Abstract
Background: Few cases of bisphosphonate-associated ear canal osteonecrosis (BPECO) have been reported, and there are no established management strategies for the diagnosis or treatment of BPECO.
Patients: A 71-year-old female who was taking alendronate for osteoporosis was initially diagnosed with left-sided otitis externa. However, a mass and wide-ranging destruction of the temporal bone were subsequently found on a computed tomography scan. The patient’s biopsy findings were suggestive of inflammatory granulation tissue and osteitis, but there was no evidence of malignancy. So, we diagnosed her with BPECO. After surgical debridement and the cessation of the alendronate treatment, the patient’s symptoms improved rapidly.
Conclusions: BPECO is not a very well-known condition and so is often misdiagnosed. Diagnostic methods and treatments for BPECO should be established in future studies.
1. Introduction
In recent years, rare side effects of long-term bisphosphonate treatment, such as osteonecrosis of the external auditory canal, have been reported [Citation1–7]. Bisphosphonate-associated ear canal osteonecrosis (BPECO) is not a very well-known condition, and no diagnostic methods or treatments for the condition have been established. So, bisphosphonate-induced masses that destroy the auditory canal can often be misdiagnosed, for example, as ear canal otitis externa, cholesteatoma, or temporal bone malignancies. The previously reported cases of BPECO were diagnosed based on the patients’ medication history and computed tomography (CT) findings and were surgically treated via the removal of inflammatory granulation tissue and necrotic bone and the reconstruction of the ear canal with cartilage.
In this paper, we present a case of BPECO involving wider ranging destruction of the temporal bone than has previously been reported.
2. Case report
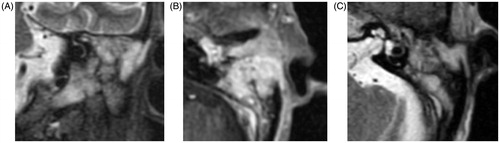
A 71-year-old female had been taking 70 mg/week alendronate for 11 years for osteoporosis. In May 2016, she presented with left-sided earache. She had been attending an ear, nose, and throat clinic for 5 months with otitis externa. She was referred to our hospital in September 2016 because her condition did not improve. An otological examination showed a mass that seemed to be composed of inflammatory granulation tissue. A CT scan demonstrated a region of soft tissue density involving the left external ear canal, middle ear cavity, and mastoid cells together with bone destruction (Figure ). Contrast-enhanced magnetic resonance imaging (MRI) showed an area of slightly high intensity (the same area as the region that demonstrated soft tissue density on CT). All of this region was enhanced. MRI also detected otitis of the temporal bone (based on the enhancement pattern) (Figure ). The patient’s right side was normal. A microbiological examination detected the growth of Pseudomonas species. Blood tests showed an elevated inflammatory response, but no increase in tumor marker levels, such as the levels of the soluble interleukin 2 receptor, carcinoembryonic antigen, squamous cell carcinoma antigen, cytoplasmic-antineutrophil cytoplasmic antibodies (C-ANCA), perinuclear-ANCA, immunoglobulin G4, and β-D glucan, were detected, and the T-SPOT test produced negative results. We performed a biopsy in the operation room after the patient’s hospitalization. The biopsy showed that the lesion was composed of inflammatory granulation tissue and otitis, but did not detect any evidence of malignancy. So, we diagnosed the patient with BPECO based on her from medication history, imaging findings, and pathological findings. In addition, blood tests ruled out ANCA-related angiitis, tuberculosis, etc. We reduced the size of the pathological lesion as much as possible and inserted a ventilation tube, and the patient’s symptoms improved rapidly. The bisphosphonate treatment was discontinued, and the patient continued taking calcium and vitamin D.
Figure 1. (A) Axial computed tomography scan of the left petrous temporal bone (B) Coronal computed tomography scan of the left petrous temporal bone showing osteonecrosis of the wall of the external auditory canal together with invasion into the mastoid bone (arrow).
