Abstract
Median palatal cyst is a rare nonodontogenic facial cleft cyst. A case of median palatal cyst was admitted to the Department of Otolaryngology, Renji Hospital. A 26-year-old female patient was admitted with ‘repeated bilateral nasal congestion for two years’ and was diagnosed as a median palatal cyst. Endoscopic resection of the cyst at the bottom of the nose plus free nasal septal cartilage transplantation were performed. The wound healed well and the cyst did not recur after one year of follow-up.
Keywords:
Case report
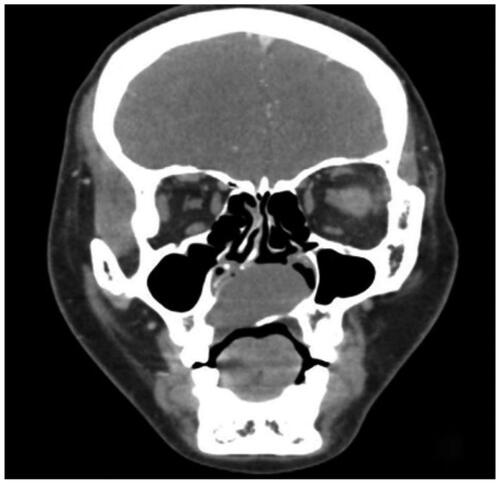
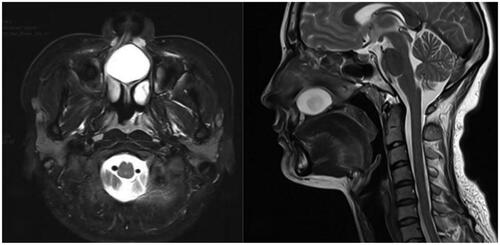
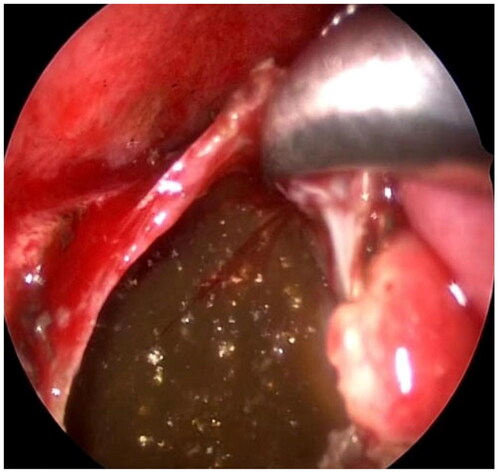
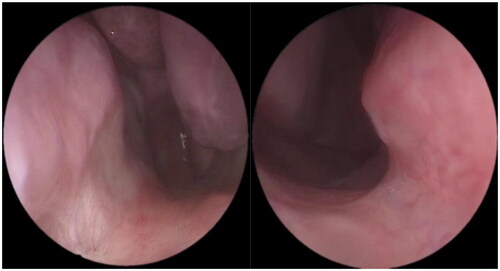
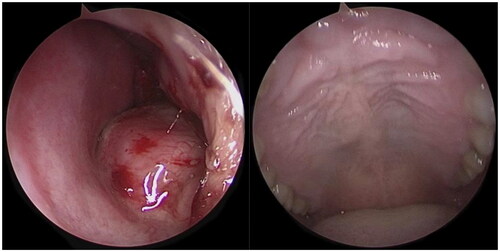
The patient, a 26-year-old female, was admitted to the hospital on 14 February 2022 due to recurrent bilateral nasal congestion for two years. On physical examination, the patient presented with a normal nasal appearance, nasal septum deviation to the right, slight bulging of the right nasal floor, noticeable bulging of the mucosa of the left nasal floor and inferior nasal septum, normal mucosal color, soft palpation, and no movement, no pain, and no obvious bulging of the hard palate. Nasal endoscopy revealed a round bulging neoplasm extending from the left nasal floor to the bottom of the nasal septum, slight elevation at the right nasal floor, and a non-bulging palate (Figure ). Enhanced computed tomography (CT) of the maxillofacial region showed a circle of expansive bone destruction and osteolytic bone destruction in the medial maxilla, slightly to the right, and compression of the nasal septum to the right, with a range of approximately 32 × 32 mm, the CT value was approximately 36 HU (Figure ). Enhanced magnetic resonance imaging (MRI) of the maxillofacial region showed an abnormal cystic signal shadow in nasal septal area just above the maxilla, with short T1 and long T2 signals, compression of the surrounding tissue, and partial right deviation of the nasal septum. The lesion size was approximately 30 × 20 × 33 mm, with no noticeable enhancement (Figure ). Clinically diagnosed as a median palatal cyst. After admission, under general anesthesia, cystectomy, and accessible septum cartilage transplantation were performed under nasal endoscopy through the nasal floor. The surgical steps were as follows. (1) The extent of the cyst was determined. The cyst was removed entirely: the left side extended to the lower edge of the medial wall of the maxillary sinus, the right side advanced to the middle of the right nasal cavity, the front rose to the level of the upper incisors, and the lower side extended to the surface of the hard palate. A large number of cholesterol crystals were seen in the cyst (Figure ). The entire cyst wall at the left nasal floor was excised, and part of the cyst wall at the right nasal floor was removed. The hard palate was explored and was determined to be intact without perforation. (2) The mucosal tissue was restored. The right nasal floor cartilage and mucosa were folded outwards and upwards, and the defect, one-third of the anterior nasal septum cartilage was observed; the left and right nasal cavities were connected at the nasal floor. (3) The defect was filled. An incision