Abstract
Endoscopic medial maxillectomy (EMM) was originally developed for surgery of maxillary sinus disease. This surgery was recently modified to preserve the inferior turbinate (IT) and the nasolacrimal duct (ND) and is commonly referred to endoscopic modified medial maxillectomy (EMMM). Here we present a case of endoscopic repair for a blowout fracture of the inferior orbital wall via access through the medial wall of the maxillary sinus, thereby preserving IT and ND, similar to EMMM. Two months postoperatively, a diplopia field test, computed tomography, and endoscopic observation were performed. Good recovery of diplopia was obtained, and empty nose syndrome, epiphora, and cheek numbness were not observed. Those complications such as empty nose syndrome, epiphora and cheek numbness can be avoided by the approach presented in this report; therefore, the maxillary medial wall approach, like EMMM, could become a preferred surgical method for blowout fractures of the inferior orbital wall.
Background
Transnasal endoscopic surgery, like endoscopic sinus surgery (ESS), has recently been developed, and its application has been expanded for various pathologies. Endoscopic medial maxillectomy (EMM), a type of ESS, was originally developed for surgery of the maxillary sinus (MS) and, in particular, inverted papilloma (IP) [Citation1–3]. During EMM, the inferior turbinate (IT) and nasolacrimal duct (ND) are commonly injured. IT has an important function in nasal airflow [Citation4,Citation5], and its resection may cause atrophic rhinitis, also called empty nose syndrome, which is difficult to treat [Citation6,Citation7], and an injury to ND often causes epiphora [Citation8]. However, the surgery was recently modified to preserve both IT and ND [Citation9–11], and is now referred to as endoscopic modified medial maxillectomy (EMMM) [Citation11].
Blowout fractures of the inferior orbital wall cause diplopia and/or ocular motility disorder. There are several accepted surgical procedures used to treat blowout fractures of the inferior orbital wall, such as the subciliary approach [Citation12], the transconjunctival approach [Citation13], and the canine fossa approach [Citation14,Citation15], and these are often used in combination. However, these procedures sometimes induce problematic complications.
EMMM was developed for surgery of MS disease; however, the maxillary medial wall approach is appropriate for blowout fractures and has lesser complications than conventional approaches. Furthermore, if the fracture involves the medial orbital wall, it can be repaired using the same surgical field.
In the present case, we conducted surgery through the medial wall of MS, similar to EMMM, for a blowout fracture of the inferior orbital wall and discussed its merits and indication.
Case report
History of the present illness
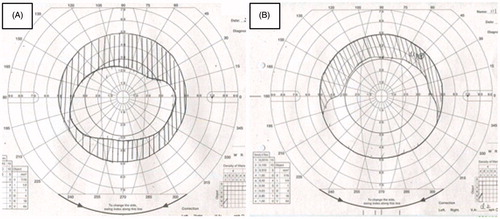
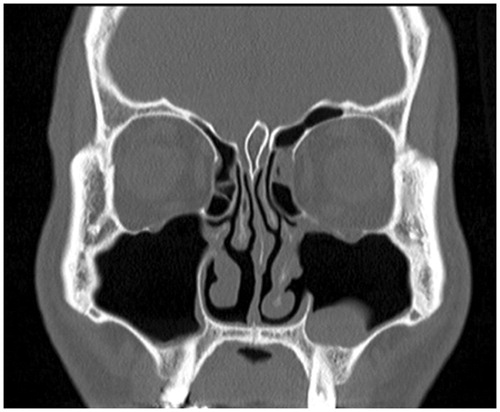
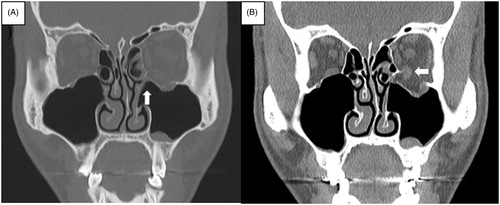
The patient was a 34-year-old male who was hit on the left eye and developed diplopia. Three days after the injury, he visited our institution, and we performed computed tomography (CT) and diagnosed him with a blowout fracture of the inferior orbital wall (Figure ). The bone window setting showed that the inferior orbital wall was fractured like a swinging door (Figure , white arrow), and the soft-tissue window setting showed dislocation of the inferior rectus muscle (Figure , white arrow). His diplopia field showed superior and inferior vertical diplopia of approximately 30° (Figure ). The diplopia did not naturally improve within 7 days after the injury, and we then performed the operation.