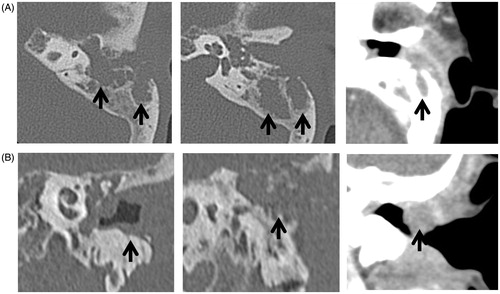
Figure 2. (A) T1-weighted coronal contrast-enhanced magnetic resonance image (B) T1-weighted axial contrast-enhanced magnetic resonance image (C) T2-weighted axial magnetic resonance image. On both T1- and T2-weighted imaging, high-intensity signals were seen in the same area as the region that exhibited soft tissue density on CT. Osteitis was also detected in the temporal bone.
3. Discussion
A growing number of patients are now receiving bisphosphonates for benign conditions, such as osteoporosis, and malignant conditions, such as breast cancer and multiple myeloma. Bisphosphonate-associated osteonecrosis of the jaws is relatively common, with hundreds of cases described in the literature [Citation8–10]. Bisphosphonate-associated osteonecrosis of jaws is defined as an area of exposed jawbone of more than 8 weeks’ duration in a patient taking oral or intravenous bisphosphonates. It is classified into four categories [Citation11] and treated according to the stage of the disease [Citation12].
Few cases of BPECO have been reported. To the best of our knowledge, the first report of possible BPECO was published in 2005, and 11 further cases have subsequently been reported (Table ). The majority of cases involved the elderly because they are vulnerable to osteoporosis. Nine patients had unilateral osteonecrosis, and all of the patients had been taking medication for more than 2 years. Most of these patients were diagnosed based on their medication history and CT findings and were treated surgically; i.e. the inflammatory granulation tissue and necrotic bone were removed, and the ear canal was reconstructed with cartilage. However, there are no established diagnostic methods or treatments for BPECO.
Table 1. Summary of the data from the present study and previous studies.
The case described in this paper involved wider-ranging destruction of the temporal bone than was seen in previously reported cases. We removed the pathological lesion as much as possible and inserted a ventilation tube. After the operation, the patient did not exhibit any symptoms, and her external auditory canal became well-epithelialized. However, there is a possibility that the pathological lesion has not been completely removed. So, the patient should be subjected to careful long-term follow-up to ensure that her condition does not deteriorate.
4. Conclusions
We describe a case of BPECO involving wider-ranging destruction of the temporal bone than has been seen in previously reported cases. BPECO is not a very well-known condition and so is often misdiagnosed. Diagnostic methods and treatments for the condition should be established in future studies.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Salzman R, Hoza J, Perina V, et al. Osteonecrosis of the external auditory canal associated with oral bisphosphonate therapy: case report and literature review. Otol Neurotol. 2013;34:209–213.
- Kharazmi M, Hallberg P, Persson U, et al. Bisphosphonate-associated osteonecrosis of the external auditory canal. J Craniofac Surg. 2013;24:2218–2220.
- Wickham N, Crawford A, Carney AS, et al. Bisphosphonate-associated osteonecrosis of the external auditory canal. J Laryngol Otol. 2013; 127:S51–S53.
- Bast F, Fuss H, Schrom T. Bilateral bisphosphonate-associated osteonecrosis of the external ear canal: a rare case. HNO. 2012;60:1127–1129.
- Froelich K, Radeloff A, Köhler C, et al. Bisphosphonate-induced osteonecrosis of the external ear canal: a retrospective study. Eur Arch Otorhinolaryngol. 2011;268:1219–1225.
- Polizzotto MN, Cousins V, Schwarer AP. Bisphosphonate-associated osteonecrosis of the auditory canal. Br J Haematol. 2006;132:114.
- Thorasteinsson AL, Lomholt AF, Eiken P. Bisphosphonate-induced osteonecrosis of the external auditory canal: a case report. J Clin Med Case Rep. 2015;2:3.
- Marx RE. Pamidronate (Aredia) and Zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–1117.
- Ruggio SL, Mehrotra B, Rosenberg TJ, et al. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of the 63 cases. J Oral Maxillofac Surg. 2004;62:527–534.
- Mavrokokki A, Cheng A, Stein B, et al. The nature and frequency of bisphosphonate associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg. 2007;65:415–423.
- Ruggiero SL, Dodson TB, Fantasia J, et al. American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaws-2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956.
- Comas-Calonge A, Figueiredo R, Gay-Escoda C. Surgical treatment vs. conservative treatment in intravenous bisphosphonate- related osteonecrosis of the jaws. Systematic review. J Clin Exp Dent. 2017;9:302–307.
