Abstract
Neuro-Behçet’s disease (NBD) involves the nervous system and has a poorer prognosis. Since the typical delay in the onset of neurological symptoms is several years, difficulties are associated with diagnosing NBD when neurological disorders occur almost simultaneously with other major symptoms. We herein report a rare case of NBD that presented with the almost simultaneous manifestation of principal symptoms and neurological disorders.
A 32-year-old Japanese woman presented with severe pharyngitis with a white coating and ulcers. On the third day of admission, she suddenly fainted while walking with urinary incontinence. T2-weighted MRI showed multiple high-intensity signals in the brainstem. Genital ulcers and pseudofolliculitis on the back were also detected. Stabilometry showed principal involvement of the peripheral vestibular system. A cerebrospinal fluid examination revealed an increase in the number of cells with lymphocyte dominance. The interleukin-6 level was markedly elevated. Pulse corticosteroid therapy led to the attenuation of symptoms.
Introduction
Behçet’s disease (BD) is a multi-systemic, recurrent, inflammatory disorder of unknown etiology that presents with oral ulcers, uveitis, genital ulcers, and skin lesions. BD with nervous system involvement is called neuro-Behçet’s disease (NBD) [Citation1]. Neurological symptoms commonly develop later in the course of BD, with a typical delay of several years [Citation1–3]. Although the neurological manifestations of NBD do not occur as frequently as the major manifestations of BD, they are associated with a poor prognosis [Citation4].
We herein report a rare case of NBD, presenting with severe pharyngitis and the abrupt manifestation of neurological disorders, which led to its diagnosis.
Case report
A 32-year-old Japanese woman with an unremarkable medical history developed a sore throat and fever. Despite the oral administration of antibiotics and analgesics at a nearby clinic, her sore throat became aggravated with oral ulcers. On the sixth day after onset, pain prevented eating and, thus, she was referred to us for hospitalization and further treatment.
The patient presented with severe pharyngitis with a white coating and ulcers. Neutrophil-dominated leukocytosis (WBC 14,300/µL, neutrophils 87%) and an elevated C-reactive protein level (13.6 mg/dl) were noted. Growth was not detected on pharyngeal or blood cultures. She also had slight genital pain with ulcers.
Severe pharyngitis caused by a mixed bacterial and viral infection was suspected, and the intravenous administration of ceftriaxone (2 g/day) and clindamycin (1.2 g/day) was initiated. On the second day of admission, the patient was afebrile with the amelioration of pain. However, on the third day, she suddenly fell in the corridor with urinary incontinence. She was subsequently unable to walk because of staggering. Although she spoke slowly, disorientation was not noted. The patient started to weep abruptly, suggesting emotional incontinence, and fever also returned.
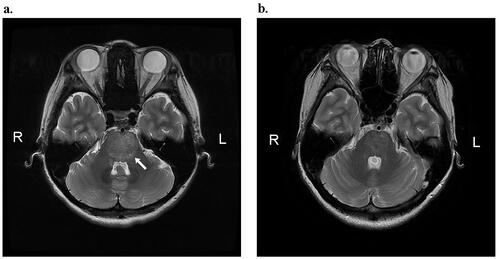
T2-weighted brain MRI showed multiple high-intensity signals in the cerebral crus, midbrain, pons, and medulla oblongata (Figure ). High intensity signals were not observed on diffusion-weighted MRI, suggesting that the lesions were edema, not infarction.
Figure 1. (a) T2-weighted brain MRI before treatment. The arrow indicates brainstem edema. (b) T2-weighted brain MRI after treatment. Brainstem edema was reduced.
Gaze-evoked nystagmus on lateral gaze was noted in a neurological examination. A cerebrospinal fluid (CSF) examination by neurologists revealed an increase in the number of cerebrospinal fluid cells (283/µL) with 28% polynuclear cells. The total protein level was 36 mg/dL and the glucose level was 59 mg/dL. The interleukin-6 level (IL-6) was 589 pg/mL. manifesting a marked elevation. An ophthalmic examination revealed no abnormalities. In a general examination, genital ulcers were confirmed and pseudofolliculitis on the back was detected.
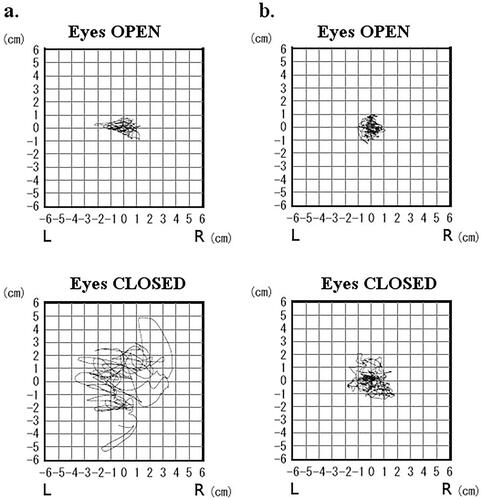
Meningoencephalitis caused by NBD was diagnosed. The patient received pulse corticosteroid therapy (PCT) with 1000 mg of methylprednisolone for 3 days, followed by 40 mg/day of prednisolone for one week as maintenance therapy. The dose of prednisolone was reduced by 10 mg per week. The neurological symptoms gradually attenuated. However, stabilometry soon after PCT still showed abnormal patterns, which were more prominent when the eyes were closed. The following parameters were increased: enveloped area (eyes closed: 30.4 cm2, open: 2.2 cm2), locus length per second (eyes closed: 5.4 cm/s, open: 1.8 cm/s), and a Romberg rate of 13.6 (Figure ). The patient was discharged approximately 1 month after the onset of symptoms.
