Abstract
COVID-19 was first reported of in December of 2019 and has since developed into a global pandemic disease. An intratonsillar abscess is a rarely encountered diagnosis and the clinical presentation can mimic that of a peritonsillar abscess. Here, we report on two cases of intratonsillar abscess and concurrent COVID-19 infection. Case 1: A 19-year old male presented with a sore throat, right-sided neck pain and difficulty swallowing. Needle aspiration of a peritonsillar bulging was negative for pus. Computed tomography showed an intratonsillar abscess. Intratonsillar needle aspiration was again negative for pus. The patient was treated with antibiotics and his condition improved without surgical intervention. Case 2: A 43-year-old female presented with a sore throat, difficulty swallowing, fever and myalgia. Examination showed peritonsillar swelling on the right side. Computed tomography showed an intratonsillar abscess on the right side. Intratonsillar needle aspiration was positive for pus. The patient was treated with antibiotics and her condition improved. To our knowledge, this is the first publication to report the development of intratonsillar abscess in patients with COVID-19.
Background
COVID-19 was first reported in Wuhan, China in December of 2019 and has since developed into a global pandemic disease [Citation1–3].
An intratonsillar abscess (ITA) has been described as a rare entity, presenting with symptoms similar to a peritonsillar abscess (PTA) albeit with a lower proportion of trismus, otalgia, dysphagia and progression of symptoms. One publication showed that ITA constitutes 7% of ITA and PTA combined [Citation4]. Needle aspiration is more frequently negative for pus compared with a PTA, and medical treatment rather than drainage procedures has been proposed [Citation4,Citation5]. Following two cases of ITA with concurrent COVID-19 within two weeks at our department, we performed a systematic PubMed search. No publications reporting ITA in patients with COVID-19 were found. The only publication found reporting head and neck abscesses as a potential complication of COVID-19 described two adolescent patients that developed periorbital abscesses [Citation6].
Here, two cases with intratonsillar abscess and concurrent COVID-19 infection are reported.
Case 1
A 19-year-old male presented at the Otorhinolaryngology Department on 8 June 2020, with a two-week history of a sore throat. For the past 48 h, the pain had intensified towards the right side of the throat. The patient had difficulty swallowing, opening his mouth fully and increased pain when turning his neck. He had no history of fever, shortness of breath, cough or gastrointestinal symptoms.
The patient had a medical history of surgery for cleft lip and palate and an asymptomatic persistent perforation of the right tympanic membrane after removal of a tympanostomy tube. The patient did not use any medications.
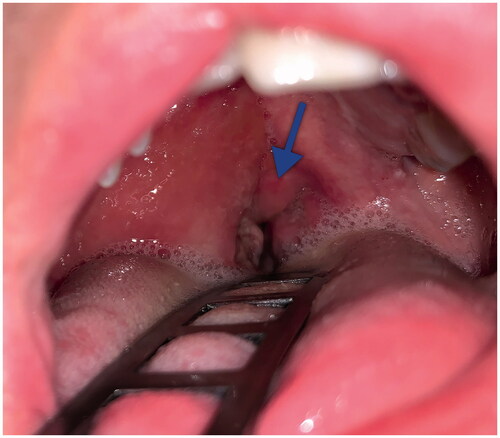
Physical examination at presentation revealed slight trismus and muffled speech, a bulging and erythematous soft palate on the right side, an ulcer on the right tonsil, uvular deviation to the left side and tender cervical lymph nodes on the right side (Figure ). Blood pressure, pulse rate, oxygen saturation and body temperature were all within normal ranges. Laboratory testing was significant for C-reactive protein elevation (CRP) at 276 mg/L and white blood cell count elevation at 12,300 cells/mm3 (neutrophil percentage was 85%).
Figure 1. Clinical presentation of the patient in case 1. The peritonsillar area on the right side is swollen and edematous. The uvula (arrow) is deviated to the left side.
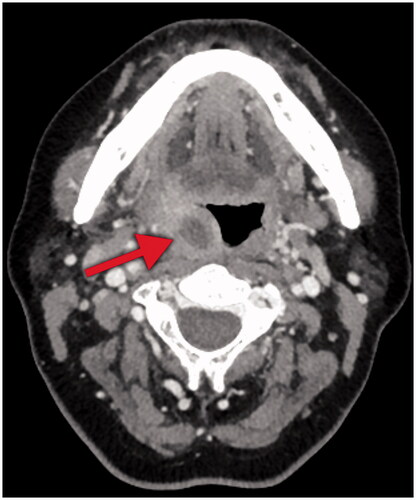
The initial clinical assessment was that the patient had developed a PTA. However, despite several needle aspirations in the peritonsillar area, no pus was detected. The patient was admitted and administration of intravenous benzylpenicillin (three grams, three times daily) was initiated. Computed tomography revealed a right-sided intratonsillar lesion indicating an abscess (Figure ). Intratonsillar needle aspiration of the lesion was performed but was again negative for pus. The patient was scheduled for a subacute tonsillectomy.
Figure 2. Computed tomography in the axial plane of the patient in case 1. Note the intratonsillar lesion (arrow) with low attenuation on the right side, measuring 26x19x20 millimeters, indicating an abscess.

Nasopharyngeal swab test (polymerase chain reaction) was positive for COVID-19 and nasopharyngeal culture showed Streptococcus pneumonia and Haemophilus influenza. As the patient’s general condition, laboratory findings and physical examination improved, a decision to delay surgery was taken. At day three, CRP was measured at 53 mg/L and white blood cell count was normalized to a level of 3,700 cells/mm3. The patient was discharged with oral phenoxymethylpenicillin (two grams, three times daily for ten days) and instructions to self-isolate during convalescence. He was scheduled for an elective tonsillectomy.
