Abstract
Thyroglossal duct remnants can harbour malignant changes in them and can present as thyroglossal cysts which are picked up incidentally in postoperative histopathology. Management of these thyroglossal duct carcinomas has always been a controversy to decide on the need to perform a total thyroidectomy in these patients and the adjuvant treatment that’s required. We present a case of a 48-year-old female patient of thyroglossal duct cyst carcinoma who had to be taken for total thyroidectomy and radio iodine ablation during treatment of the lesion. Careful treatment planning aids are necessary in the management of such lesions.
Introduction
Thyroglossal duct cysts present as anterior midline painless neck masses in close relation to hyoid bone. Thyroglossal cysts are common in paediatric age group but can also be seen in older age groups. They are benign most of the times and occurrence of malignancy in the cyst has been rarely reported, though rare. The first case of thyroglossal duct cyst carcinoma was described by Brentano in 1911 [Citation1]. Hirshoren et al. [Citation2] in their review of 160 cases of thyroglossal duct cysts, reported papillary carcinoma in only one patient. Total number of reported cases in world literature till date is 275 [Citation3]. Although papillary thyroid carcinoma is the most common type, squamous carcinomas can also occur [Citation4]. Differentiated thyroid carcinomas (DTC) in thyroglossal cyst are more aggressive compared to those arising within the thyroid tissue and many a times associated with concomitant tumours in the thyroid gland and lymph nodes at presentation. Aggressive surgical approach is needed while dealing with DTC in thyroglossal duct cyst. However, controversies exist regarding the management of such cases. Sistrunk’s operation is done in all cases, but the role of total thyroidectomy and radioiodine therapy is controversial and no uniform consensus exists.
Here, we present a rare case of a 48-year-old woman who presented with a thyroglossal duct cyst in the sub-mental region, which was later diagnosed as papillary thyroid carcinoma of the thyroglossal cyst in postoperative histopathology. We have tried to discuss the management issues involved and review the literature.
Case report
A woman of 48 years in age presented to our outpatient department with a swelling in the upper neck. The lesion was insidious to begin with and gradually progressing since one and a half years. She did not complaint of pain, dysphasia, dyspnoea and change in voice. She had hypothyroid hormonal status and was on medication. History of prior irradiation was absent.
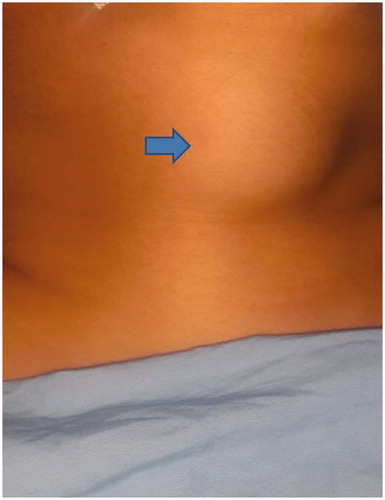
On examination, there was a 4 × 3 cm firm, diffuse, non-tender swelling in the sub-mental region superiorly reaching 1 cm below the mandible to 1 cm above thyroid notch inferiorly. Overlying skin was pinchable. Swelling was moving with deglutition but not with protrusion of the tongue. (Figure ) There were no palpable lymph nodes and a soft non-tender bulge present in the floor of mouth. Thyroid gland was normal on palpation. Systemic examinations were normal. On investigation, the patient was euthyroid. Fine needle aspiration cytology (FNAC) revealed a benign cystic lesion. An ultrasound of the neck and thyroid gland was done. Ultrasonography (USG) of neck showed normal thyroid gland with no evidence of hypo echoic nodules. There was no evidence of lymphadenopathy in the neck. A clinical diagnosis of supra hyoid thyroglossal cyst was made.
Figure 1. Preoperative showing the presence of cystic lesion above the hyoid bone (supra hyoid thyroglossal cyst).