Figure 1. Bone window setting (A) and soft-tissue window setting (B) as seen in preoperative computed tomography image. The bone window setting showed that the inferior orbital wall was fractured like a swinging door (A, white arrow), and the soft-tissue window setting showed the dislocation of the inferior rectus muscle (B, white arrow).
Surgical procedure
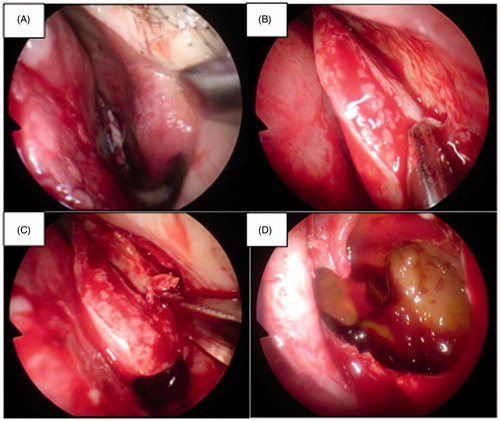
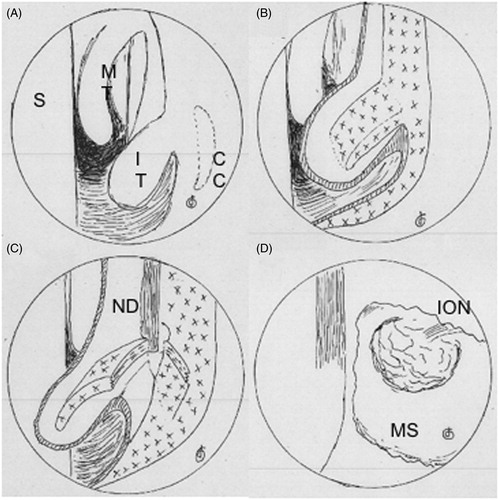
The operation was performed under general anesthesia. Figures show the endoscopic view before the incision. A mucosal incision from the medial wall of MS behind the concha crest toward the floor of the nose was made. The mucosal flap was elevated, and the IT bone was revealed (Figures and ). The IT bone and ND were medially swung from the medial wall of MS (Figures and ). The medial wall of MS was then removed, and the herniation of the orbital contents with the swing-door-like fractured bone was observed (Figures and ). Small segments which disturbed motility of the inferior rectus muscle were removed, the resistance of the inferior rectus muscle was released, the orbital contents were put into the orbit, and the bone plate of the inferior wall was used to support the orbital contents. Finally, a ureteral balloon catheter was put through the inferior nasal meatus to support the inferior orbital wall.
Figure 3. Schemas of endoscope during surgery. The preincisional view is shown in A. The bone of the inferior turbinate and the medial wall of the maxillary sinus were revealed (B). The bone of the inferior turbine and the nasolacrimal duct were revealed (C). The maxillary sinus and the orbital contents within it were observed (D). S: nasal septum; MT: middle turbinate; IT: inferior turbinate; CC: concha crest; ND: nasolacrimal duct; MS: maxillary sinus; ION: infraorbital nerve.
Postoperative course
The ureteral balloon was removed 10 days postoperatively. The subjective diplopia remained for several days postoperatively but disappeared a day after removing the balloon. The patient did not complain of epiphora or cheek numbness throughout the entire period. The postoperative diplopia field and CT scan were performed 2 months postoperatively. The CT scan showed that the fracture of the inferior orbital wall and the dislocation of the inferior rectus muscle were repaired (Figure ). The diplopia field had recovered to approximately 10° (Figure ).
Discussion and conclusions
Maxillary medial wall approach versus other conventional surgical approaches for blowout fracture repair
There are several acceptable surgical procedures for blowout fracture repair. The transcutaneous approaches, including the subciliary approach and the transconjunctival approach, are mostly preferred by plastic surgeons. These procedures require an external incision on the palpebral conjunctiva or the skin of the lower eyelid, and sometimes these procedures cause ectropion because of the injury of the supporting structures of the lower eyelid [Citation16,Citation17]. The canine fossa approach, which is a conventional technique, requires an oral mucosal incision and the elevation of the mucoperiosteal flap. Therefore, cheek numbness often occurs as an irreversible complication due to injury of the infraorbital nerve or its branch. In contrast to these procedures, the maxillary medial wall approach requires only a nasal mucosal incision; therefore, there is no risk of ectropion or check numbness.
