Abstract
We report a 48-year-old man presented with episodic rotatory vertigo accompanied by right hearing loss and headache. He did not have medical history of migraine. His hearing loss was progressive. He showed unilateral (right-sided) absence of cervical and ocular vestibular evoked myogenic potentials (cVEMP and oVEMP) to the right ear stimulation, while his caloric tests were normal on both sides. His signs and symptoms were suggestive of right peripheral vestibular vertigo except for headache. MRI revealed cerebellar arteriovenous malformation (AVM). Headache might be a sole cue for correct diagnosis. On the diagnosis of vertigo patients with headache, vertigo associated with secondary headache must be considered.
Introduction
Arteriovenous malformation (AVM) in the posterior cranial fossa is commonly presented with infratentorial hemorrhages [Citation1]. Hemorrhages may present as parenchymal, subarachnoid or intraventricular. Clinical manifestation of posterior fossa AVM could be headache, vomiting, cerebellar ataxia, and/or progressive neurological symptoms [Citation1].
We experienced a cerebellar AVM patient presented with vertigo which looks like peripheral vestibular origin accompanied by unilateral hearing loss and headache. Herein, we report the case.
Case presentation
A 48-year-old man visited our clinic with complaints of episodic rotatory vertigo accompanied by hearing loss in the right ear. He had these symptoms several times in one month. During vertigo attacks, he felt nauseous and sometimes vomited. He became unsteady during vertigo attacks. His vertigo lasted for several hours. He also complained of headaches preceding vertigo attacks. He had not had such a headache before.
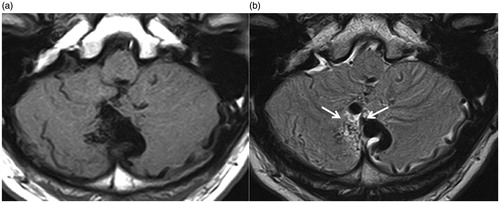
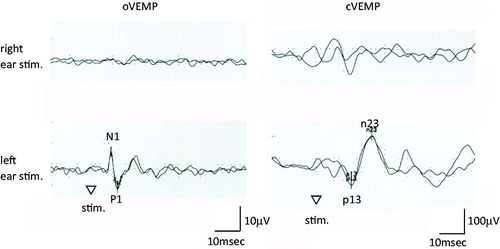
His tympanic membranes were normal. He showed mild sensorineural hearing loss in the right ear (). He showed direction-fixed left beating nystagmus. Stabilometry showed normal equilibrium. On electronystagmography, his pursuit, saccade, and optokinetic nystagmus were normal. Caloric tests were normal on both sides. Cervical and ocular vestibular evoked myogenic potentials (cVEMP and oVEMP) were absent to the right ear stimulation (air-conducted 500 Hz short tone bursts, 125 dBSPL) (). Recording methods of VEMPs were the same as those by Murofushi et al. [Citation2]. He also complained of progression of his hearing loss, which was confirmed by pure tone audiometry (). He did not show any other signs suggestive of cerebellar disorders or other cranial nerve disorders than the eighth cranial nerve.
Figure 1. Pure-tone audiogram. His right hearing loss was progressed in one month. O: right air-conducted hearing level; X: left air-conducted hearing level; [: right bone-conducted hearing level; ]: left bone conducted hearing level.
![Figure 1. Pure-tone audiogram. His right hearing loss was progressed in one month. O: right air-conducted hearing level; X: left air-conducted hearing level; [: right bone-conducted hearing level; ]: left bone conducted hearing level.](/cms/asset/291072db-434f-454f-8c06-2f040d553748/icro_a_1319735_f0001_c.jpg)
Figure 2. VEMP findings. 500 Hz short tone bursts (air-conducted, 125 dBSPL). cVEMPs were recorded on the sternocleidomastoid muscle ipsilateral to the stimulated ear, while oVEMPs were recorded just below the lower eye lid contralateral to the stimulated ear. Both of cVEMP and oVEMP were absent to the right ear stimulation (air-conducted 500 Hz short tone bursts, 125 dBSPL).