Case 2
A 43-year-old female with an increasingly sore throat, difficulty swallowing and myalgia was referred to the Otorhinolaryngology department from a primary care facility on 19 June 2020. The pain was initially confined to the right side of the throat but subsequently progressed to radiate towards the ipsilateral ear and neck. She had difficulty talking and opening her mouth. At the day of referral, she had developed fever. She had no history of shortness of breath, cough or gastrointestinal symptoms.
The patient had a medical history of previous cholecystectomy and surgery for breast cancer 14 months earlier with adjuvant chemoradiotherapy completed eight months earlier. She had no signs of recurrence. Current medications were Vitamin D supplementation and tamoxifen 20 milligrams daily.
Physical examination revealed trismus and there was a peritonsillar swelling on the right side. The uvula was deviated to the left. There was marked tenderness on neck examination. She had normal blood pressure and oxygen saturation, respiratory frequency of 20 breaths/minute, pulse rate of 100 beats/minute and a body temperature of 38.4 °C. Laboratory testing was significant for CRP elevation at 112 mg/L and white blood cell count at 8,000 cells/mm3 (neutrophil percentage was 81%).
The initial clinical assessment was that the patient had a PTA. Needle aspiration was performed in the right peritonsillar area, but no pus was detected. She was admitted and intravenous penicillin (three grams, three times daily) was initiated. Computed tomography showed an ITA rather than a PTA (Figure ). In a subsequent intratonsillar needle aspiration 1.5 mL of pus was detected. Nasopharyngeal swab test (polymerase chain reaction) was positive for COVID-19. The aspiration culture showed Streptococcus anginosus and various anaerobic bacteria. The patient’s condition improved, and she was discharged at day three with oral phenoxymethylpenicillin (two grams three, times daily for ten days) and low molecular weight heparin therapy for two weeks to prevent thrombosis. She was instructed to self-isolate during convalescence.
Discussion and conclusions
The COVID-19 pandemic, caused by the SARS-CoV-2 virus of the Coronaviridae family, has rapidly developed into a major threat to public health [Citation7]. To date, more than 46 million cases and 1.2 million deaths have been reported by the WHO [Citation8]. To our knowledge, this is the first publication to report the development of an ITA in patients with COVID-19. The cases presented to a University Hospital serving a population of approximately 300,000 people on 8 and 19 June 2020, respectively [Citation9]. One hundred and thirty-seven cases of COVID-19 were detected in this geographical area during the period 8–14 June 2020, corresponding to 4492 cases per 100,000 inhabitants [Citation10].
The ITA is a rarely encountered diagnosis and the clinical presentation can mimic that of a PTA. Previous reports have indicated that the frequency of needle aspiration positive for pus is lower for ITA than for PTA [Citation4,Citation5]. At our institution, it is customary to perform a computed tomography when there is a persistent suspicion of PTA after a negative aspiration. In case 1, although needle aspiration was negative for pus, the clinical presentation in addition to the radiologic findings strongly suggested an ITA. In case 2, on the other hand, needle aspiration was positive for pus, confirming the diagnosis. Both patients improved and could be discharged without a need of surgical intervention.
Ethics approval
Ethical approval was not sought for the present publication because it is not a requirement for case reports.
Informed consent
A written informed consent for participation was obtained from both patients.
Consent for publication
A written informed consent for publication was obtained from both patients. Copies of the statements can be provided upon request.
Author contributions
S.I and J.E took initiative to and collected information needed to complete this report. They also formulated the text. E.A helped collect data. L.F reviewed the report. All named authors have contributed, read and agreed to the submitted version of the manuscript.
| Abbreviations | ||
| ITA | = | intratonsillar abscess |
| PTA | = | peritonsillar abscess |
| CRP | = | C-reactive protein |
Acknowledgements
The authors thank the department of ENT at Örebro University Hospital. We also thank the two patients letting their cases be presented.
Disclosure statement
The authors declare that they have no competing interests.
Data availability statement
Data sharing is not applicable to this article as no datasets were generated or analysed in these case reports.
References
- Margallo LN, Diaz M, Lim PP. 2019 novel coronavirus pandemic: what do we know? S D Med. 2020;73:262–264.
- Da Silveira Cespedes M, De Souza JCP. Sars-CoV-2: a clinical update – II. Rev Assoc Med Bras (1992). 2020;66:547–557.
- Xie P, Ma W, Tang H, et al. Severe COVID-19: a review of recent progress with a look toward the future. Front Public Health. 2020;8:189.
- Ali SA, Kovatch KJ, Smith J, et al. Predictors of intratonsillar versus peritonsillar abscess: a case-control series. Laryngoscope. 2019;129:1354–1359.
- Ali SA, Kovatch KJ, Smith J, et al. Predictors of intratonsillar abscess versus peritonsillar abscess in the pediatric patient. Int J Pediatr Otorhinolaryngol. 2018;114:143–146. Nov
- Turbin RE, Wawrzusin PJ, Sakla NM, et. al. Orbital cellulitis, sinusitis and intracranial abnormalities in two adolescents with COVID-19. Orbit. 2020;39:305–310.
- Malik YS, Kumar N, Sircar S, et al. Coronavirus Disease Pandemic (COVID-19): challenges and global perspective. Pathogens. 2020;9:519.
- The World Health Organization. [accessed 2020 Nov 3]. Available from: http://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Regionfakta. [accessed 2020 Dec 17]. Available from: http://www.regionfakta.com/Orebro-lan/Befolkning-och-hushall/Befolkning/Folkmangd-31-december-alder
- Website. https://www.regionorebrolan.se/sv/Halsa-och-vard/Corona/Lagesbilder-och-statistik. Accessed 21 December 2020