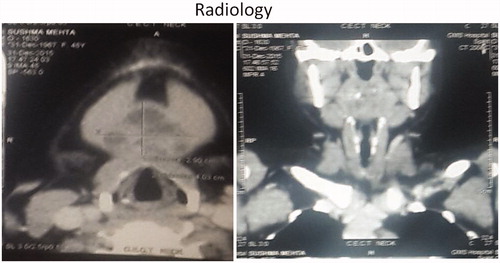
Contrast-enhanced computed tomography scan revealed a midline complex cystic lesion of 4 × 3 cm in the region of hyoid with tiny specks of calcification. Significant enhancement was seen in the nodular component situated posteriorly abutting the hyoid bone. Lesion was abutting the medial border of bilateral mylohyoid and abutted the hyoid bone and strap muscles in the inferior extend. (Figure )
Figure 2. CT scan of Neck axial cuts showing well encapsulated cystic lesion with areas of heterogeneity within the cyst.
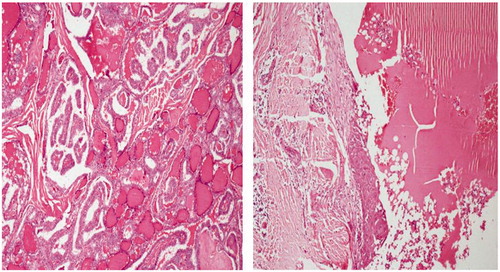
She underwent Sistrunk’s procedure. Intra-operative findings revealed a 3 × 3 cm cystic swelling in the sub-mental region which was going into the body of the hyoid bone. The muscles of floor of mouth were adherent to swelling. Tract was delineated till base of tongue and excised totally along with the body of hyoid. Post-operative histopathological examination showed large cyst of 3.5 × 3×2.5 cm with solid areas. The solid areas showed tumour with predominant papillary pattern with mild pleomorphism and vesicular nuclei and infiltration into the muscles of neck. Cystic areas showed large dilated thyroid follicles lined by cuboidal epithelium. A diagnosis of Papillary in carcinoma thyroid in thyroglossal cyst was made. (Figure )
The decision of whether to proceed with a total thyroidectomy in view of the normal thyroid USG and the absence of lymph nodes in the neck was a management issue for us. We had to discuss the issue of total thyroidectomy, as on one end it would lead to lifelong external thyroid hormone dependency along with the chances of developing hypoparathyroidism; and on the other hand there was need of total thyroidectomy in order to make her physiologically eligible for the radioiodine scans for diagnosis and if required for radio ablation in view of the infiltrated strap muscles in the histology. The normal thyroid USG added to the dilemma. However, she was planned for total thyroidectomy considering the status of cyst which was adherent to the muscles of the floor of the mouth and also showed infiltration in histopathology after and informed discussion with the patient and a multidisciplinary review in the tumour board of the institute. The earlier evidences in literature by Balalaa et al. [Citation3] and Pellegriti et al. [Citation5] were considered while discussing the option of thyroidectomy with the patient along with the need of post-operative whole body radio Iodine Diagnostic scans. Total thyroidectomy was performed. Histopathological examination of total thyroid specimen showed no definite nodule or focal lesion and no residual tumour in thyroid gland could be revealed.
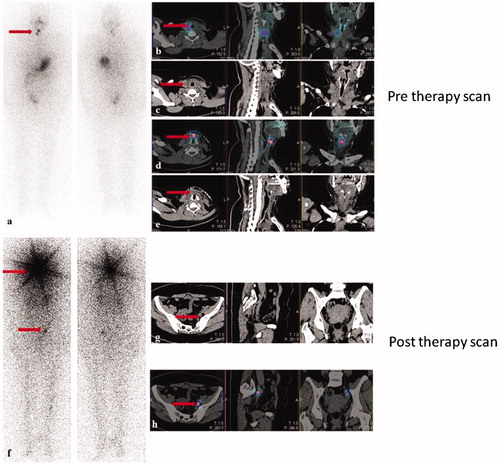
Diagnostic whole body radio iodine scan with single-photon emission computerised tomography (SPECT CT) of neck was done, which showed tracer uptake in thyroid bed and a strap muscle in the in the region of thyroglossal cyst. Radioactive ablation was done with 110 micro curie of I 131. Post-therapy whole body radio iodine scan with SPECT CT showed tracer uptake in right ovary. (Figure ) Carcino-embryonic antigen 125 was done, which was within normal limits. Ovary uptake was thought to be physiological uptake and she is being kept under regular follow up in gynaecology and ENT for last 6 months.
