Abstract
Syphilis is a systemic infection caused by Treponema pallidum, and acquired syphilis is a well-known sexually transmitted infection with a variety of symptoms that hinder accurate diagnosis. We herein reported the case of a 60-year-old male with right unilateral syphilitic tonsillitis presenting as an ulcerated lesion accompanied with bilateral lymphadenopathy; metastatic oropharyngeal cancer was initially considered. Blood tests before surgery indicated syphilitic infection; however, because of the atypical lesion presentation in the absence of accompanying genital, skin, or systemic symptoms, tonsillectomy was performed to exclude malignancy. Syphilis is not commonly encountered in otorhinolaryngology; thus syphilis should be included in differential diagnosis for oral lesions of unknown origin. Critically, diagnostic surgery in addition to systemic physical examination is necessary to avoid misdiagnosis; failure of antibiotic therapy for syphilis without confirmed pathological diagnosis in true cases of oropharyngeal cancer may consequently lead to a delay in appropriate treatment and progression of malignancy.
Keywords:
A. Background
Syphilis is an infectious disease caused by Treponema pallidum and is classified as acquired or congenital; the acquired form is sexually transmitted. Syphilis is divided into four stages from the time of the appearance of chancre, a painless and indurated ulcer which develops 10–90 days after transmission: primary, secondary, tertiary, and quaternary.[Citation1] Primary syphilis is characterized by chancre with regional lymphadenopathy, whereas secondary syphilis, which occurs within one year after infection, is defined by the presence of local manifestations such as skin rash and/or mucocutaneous lesions. Secondary syphilis can also present with various systemic symptoms, including fever, headache, lymphadenopathy, hepatitis, splenomegaly, periostitis, arthritis, and glomerulonephritis.[Citation1–3]
Oral sex is an important route of transmission for T. pallidum, and local pathology is commonly observed in oral syphilis.[Citation2] Syphilitic lesions in the oral cavity can appear during any stage of syphilis; however, the main lesion location in syphilis is genitalia.[Citation4] In the oral cavity, primary chancres appear on the lip, tongue, and tonsils.[Citation3] Tonsillar lesions in syphilis are observed as non-tender, painless, and unilateral ulcerations[Citation4,Citation5]. Conversely, secondary syphilis of the oral cavity is characterized by mucous patches and/or painful ulcers with leukoplakia-like lesions.[Citation5–8]
Peripheral blood tests are crucial for the accurate diagnosis of syphilis and include nontreponemal tests (nTTs) and treponemal tests (TTs). nTTs including the Rapid Plasma Reagin (RPR) test can detect a number of heterophil IgG and IgM antibodies and have a relatively high sensitivity. RPR titers become positive around six weeks after infection and are used to monitor disease activity and treatment efficacy as they correlate with disease progression.[Citation1] TTs including the T. Pallidum hemagglutination (TPHA) test utilize recombinant treponemal antigens to detect both IgG- and IgM-type antibodies. TPHA becomes positive around three months after infection; however, titers are not helpful in syphilis diagnosis and should not be used to assess disease activity and treatment outcomes as they remain positive for life in most patients.[Citation1] Following successful treatment of syphilis, RPR titers do not become negative for 1–2 years, and the TPHA test remains positive. Thus, these tests will often be positive in individuals with risky behaviors who are repeatedly exposed to T. Pallidum, impeding proper association of symptoms with acute syphilis during clinical examination.[Citation5,Citation9]
Syphilitic tonsillitis is often confused with oropharyngeal cancer because of the painless and ulcerated lesions that can be observed in clinical presentation. Malignancy can be excluded only by pathological diagnosis, and although additional physical examinations and blood markers may aid in diagnosis, they usually do not provide definitive diagnosis.[Citation10] In this report, we present a patient with oral syphilis who presented with atypical signs and symptoms suggestive of oropharyngeal cancer.