of approximately 2 cm in length was made along the junction of the skin and mucous membranes of the left nasal septum to the nasal floor. The mucosa on both sides of the nasal septal cartilage was separated under the endoscope. A part of the nasal septal cartilage (approximately 2 × 3 cm) was cut and placed in the lower part of the nasal septum. A pedicled left septal mucosal flap was prepared, transferred, and fixed at the left nasal floor. (4) The surgical site was packed. The bilateral nasal cavity was filled with a sponge; the packing was removed 48 h after the operation. After the operation, the nasal mucosa incision had healed well, and the patient had no nasal congestion, no nasal discharge, and no nasal septum perforation. The hard palate was intact without perforation. No recurrence was seen at one year of follow-up (Figure ).
Figure 1. A nasal endoscopy shows a bulge from the left floor of the nose to the bottom of the nasal septum, but there is no bulge in the palate.
Discussion
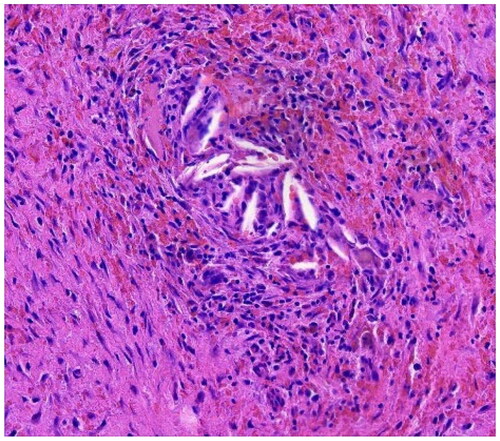
Median palatine cyst (MPC) is a rare nonodontogenic facial cleft cyst located behind the incisive papilla on the midline of the palate. It mainly develops from the remaining epithelial embryonic tissue of the palatal bone. MPC accounts for only 7.14% of all jaw cysts [Citation1]. The process of its formation is still under debate; it was initially thought that in the sixth embryonic week if the midline of the palatine process does not form ultimately, the residual ectodermal epithelial cells can form cysts [Citation2]. Some scholars propose that an MPC is the posterior extension of a nasopalatine duct cyst [Citation3]. Histologically, MPCs resemble squamous or columnar epithelium and fibrous connective tissue. In addition, there are inflammatory infiltrates of different intensities under the epithelium of the cyst wall, and lymphocytes, plasma cells, cholesterol crystals, and foreign body giant cells can be observed inside, a presentation similar to that in this case study (). The deposition of cholesterol crystals occurs due to the breakdown of erythrocytes, lymphocytes, plasma cells, and macrophages.
Figure 6. Pathological tissue shows a large number of inflammatory cell infiltrates and cholesterol crystals. Hematoxylin-eosin staining 100.
Cysts located in the middle of the palatine process are mostly asymptomatic in the early stage. As cysts expand into the nasal floor, nasal congestion, pain, swelling of the nose, and numbness of the upper lip will occur, which can cause bulging of the nasal floor, upper lip, and palate. The distending changes can cause damage to the hard palate and the nasal floor, resulting in local deformities. MPC should be differentiated from odontogenic cysts; therefore, it is essential to examine the dental and periodontal conditions. Some scholars have described the diagnostic criteria for MPC: the cyst must be located posterior to the palatal papilla; the location of the cyst on the palatal midline should be roughly symmetrical; the cyst should not be associated with the incisor canal or teeth; and the shape of the cyst should be round, pear-shaped, or oval; histologically, the cyst wall should be without hyaline cartilage, large blood vessels, or salivary glands [Citation4–6].