Discussion
Thyroid gland descends from foramen caecum in the tongue to its location in the neck after arising as a midline endodermal invagination of the foregut. The tract closes around 5th to10th week of gestational life and failure of involution gives rise to thyroglossal remnants. Thyroglossal remnants can present as a cyst, duct, tract, fistula or ectopic thyroid tissue [Citation3]. Thyroglossal cysts constitute the commonest congenital disorders of thyroid gland. 70% of neck masses diagnosed in childhood are thyroglossal cysts whereas in adults, they contribute only 7% [Citation2]. They can be found anywhere between sub-mental and suprasternal region [Citation3].
Malignancy in a thyroglossal duct cyst is rare entity and accounts for 1% of all thyroglossal cysts (1%).[Citation6,Citation7] 90–95% of these carcinomas arise from thyro-embryonic remnants within the cysts [Citation8]. Commonest among these are papillary carcinomas [Citation9], although follicular [Citation10] and mixed types can also occur [Citation11]. Squamous cell carcinoma arising within thyroglossal duct cyst is even rarer and contributes less than 5% of all malignant lesions involving thyroglossal cysts [Citation12]. Widstrom et al. [Citation13] laid down the criteria for diagnosing primary carcinoma of thyroglossal duct remnants, which includes histological identification of thyroglossal duct carcinoma (TGDC) by demonstration of carcinomatous areas in epithelial lining of ducts along with normal thyroid follicles within the walls of the cysts, normal thyroid tissue adjacent to the tumour and histopathological evidence of the thyroid gland showing no signs of primary carcinoma arising from the thyroid gland [Citation14].
Among the various theories those have been formulated regarding the origin of a thyroglossal cyst carcinoma, the most plausible one states that carcinomas in the thyroglossal duct/cyst arise de novo in the thyroid remnants present in the thyroglossal cyst [Citation15]. This explains the reason for which of medullary carcinoma (MTC) thyroid has never been reported in thyroglossal tract remnants as MTC arises from para-follicular cells. Other possible explanations proposed regarding the origin of papillary carcinomatous lesions in thyroglossal remnants include multi focal origin of carcinomas in genetically predisposed individuals and metastasis from papillary carcinomas of thyroid gland [Citation16]. Columnar lining of the thyroglossal cyst can undergo metaplasia and lead to squamous cell carcinoma on rare instances [Citation4] even in the absence of thyroid tissue in the ductal epithelial lining and surrounding soft tissue of the thyroglossal cyst. Therefore, some researchers believe that squamous cell carcinoma is the only true carcinoma of the thyroglossal cyst [Citation17,Citation18]. It is a rare entity and does have a mortality rate of 30–40 [Citation19].
Thyroglossal duct cyst carcinoma usually present with clinical features similar to benign thyroglossal duct cyst and it is often difficult to clinically diagnose it preoperatively. Thyroglossal cyst carcinoma is more common in females from third to sixth decade as seen in our case. Thyroglossal duct cyst should be evaluated preoperatively with Ultra sonography, CT scan, Magnetic resonance imaging and FNAC in all cases. Even after these investigations a diagnosis of thyroglossal duct cyst carcinoma is usually made postoperatively after histopathological examination .This is due to inadequate sampling done with aspiration cytology studies without USG guidance. FNAC has sensitivity of 50–60% in diagnosing carcinomas of thyroglossal duct cyst as compared to primary thyroid gland lesions where the sensitivity is 85%.
On ultrasound examination of neck, the cyst presents as an anechoic to hypo-echoic lesion with the presence of solid areas along the cyst wall or within the cyst and may have micro calcifications. Thyroid gland sonography should always be done to rule out multifocal cancer. Ultrasound, CT and MRI imaging studies can be used to evaluate the neck for nodal metastases as per need and surgical planning. Radionuclide studies may be used to see whether normally functioning thyroid gland is present in neck and whether there are any cold areas in the thyroid tissue of the cyst and the thyroid gland. FNAC of any suspicious nodule in the thyroid gland should be done.