B. Case report
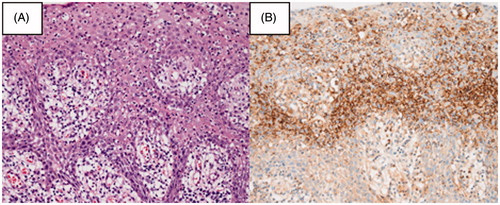
A 60-year-old homosexual male infected with human immunodeficiency virus (HIV) who was followed at the department of infectious diseases was noted to have an ulcerated right tonsillar tumor (Figure ) and bilateral lymphadenopathy by the infectious diseases specialist during a routine follow-up examination, and he was referred to the department of otorhinolaryngology in Osaka National Hospital. The patient had a smoking habit (20/day for 20 years; Brinkman’s index, 400). His HIV RNA levels by polymerase chain reaction (PCR) and CD4+ T cell counts measured in peripheral blood over the last four years were within normal ranges. The patient had no subjective symptoms such as pain or obstruction. On initial examination, the tonsillar tumor was elastic and hard by palpation. Bilateral submandibular lymph nodes were enlarged. Further evaluation by echography suggested a diagnosis of metastatic tumor due to the spherical form and the disappearance of hila of the lymph nodes (Figure ). The evaluation of specimens obtained by partial biopsy of the tonsillar lesion, performed three times, and fine-needle biopsy (FNA) of bilateral lymph nodes, performed five times in the consultation room, showed only nonspecific inflammatory changes. In addition, imaging studies including contrast-enhanced computed tomography (CECT) and 18F-fluorodeoxyglucose-positron emission tomography (18F-FDG PET) (Figure ) were performed. Specifically, CECT scans showed enhancement and enlargement of bilateral submandibular lymph nodes and absence of enhancement in bilateral tonsils. 18F-FDG PET scans showed that the accumulation of 18F-FDG in bilateral tonsils was within physiological limits (maximum standardized uptake value [SUVmax], 5.1 and 5.1 in right and left sides, respectively), whereas 18F-FGD accumulation in bilateral submandibular lymph nodes was significant (SUVmax, 4.7 and 4.3 in right and left sides, respectively). However, preoperative blood tests as part of routine preoperative assessment indicated syphilis infection (RPR, 108 RPR unit [RU], TPHA, positive). A prior test four years earlier was negative for exposure to T. pallidum at the time, suggesting that the patient was acutely infected. Nonetheless, surgery was performed to exclude malignancy. The final pathological diagnosis was syphilitic tonsillitis (Figure ). Based on the consultation with the infectious diseases specialists, the patient was successfully treated with constant infusion of 24,000,000 units of benzylpenicillin for seven days; the tonsillar lesion and lymphadenopathy disappeared in two months.
Figure 2. Echography of bilateral submandibular lymph nodes. Note their spherical form and the absence of hila.
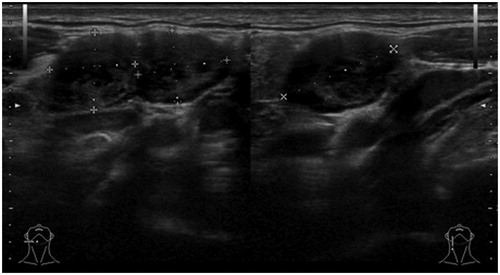
Figure 3. Scans from contrast enhanced computed tomography (CECT) and 18F-fluorodeoxyglucose-positron emission tomography (18F-FDG PET) imaging studies. (A) A CECT scan showing bilateral swelling of lymph nodes and normal tonsils that are not enhanced. (B) An 18F-FDG PET scan shows accumulation of 18F-FDG within the physiological range (maximum standardized uptake value [SUVmax], 5.1 and 5.1 in right and left sides, respectively) in bilateral tonsils, whereas 18F-FDG accumulation is observed at significant levels in bilateral submandibular lymph nodes (SUVmax, 4.7 and 4.3 in right and left sides, respectively).
![Figure 3. Scans from contrast enhanced computed tomography (CECT) and 18F-fluorodeoxyglucose-positron emission tomography (18F-FDG PET) imaging studies. (A) A CECT scan showing bilateral swelling of lymph nodes and normal tonsils that are not enhanced. (B) An 18F-FDG PET scan shows accumulation of 18F-FDG within the physiological range (maximum standardized uptake value [SUVmax], 5.1 and 5.1 in right and left sides, respectively) in bilateral tonsils, whereas 18F-FDG accumulation is observed at significant levels in bilateral submandibular lymph nodes (SUVmax, 4.7 and 4.3 in right and left sides, respectively).](/cms/asset/3fdda93c-46f6-4218-a26c-cb8dc78af6e3/icro_a_1256214_f0003_c.jpg)
C. Discussion
Oral syphilis can present with several phenotypes and may be confused with malignant tumors during otolaryngologic examination. The oral lesion in the present case was strongly suspected as oropharyngeal cancer. To date, several syphilis cases involving the oral cavity were reported,[Citation2,Citation4–11] and the majority of these cases were diagnosed as secondary syphilis. Intriguingly, reports of primary syphilis presenting as painless oral chancres on the lips, tongue, and tonsils are increasingly reported. Accompanied with regional lymphadenopathy,[Citation2,Citation3,Citation9] this presentation commonly leads to the suspicion of malignancy. In the present report, the patient did not have any symptoms other than the ulcerated tonsillar tumor. Similar to earlier reports, the patient was correctly diagnosed with primary syphilis.