There are many ways to treat MPC. Surgery aims to remove the cyst, strip away as much of the cyst wall as possible and restore the normal appearance of the nasal floor or palate. The current surgical methods include the transoral and trans palatal approach, the labial gingival sulcus approach, and the transnasal floor approach. Some clinicians used the upper labial gingival sulcus approach in the early stage with a palatal bulge incision. First, Manzon et al. [Citation7] used an 18-gauge needle with a diameter of approximately 4 cm to decompress the lesion. The puncture fluid contained dark brown substances containing cholesterol deposits, and malignant lesions were excluded. Finally, the cyst was excised through the trans palatal approach. Therefore, for larger cysts, decompression can be performed through puncture and aspiration, and then, complete cyst resection can be achieved. In 2012, the case of a 14-year-old male patient was reported by Kim et al. [Citation8]. A cyst (approximately 53 × 46 × 43 mm) was found at the distal end of the palatal papilla. The cyst was excised through a midline incision of the palate and an upper gingival incision. Oronasal fistula occurred 13 months after the operation. The fistula and the surrounding scar tissue were removed by surgery, the free oral mucosa flap was rotated, and the palate was reconstructed. There was no recurrence or fistula in the 3-year follow-up after the operation. In 2018, a case of isolated oval swelling (approximately 20 × 30 mm) in the midline palate was reported by Rangaswamy[Citation1]. To excavate the lesion, local anesthesia was used to lift the mucosa and periosteum flap through the palate. A palatal incision is associated with a risk of wound infection and high suture tension; the labial gingival sulcus incision can easily damage the infraorbital nerve and alveolar nerve, which can cause facial swelling, lip numbness, gingival fistula, other complications after surgery. If the mucosa of the nasal floor is ruptured during the operation, an oronasal fistula can form.
With the development of nasal endoscopy, minimally invasive surgery using direct vision with nasal endoscopy has become popular in China because of fewer complications. In the patient in this case study, the cyst was large, and the disease course was long. Part of the nasal septum cartilage had been absorbed and destroyed, accounting for 1/3 of the anterior segment defect. Therefore, intraoperative free nasal septal cartilage was required for reconstruction, and a nasal floor flap was used for the repair. The patient was satisfied with the surgical results. If the defect of the palate and the nasal floor is minor, it can be temporarily filled with gauze or a sponge. A local rotating flap can be designed to reconstruct the defect without tension for patients with obvious signs of a palatal mass, thinning bone, or significant defects. Therefore, estimating the surgical wound and necessary flap reconstruction before surgery is very important. Notably, the mucosa of the nasal floor must be protected to prevent the occurrence of oronasal fistulas.
Klebsiella aerogenes was observed in cultured pus of the patient in this case study, serving as the first case of such disease reported in domestic and foreign literature. The MRI in Figure shows a low-density shadow in the middle of the cyst. It is speculated that Klebsiella produces formic hydrogenase and obtains energy through glucose fermentation, facilitating gas formation in pus under an acidic environment. After evident bacterial culture and drug susceptibility test results, sensitive antibiotics were used postoperatively.
We believe that MPC resection under nasal endoscopy has the advantages of a clear field of vision, adequate exposure of anatomical structures, delicate operation, low risk, less trauma, no need for nasal feeding after operation, and fewer complications, e.g. oronasal fistula. The patient and his family were delighted with the postoperative effect, and this procedure is recommended for clinical promotion.
Informed consent
Written informed consent was obtained from the patient for the publication of these findings.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Rangaswamy S, Singh M, Yumnum R. True median palatal cyst; a rare case report. J Oral Maxillofac Pathol. 2018;22(2):286. doi: 10.4103/jomfp.JOMFP_199_17.
- Kramer IR, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumours. A commentary on the second edition. Cancer. 1992;70(12):2988–2994. doi: 10.1002/1097-0142(19921215)70:12<2988::AID-CNCR2820701242>3.0.CO;2-V.
- Rapidis AD, Langdon JD. Median cysts of the jaws–not a true clinical entity. Int J Oral Surg. 1982;11(6):360–363. doi: 10.1016/s0300-9785(82)80059-8.
- Hadi U, Younes A, Ghosseini S, et al. Median palatine cyst: an unusual presentation of a rare entity. Br J Oral Maxillofac Surg. 2001;39(4):278–281. doi: 10.1054/bjom.2001.0620.
- Karaçal N, Ambarcoğlu O, Kutlu N. Median palatine cyst: report of an unusual entity. Plast Reconstr Surg. 2005;115(4):1213–1214. doi: 10.1097/01.prs.0000157510.37851.2a.
- Gingell JC, Levy BA, DePaola LG. Median palatine cyst. J Oral Maxillofac Surg. 1985;43(1):47–51. doi: 10.1016/s0278-2391(85)80013-6.
- Manzon S, Graffeo M, Philbert R. Median palatal cyst: case report and review of literature. J Oral Maxillofac Surg. 2009;67(4):926–930. doi: 10.1016/j.joms.2008.06.103.
- Kim SW, Seo BF, Baek SO, et al. Large median palatine cyst. J Craniofac Surg. 2012;23(4):e288-90–e290. doi: 10.1097/SCS.0b013e31824e5c33.