Controversy exists regarding management of such cancers. The role of total thyroidectomy remains debatable especially if there is no suspicious nodule is detected on ultra sonography as it was seen in our case. Literature is divided on this issue, however, broad guidelines indicate that total thyroidectomy should be done based on risk stratification. High-risk factors include age >45 years, male, size >4 cm, extra-capsular invasion, positive nodal status, history of irradiation, presence of cold nodules in thyroid on thyroid scan [Citation8,Citation20,Citation21]. In such high-risk cases, Sistrunk’s surgery with total thyroidectomy and modified neck dissection should be done if neck nodes are present. In such cases post-operative radio-iodine ablation with thyroid suppression should be considered. Pellegriti et al. [Citation5] reported a rate of 60% incidence of occurrence of pT1 micro carcinomas among elective total thyroidectomies performed in cases of thyroglossal duct cyst carcinoma. Similarly Bakkar [Citation22] has found a 43% risk of missing a malignancy in sonographically normal thyroids after Sistrunk’s surgery in cases of papillary carcinomas in thyroglossal duct cysts. Miccoli et al. [Citation23,Citation24] in their two retrospective studies propose that ‘total thyroidectomy for tumours of thyroglossal cysts could be justified by the high incidence of associated papillary carcinomas of the thyroid and by the relatively aggressive nature that some tumours’. On the contrast, Hartl [Citation25] could find carcinomatous foci in the thyroid lobes in 3 out of 18 cases. Dzodic et al. [Citation26] reported a 25% rate of detecting a lesion in the thyroidectomy specimen. In low-risk cases age <45 years, cyst size less than 4 cm, no extra capsular infiltration and no neck node Sistrunk’s operation only will suffice but requires regular and close follow up. Sistrunk’s operation involves removal of the cyst, body of hyoid along with the tract until foramen caecum. Patel et al. found that the 5-year survival rate is 100% and concluded that the addition of total thyroidectomy to Sistrunk’s operation didn’t change the outcome [Citation27].
The present case fell into high-risk category due to age >45 years and cyst more than 4 cm with muscle infiltration. Hence, total thyroidectomy was done after discussing the options with the patient. Postoperatively radioiodine ablation was also done and patient was kept on thyroid suppression therapy.
In a case of squamous cell carcinoma, wide local resection is recommended and neck dissection should be done in cases of nodal metastasis. Adjuvant radiotherapy is recommended in case of positive surgical margins, extensive nodal metastasis and larger tumour size [Citation4].
Conclusions
The rarity of papillary carcinoma in a thyroglossal remnant leads to controversies in the management of such patients. In low-risk patients, a Sistrunk’s operation will suffice. In high-risk patients, a combined modality approach should be done.
Disclosure statement
There is no conflict of interest or financial disclosure to be made.
References
- Brentano H. Struma aberrata lingual mit druzen metastasen. Dtsch Med Wochenschr. 1911;37:665.
- Hirshoren N, Neuman T, Udassin R, et al. The imperative of the Sistrunk operation: review of 160 thyroglossal tract remnant operations. Otolaryngol Head Neck Surg. 2009;140:338–342.
- Balalaa N, Megahed M, Ashari MA, et al. Thyroglossal duct cyst papillary carcinoma. Case Rep Oncol. 2011; 4:39–43.
- Shah S, Kadakia S, Khorsandi A, et al. Squamous cell carcinoma in a thyroglossal duct cyst: a case report with review of the literature. Am J Otolaryngol. 2015;36:460–462.
- Pellegriti G, Lumera G, Malandrino P, et al. Thyroid cancer in thyroglossal duct cysts requires a specific approach due to its unpredictable extension. J Clin Endocrinol Metab. 2013;98:458–465.
- Heshmati HM, Fatourechi V, van Heerden JA, et al. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc. 1997;72:315–319.