Various methods are used for reconstruction; however, there is some controversy about their indication. Reconstruction with soft materials is often used in the canine fossa approach. The ureteral balloon is commonly used as a soft material [Citation14,Citation15]. However, a previous study reported that reconstruction with soft materials might cause enophthalmos [Citation18]. Reconstruction with hard materials requires a relatively wide operation field and are often applied via the subciliary or transconjunctival approach [Citation12,Citation13]. Nishiike et al. reported favorable results using antral bone via the canine fossa approach [Citation15]. In the present study, we used the ureteral balloon and inferior orbital bone as soft and hard materials, respectively, for reconstruction. The maxillary medial wall approach provided a surgical field wide enough to use hard materials, such as a cartilage from the nasal septum or a hydroxyapatite plate.
Indication of the medial wall approach for blowout fractures
As mentioned above, the maxillary medial wall approach generally has lesser complications than conventional approaches. Furthermore, it can be used to apply both soft and hard reconstruction materials because of its wide operation field. If a fracture involves the medial orbital wall and the inferior orbital wall, we can repair both walls using the same operating field. Therefore, the maxillary medial wall approach may be a treatment indication for blowout fractures of the inferior orbital wall.
Geolocation information
Osaka, Japan
Acknowledgements
None declared.
Disclosure statement
The authors report no conflicts of interest.
References
- Kamel RH. Transnasal endoscopic medial maxillectomy in inverted papilloma. Laryngoscope. 1995;105:847–853.
- Sadeghi N, Al-Dhahri S, Manoukian JJ. Transnasal endoscopic medial maxillectomy for inverting papilloma. Laryngoscope. 2003;113:749–753.
- Wormald PJ, Ooi E, van Hasselt CA, et al. Endoscopic removal of sinonasal inverted papilloma including endoscopic medial maxillectomy. Laryngoscope. 2003;113:867–873.
- Chen XB, Leong SC, Lee HP, et al. Aerodynamic effects of inferior turbinate surgery on nasal airflow: a computational fluid dynamics model. Rhinology. 2010;48:394–400.
- Chen XB, Lee HP, Chong VF, et al. Numerical simulation of the effects of inferior turbinate surgery on nasal airway heating capacity. Am J Rhinol Allergy. 2010;24:e118–e122.
- Hildenbrand T, Weber RK, Brehmer D. Rhinitis sicca, dry nose and atrophic rhinitis: a review of the literature. Eur Arch Otorhinolaryngol. 2011;268:17–26.
- Heathcote KJ, Nair SB. The impact of modern techniques on the recurrence rate of inverted papilloma treated by endonasal surgery. Rhinology. 2009;47:339–344.
- Sadeghi N, Joshi A. Management of the nasolacrimal system during transnasal endoscopic medial maxillectomy. Am J Rhinol allergy. 2012;26:e85–e88.
- Suzuki M, Nakamura Y, Nakayama M, et al. Modified transnasal endoscopic medial maxillectomy with medial shift of preserved inferior turbinate and nasolacrimal duct. Laryngoscope. 2011;121:2399–2401.
- Nakamaru Y, Furuta Y, Takagi D, et al. Preservation of the nasolacrimal duct during endoscopic medial maxillectomy for sinonasal inverted papilloma. Rhinology. 2010;48:452–456.
- Nakayama T, Asaka D, Okushi T, et al. Endoscopic medial maxillectomy with preservation of inferior turbinate and nasolacrimal duct. Am J Rhinol Allergy. 2012;26:405–408.
- Lee HH, Alcaraz N, Reino A, et al. Reconstruction of orbital floor fractures with maxillary bone. Arch Otolaryngol Head Neck Surg. 1998;124:56–59.
- Lai A, Gliklich RE, Rubin PA. Repair of orbital blow-out fractures with nasoseptal cartilage. Laryngoscope. 1998;108:645–650.
- Ducic Y, Verret DJ. Endoscopic transantral repair of orbital floor fractures. Otolaryngol Head Neck Surg. 2009;140:849–854.
- Nishiike S, Nagai M, Nakagawa A, et al. Endoscopic transantral orbital floor repair with antral bone grafts. Arch Otolaryngol Head Neck Surg. 2005;131:911–915.
- Whitehouse RW, Batterbury M, Jackson A, et al. Prediction of enophthalmos by computed tomography after ‘blow out’ orbital fracture. Br J Ophthalmol. 1994;78:618–620.
- Raskin EM, Millman AL, Lubkin V, et al. Prediction of late enophthalmos by volumetric analysis of orbital fractures. Ophthal Plast Reconstr Surg. 1998;14:19–26.
- Gray LN, Kalimuthu R, Jayaram B, et al. A retrospective study of treatment of orbital floor fractures with the maxillary sinus approach. Br J Plast Surg. 1985;38:113–115.