty opening her mouth or moving her neck. Physical examination revealed a morbidly obese woman in no apparent distress with a hyperactive gag reflex preventing indirect laryngoscopy. Flexible fiber optic examination provided visualization of a 5 cm tongue base mass that protruded into the airway. The remainder of examination was unremarkable. Due to the oropharyngeal airway narrowing and for definitive diagnosis, excision of the tongue base mass was undertaken by transoral laser microsurgery. Due to the severe OSA, airway management was managed by long-term flap tracheotomy. Plans for decannulation would be made pending post-operative sleep study and adequate use of CPAP.
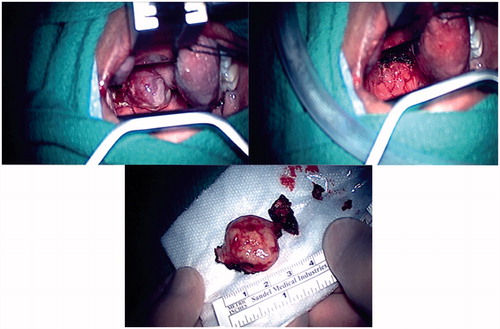
Intraoperatively, the mass was noted protruding from the tongue base, left of the midline (). The CO2 laser fiber was used to excise the visible mass and some of the sub mucosal mass from the tongue to the base of the epiglottis. The lingual surface of the epiglottis showed markedly redundant mucosa. The tissue appeared glandular with an infiltrative growth pattern and no discrete capsule. Through immunostaining for thyroglobulin, pathology confirmed thyroid tissue. Due to clinical and anatomical correlation, the ectopic thyroid tissue at the tongue base with mucosal ulceration was consistent with the diagnosis of lingual thyroid.
Figure 3. Operative images of the lingual thyroid sitting on the posterior tongue base viewed through the oropharynx and the excised lingual thyroid.
The patient was observed with an unremarkable course in the hospital for 6 d. The patient was presented at Tumor Board for further management that concluded that the ectopic lingual thyroid was adequately excised and required no further treatment. At post-operative evaluations, patient was stable with suspected tracheotomy site infection due to low-grade fevers and draining green mucus from tracheotomy site. Azithromycin was prescribed which eradicated her symptoms. At subsequent post-operative evaluations, the patient was stable on insulin therapy and 200 mcg of levothyroxine, eating well, and losing weight. Decannulation of Shiley tracheotomy tube was performed at the six-week post-operative visit, after confirming tolerance of CPAP with tracheotomy tube capped on post-operative polysomnogram.
Discussion
Lingual thyroid is a rare embryological malformation in which the thyroid gland fails to descend to its proper pre-laryngeal location. Arrest of the thyroid tissue migration has a wide spectrum of presentations ranging from asymptomatic with sufficient functional thyroid tissue to severe hypothyroidism with airway obstruction.[Citation7]
Our patient was diagnosed with hypothyroidism since five years of age, which can now be attributed to her non-functional lingual thyroid and complete absence of thyroid. Due to her thyroid disease, she developed severe obesity and OSA and thus insulin resistant diabetes. The lingual thyroid caused mild to moderate narrowing of the oropharyngeal airway. The patient had not noticed dysphagia or dysphonia due to the slow growing nature of the disease.
The tongue base mass was removed through a transoral microsurgical approach and confirmed by pathology to be ectopic thyroid tissue through immunostaining. At six weeks post-operative, the patient noted improvement in breathing and swallowing. Post-operative polysomnogram data showing tolerance to CPAP allowed decannulation in the office. She has remained stable on levothyroxine and insulin, resulting in a 10-pound weight loss since surgery. The patient’s sleeping notably improved on CPAP when she was seen at her one-month post-operative appointment ().
Table 1. Polysomnogram results performed pre-operatively and 1 month post-operatively with CPAP.
Conclusion
Lingual thyroid is a congenital condition which has a wide spectrum of presentations and thyroid states. Patients who present asymptomatically and are discovered incidentally have the potential to result in acute emergencies due to airway compromise.[Citation2] This potential increases with the size of the ectopic thyroid. Lingual thyroid has been associated with 1 in 4000–8000 patients with severe hypothyroidism.[Citation8] Once properly identified, the lingual thyroid may be excised with modern minimally invasive technique for definitive diagnosis and airway management. The co-morbidity of severe OSA, in this patient, was successfully managed post-operatively.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Henry JF. Applied embryology of the thyroid and parathyroid glands. In: Randolph GW, editor. Surgery of the thyroid and parathyroid glands. Philadelphia: Saunders; 2003. p. 12–20.
- Henry L. Surgical pathology of the head and neck. In: Barnes L, editor. The Journal of Pathology. New York and Basel: Marcel Dekker Inc; 1986. p. 157–158.
- Di Benedetoo V. Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: a case report. J Pediatr Surg. 1997;32:1745–1746.
- Baughman RA. Lingual thyroid and lingual thyroglossal tract remnants. a clinical and histopathologic study with review of the literature. Oral Surg Oral Med Oral Pathol. 1972;34:781–799.
- Toso A, Colombani F, Averono G, et al. Lingual thyroid causing dysphagia and dyspnea: case reports and review of the literature. Acta Otorhinolaryngol Ital. 2009;29:213–217.
- Ibrahim N. Ectopic Thyroid: etiology, pathology and management. Hormones. 2011;10:261–269.
- Baek MK, Kim EY, Lee SG, et al. A rare case of bleeding ectopic lingual thyroid presenting as hematemesis. Yonsei Med J. 2015;56:1163–1164.
- Khamassi K. Case report ectopic lingual thyroid. Case Rep Pediatr. 2015:1–4.