Follow-up stabilometry approximately 1.5 months after onset revealed a normal postural equilibrium (Figure ). Follow-up brain MRI in the same period showed a marked reduction in edema (Figure ). Her CSF IL-6 level returned to a normal level 2 months after her discharge (1.1 pg/mL). She repeatedly developed oral and genital ulceration without the exacerbation of neurological symptoms for 1 year under maintenance therapy with colchicine and prednisolone.
Discussion
BD is a systemic inflammatory disease that is typically characterized by recurrent oral aphthous ulcers, uveitis, genital ulcers, and skin lesions. Although the etiology of BD remains unknown, genetic and environmental factors are considered to be important in its pathogenesis. The prevalence of BD is higher in countries along the ancient ‘Silk Road’: it ranges between 13.5 and 85 per 100,000 population in Asian countries, such as Iran, Korea, China, and Japan [Citation5], and is markedly lower at between 0.12 and 0.64 per 100,000 population in Western countries [Citation6,Citation7]. The present case met the criteria of the International BD Study Group (oral, genital, and skin lesions) [Citation8].
Neurological involvement in BD is rare, but has a poorer prognosis. It has been reported in 5.3 − 14.3% of BD cases [Citation9–11]. Brainstem edema in MRI and an elevated IL-6 level in CSF are characteristic of NBD [Citation8]. Nervous system complications typically develop several years after the onset of the major symptoms of BD [Citation1–3]. The clinical course of the present case was rare because neurological disorders developed soon after the onset of the major symptoms of BD. A few similar cases have been reported in the literature [Citation12].
Based on its clinical course, NBD is classified into acute and chronic progressing types [Citation13]. No progression is principally observed in acute-type NBD; however, neurological symptoms sometimes recur [Citation13]. Chronic-type NBD is an intractable and progressive disease. Neurological manifestations lead to severe disability despite empirical immunotherapy [Citation13]. The present case is compatible with the acute type due to its abrupt manifestation with negligible progression.
Neurological involvement of the vestibular system has been reported [Citation14,Citation15]. The site of involvement may be peripheral as well as central. In the present case, stabilometry principally indicated peripheral disorders, which subsided after treatment.
Difficulties are associated with diagnosing BD (NBD) when neurological disorders occur almost simultaneously with other major symptoms. Moreover, these patients may consult several departments, including otolaryngology, dermatology, gynecology, and neurology, receiving multiple independent diagnoses. The present case draws attention to this possibility, and encourages the sharing of information among departments.
Conclusion
A case of acute pharyngitis with the abrupt manifestation of neurological disorders, which led to a diagnosis of Neuro-Behçet’s disease (NBD), was reported. NBD is a form of Behçet’s disease that involves the nervous system and has a poorer prognosis. The typical delay in the onset of neurological symptoms is several years. Difficulties are associated with diagnosing NBD when neurological disorders occur almost simultaneously with other major symptoms. The sharing of information among several departments is important for the diagnosis of NBD.
Ethical approval
Written informed consent was obtained from the patient for the presentation of clinical findings.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Akman-Demir G, Serdaroglu P, Tasçi B, The Neuro-Behçet Study Group. Clinical patterns of neurological involvement in Behçet's disease: evaluation of 200 patients. Brain. 1999;122(Pt 11):2171–2181.
- Kidd D, Steuer A, Denman AM, et al. Neurological complications in Behçet's syndrome. Brain. 1999;122(Pt 11):2183–2194.
- Siva A, Kantarci OH, Saip S, et al. Behçet's disease: diagnostic and prognostic aspects of neurological involvement. J Neurol. 2001;248(2):95–103.
- Haghighi AB, Pourmand R, Nikseresht A-R. Neuro-Behçet disease. A review. Neurologist. 2005;11(2):80–89.
- Lawton G, Bhakta BB, Chamberlain MA, et al. The Behcet's disease activity index. Rheumatology. 2004;43(1):73–78.
- Mendes D, Correia M, Barbedo M, et al. Behçet's disease-a contemporary review. J Autoimmun. 2009;32(3–4):178–188.
- Savey L, Resche-Rigon M, Wechsler B, et al. Ethnicity and association with disease manifestations and mortality in Behçet's disease. Orphanet J Rare Dis. 2014; 9:42.
- Al-Araji A, Kidd DP. Neuro-Behçet's disease: epidemiology, clinical characteristics, and management. Lancet Neurol. 2009;8(2):192–204.
- Serdaroglu P, Yazici H, Ozdemir C, et al. Neurological involvement in Behçet’s syndrome—a prospective study. Arch Neurol. 1989;46:265–269.
- Ashjazadeh N, Borhani Haghighi A, Samangooie S, et al. Neuro-Behçet’s disease: a masquerader of multiple sclerosis. A prospective study of neurologic manifestations of Behçet’s disease in 96 Iranian patients. Exp Mol Pathol. 2003;74(1):17–22.
- Al-Araji A, Sharquie K, Al-Rawi Z. Prevalence and patterns of neurological involvement in Behcet's disease: a prospective study from Iraq. J Neurol Neurosurg Psychiatry. 2003;74(5):608–613.
- Tsunemi T, Sakai Y, Tsunoda K, et al. Neuro-Behçets/neuro-Sweets disease presents simultaneously with severe tonsillitis, and features mimicking bacterial meningitis with skin lesions. Intern Med. 2006;45(22):1315–1317.
- Hirohata S. Potential new therapeutic options for involvement of Central nervous system in Behçet’s disease (Neuro-Behçet’s syndrome). CRR. 2007;3(4):297–303.
- White AS, Taylor RL, McNeill C, et al. Behçet's disease presenting as a peripheral vestibulopathy. J Clin Neurosci. 2014;21(6):1060–1063.
- Sugita-Kitajima A, Koizuka I. Neuro-Behçet's disease with dizziness. Auris Nasus Larynx. 2010;37(2):229–232.