- Cheon NJ, Lee YM, Lee JH, et al. Papillary carcinoma within a thyroglossal duct cyst in a 17-year-old child. J Craniofac Surg. 2016;27:e282–e283.
- Forest VI, Murali R, Clark JR. Thyroglossal duct cyst carcinoma: case series. J Otolaryngol Head Neck Surg. 2011;40:151–156.
- Patel NS, Sheykholeslami K. Papillary carcinoma in thyroglossal duct cyst: two case reports and review of the literature. Ear Nose Throat J. 2016;95:E36–E38.
- Kim WJ, Souillard R, Brandwein MS, et al. Follicular adenoma in a juxtathyroidal thyroglossal duct cyst with papillary carcinoma in the adjacent thyroid gland. Am J Otolaryngol. 2005;26:348–350.
- Van Vuuren PA, Balm AJ, Gregor RT, et al. Carcinoma arising in thyroglossal remnants. Clin Otolaryngol Allied Sci. 1994;19:509–515.
- El Bakkouri W, Racy E, Vereecke A, et al. Squamous cell carcinoma in a thyroglossal duct cyst. Ann Otolaryngol Chir Cervicofac. 2004;121:303–305.
- Widstrom A, Magnusson P, Hallberg O, et al. Adenocarcinoma originating in the thyroglossal duct. Ann Otol Rhinol Laryngol. 1976;85:286–290.
- Carter Y, Yeutter N, Mazeh H. Thyroglossal duct remnant carcinoma: beyond the Sistrunk procedure. Surg Oncol. 2014;23:161–166.
- Hilger AW, Thompson SD, Smallman LA, et al. Papillary carcinoma arising in a thyroglossal duct cyst: a case report and literature review. J Laryngol Otol. 1995;109:1124–1127.
- Tew S, Reeve TS, Poole AG, et al. Papillary thyroid carcinoma arising in thyroglossal duct cysts: incidence and management. Aust N Z J Surg. 1995;65:717–718.
- Mobini J, Krouse TB, Klinghoffer JF. Squamous cell carcinoma arising in a thyroglossal duct cyst. Am Surg. 1974; 40:290–294.
- Iakovou I, Konstantinidis I, Doumas A, et al. Squamous cell carcinoma in a thyroglossal duct cyst and 99mTc-MIBI findings. Hell J Nucl Med. 2011;14:62–64.
- Boswell WC, Zoller M, Williams JS, et al. Thyroglossal duct carcinoma. Am Surg. 1994;60:650–655.
- Chrisoulidou A, Iliadou P, Doumala E, et al. Thyroglossal duct cyst carcinomas: is there a need for thyroidectomy? Hormones (Athens). 2013;12:522–528.
- Tharmabala M, Kanthan R. Incidental thyroid papillary carcinoma in a thyroglossal duct cyst – management dilemmas. Int J Surg Case Rep. 2013;4:58–61.
- Bakkar S, Biricotti M, Stefanini G, et al. The extent of surgery in thyroglossal cyst carcinoma. Langenbecks Arch Surg. 2016; 6 p. DOI:10.1007/s00423-016-1460-x.
- Miccoli P, Pacini F, Basolo S, et al. Thyroid carcinoma in a thyroglossal duct cyst: tumor resection alone or a total thyroidectomy? Ann Chir. 1998;52:452–454.
- Miccoli P, Minuto MN, Galleri D, et al. Extent of surgery in thyroglossal duct carcinoma: reflections on a series of eighteen cases. Thyroid. 2004;14:121–123.
- Hartl DM, Al Ghuzlan A, Chami L, et al. High rate of multifocality and occult lymph node metastases in papillary thyroid carcinoma arising in thyroglossal duct cysts. Ann Surg Oncol. 2009;16:2595–2601.
- Dzodic R, Markovic I, Stanojevic B, et al. Surgical management of primary thyroid carcinoma arising in thyroglossal duct cyst: an experience of a single institution in Serbia. Endocr J. 2012;59:517–522.
- Patel SG, Escrig M, Shaha AR, et al. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. J Surg Oncol. 2002;79:134–139.