Although blood tests, including RPR and TPHA, are very useful for syphilis diagnosis, their positivity may not be sufficient to exclude malignancy. In addition, antibody titers are not elevated immediately after infection and do not decrease following infection resolution, hindering accurate evaluation of existing symptoms for the diagnosis of acute as well as chronic syphilis infections. Additionally, patients with HIV infection exhibit behavioral patterns such as oral sex that increase the risk of other sexually transmitted diseases (STDs); therefore, suspicion for coexisting STDs, including syphilis, should be higher for patients such as the HIV-infected patient presented in this report. Furthermore, positivity for syphilis by blood tests might indicate past or chronic infection in these patients, further complicating differential diagnosis.
Unlike that observed in the present case, numerous symptoms such as fever, dysphagia or dysphonia,[Citation6,Citation11] skin lesions,[Citation5,Citation7] and sore throat [Citation5,Citation6,Citation11] were reported in previous oral syphilis cases. Furthermore, in the majority of the patients, tonsillar lesions were bilateral.[Citation5,Citation6,Citation11] In our patient, oropharyngeal cancer was suspected because of the painless presentation of a unilateral tonsillar lesion with no other symptoms; moreover, gross appearance resembled a malignant tumor, and pathological examinations, including biopsy and FNA, were performed in the consultation room. In previous cases, partial biopsies of tonsils showed only inflammatory changes,[Citation5,Citation6,Citation11] similar to the present case. Biopsy for oropharyngeal cancer may be inconclusive because the outer regions of the tumor mass may exhibit only inflammatory changes, and malignancy may only be observed in specimens obtained from deeper sites [Citation10] or in a quite limited part of the tonsil.[Citation12] In our patient, these caveats impeded the absolute exclusion of malignancy based on the results of partial biopsy samples and led to the decision of surgery.
Definite pathological diagnosis requires further biopsy and surgical resection of the tonsil; thus, tonsillectomy was chosen in this patient. As a result, histopathological examination demonstrated syphilitic tonsillitis and no malignancy. Hamlyn et al. [Citation11] reported surgical dissection of the tonsil in patients with unilateral tonsillar lesions presenting with sore throat. For the conclusive exclusion of malignancy as a diagnosis, surgery was performed in the present case.
D. Conclusions
In this report, we presented a patient with a unilateral ulcerated tonsillar tumor and bilateral lymphadenopathy due to syphilis, which resembled a metastatic tumor. Blood tests led to the diagnosis of syphilis; however, pathological diagnosis that was necessary to exclude malignancy required surgical removal of the tonsil. Not only malignancy but also syphilis should be considered in the differential diagnosis of patients presenting with unilateral ulcerated tonsillar lesions accompanied with lymphadenopathy.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Janier M, Heqvi V, Dupin N, et al. European guideline on the management of syphilis: giving evidence priority. J Eur Acad Dermatol Venereol. 2014;28:1581–1593.
- Fiumara NJ, Walker EA. Primary syphilis of the tonsil. Arch Otolaryngol. 1982;108:43–44.
- McNulty JS, Fassett RL. Syphilis: an otolaryngologic perspective. Laryngoscope. 1981;91:889–905.
- Viers WA. Primary syphilis of the tonsil: presentation of four cases. Laryngoscope. 1981;91:1507–1511.
- Baarsma EA, Kazzaz B, Soei KI. Secondary syphilis of the tonsils. J Laryngol Otol. 1985;99:601–603.
- Mannarà GM, Sacilotto C, Frattasio A, et al. Bilateral secondary syphilis of the tonsil. J Laryngol Otol. 1999;113:1125–1127.
- Shimizu T, Shinogi J, Majima Y, et al. Secondary syphilis of the tonsil. Arch Otorhinolaryngol. 1989;246:117–120.
- de Paulo LF, Servato JP, Oliveira MT, et al. Oral manifestations of secondary syphilis. Int J Infect Dis. 2015;35:40–42.
- Ishimaru T, Mizuno Y, Shiga H, et al. Patient with primary tonsillar and gastric syphilis. J Laryngol Otol. 1997;111:766–768.
- Oddó D, Carrasco G, Capdeville F, et al. Syphilitic tonsillitis presenting as an ulcerated tonsillar tumor with ipsilateral lymphadenopathy. Ann Diagn Pathol. 2007;11:353–357.
- Hamlyn E, Marriott D, Gallagher RM. Secondary syphilis presenting as tonsillitis in three patients. J Laryngol Otol. 2006;120:602–604.
- Yasui T, Morii E, Yamamoto Y, et al. Human papillomavirus and cystic node metastasis in oropharyngeal cancer and cancer of unknown primary origin. PLoS One. 2014;9:e95364. doi: 10.1371/journal.pone.0095364.