His clinical findings suggested vertigo due to peripheral vestibular disorders in the right. However, as he also complained of headache, which he had not had ever, he underwent assessment of the brain using MRI. Brain MRI revealed tiny vessels showing nidus and flow void of dilated draining vein in the cerebellar vermis (). On the basis of these MRI findings, he was diagnosed with having AVM in the cerebellum. His symptoms were considered to be caused by minor hemorrhages around AVM.
Discussion
The patient in this report was presented with episodic vertigo accompanied by unilateral progressive hearing loss and headache. Episodic vertigo accompanied by progressive hearing loss can be often experienced in cases with peripheral vestibular disorders. However, his brain MRI revealed tiny vessels showing nidus and flow void of dilated draining vein in the cerebellar vermis (). On the basis of these MRI findings, he was diagnosed with having AVM in the cerebellum. His symptoms were considered to be caused by minor hemorrhages around AVM. Headache, which he had not had ever, might be a sole cue for correct diagnosis. Hemorrhages in AVM may present as parenchymal, subarachnoid or intraventricular [Citation1]. Minor hemorrhages around the nidus, probably from the posterior inferior cerebellar artery or anterior inferior cerebellar artery, might cause his symptoms. Apart from minor hemorrhages around AVM which might also cause destruction or compression, ischemia by hemodynamic steal of blood flow and compression by winding vessels should be considered as a cause of his symptoms as well. Of course, we need to consider about the possibility of incidental discovery of AVM in a patient with peripheral vestibular disorders or vestibular migraine (VM). However, his vestibular symptoms were accompanied by headache although he had not severe headache before. It is also true that his brain MRI showed flow voids suggesting nidus without clear evidences of hemorrhages. These facts suggest that his symptoms should be caused by very minor hemorrhages in AVM.
Only a few similar cases have been reported. Kikuchi et al. [Citation3] reported a cerebellar AVM case presented with recurrent unilateral facial palsy accompanied by ipsilateral hearing loss and tinnitus. This patient also had a slight sensory disturbance on the left side of the face and the right lower extremity. Takai et al. [Citation4] reported a case with hemorrhage due to cerebellar AVM. Their case presented with rotatory vertigo and tinnitus. This patient also showed dysarthria later. These cases could be diagnosed with having peripheral vestibular problems because they also had cochlear symptoms. However, it was important that they also had other neurological symptoms and signs such as dysarthria or sensory disturbance. Then clinicians should consider vertigo of the central origin. On the other hand, our patient did not show any other symptoms or signs except for headache. He had not had ever serious headache. Headache was a sole cue to suspect diseases in the central nervous system. Nowadays, attention has been paid to VM as one of common clinical entities of vertigo [Citation5,Citation6]. However, prior to diagnosis of VM, vertigo associated with secondary headache must be excluded.
Disclosure statement
The authors do not have any conflicts of interest to declare.
Additional information
Funding
References
- Almeida JP, Medina R, Tamargo RJ. Management of posterior fossa arteriovenous malformations. Surg Neurol Int. 2015;6:31.
- Murofushi T, Nakahara H, Yoshimura E, et al. Association of air-conducted sound oVEMP findings with cVEMP and caloric test findings in patients with unilateral peripheral vestibular disorders. Acta Otolaryngol. 2011;131:945–950.
- Kikuchi M, Funabiki K, Hasebe S, et al. Cerebellar arteriovenous malformation with facial paralysis, hearing loss, and tinnitus: a case report. Otol Neurotol. 2002;23:723–726.
- Takai Y, Aoki K, Miyano K. A case of cerebellar hemorrhage with vertigo and tinnitus (in Japanese). Equilibrium Res. 2014;73:214–219.
- Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res. 2012;22:167–172.
- Murofushi T, Ozeki H, Inoue A, et al. Does migraine-associated vertigo share a common pathophysiology with Meniere’s disease? Study with vestibular evoked myogenic potential. Cephalalgia. 2009;29:1259–1266.