Abstract
Septic arthritis of the sternoclavicular joint is a rare condition. The diagnosis of sternoclavicular septic arthritis as a late complication of surgical tracheostomy is extremely uncommon. A case study is presented of a man in his 70s who experienced painful swelling of the right sternoclavicular joint three months after elective surgical tracheostomy. The diagnosis was made based on clinical history and examination. The patient achieved a full recovery following antibiotic treatment and surgical drainage. This report is the second documented case of sternoclavicular septic arthritis resulting from surgical tracheostomy.
Introduction
Surgical tracheostomy is a surgical procedure that creates a semi-permanent or permanent connection between the trachea and the skin. It was developed by Trousseau in the nineteenth century to relieve respiratory obstruction in patients with diphtheria [Citation1]. Complications associated with this procedureCitation2 can be classified as immediate, occurring during the surgical procedure (such as bleeding, pneumothorax, and pneumomediastinum). Infections and pressure ulcers are considered early postoperative complications, while tracheal stenosis, tracheocutaneous, tracheoinnominate and tracheoesophageal fistulas are considered late postoperative complications.
Septic arthritis of the sternoclavicular joint is a rare clinical condition, accounting for only 1% of all cases of septic arthritis [Citation3]. It can lead to serious complications such as thoracic abscesses, osteomyelitis, mediastinitis and bacteremia [Citation3]. Risk factors for sternoclavicular arthritis include immunosuppressant drugs, intravenous drugs, chronic kidney disease, cancer, chemotherapy, and diabetes mellitus [Citation4]. Although cases in healthy adults have also been described [Citation5], septic arthritis as a late complication of surgical tracheostomy is very unusual. The authors report the second case of septic arthritis of the sternoclavicular joint following surgical tracheostomy.
Patient information
A 72-year-old man presented to the emergency department (ED) with a two-week history of fever, pain, and reduced range of motion in his right upper limb. The patient had been diagnosed with squamous cell carcinoma of the hypopharynx approximately three months ago (cT3N2aM0) and was recommended for radical chemoradiotherapy. He underwent an elective surgical tracheostomy (Bjork flap technique) at the time of diagnosis due to airway risk, which was uneventful. The patient had a medical history of hypopharynx cancer and type 2 diabetes mellitus. He did not smoke, but was a social drinker and denied any intravenous or recreational drug use.
Clinical findings
Upon presentation, he had a fever and normal blood pressure. His oxygen saturation was 99% on air. During the initial examination, he exhibited a reduced range of motion in his right upper limb and a painful, red swelling in the area of the right sternoclavicular joint without fluctuation. The tracheostoma was open, with granulation tissue present at 12 h and minor serohematic drainage. There were no signs of pus or fistulization. An indirect laryngoscopy revealed an ulcerative-vegetative lesion implanted on the medial wall of the left piriform sinus, with left vocal cord paralysis.
The initial baseline blood test showed a hemoglobin level of 8.8 g/dL, normal white cell count, and raised inflammatory markers: C-reactive protein of 129 mg/dL (normal range: <0.5 mg/dL) and sedimentation rate of 103 mm/h (normal range: <15 mm/h). Blood cultures were negative.
Diagnostic assessment
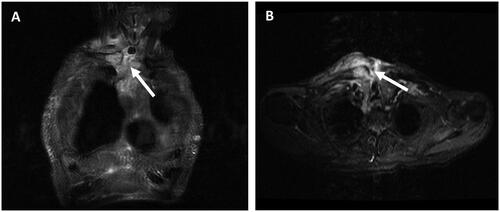
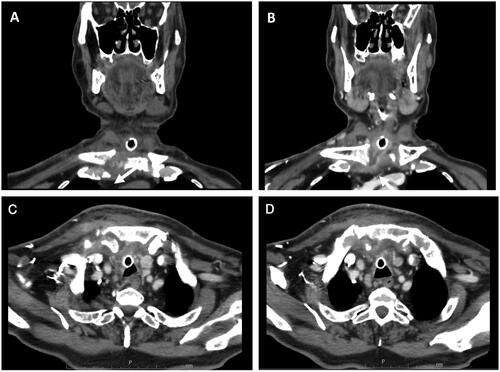
A CT scan with contrast was performed on the head, neck and chest. The results showed effusion in the right sternoclavicular joint, with thickening and increased synovial uptake (Figure ), irregularity of the clavicular and sternal cortical bone (Figure ), with erosion and inflammatory changes in the soft tissues adjacent to the tracheostomy. The contrast-enhanced MRI of the head, neck, and chest revealed a suppurative collection adjacent to the tracheostomy and a fistulous path between the referred liquid collection and the sternoclavicular joint effusion, in the plane immediately above the sternal notch (Figures ).
Figure 1. (A) Coronal and (C) Axial contrast-enhanced CT of the head, neck and chest shows irregularity of the right clavicular and sternal cortical bone (arrows). (B) Coronal and (D) Axial contrast-enhanced CT of the head, neck and chest shows effusion in the right sternoclavicular joint, with thickening and increased synovial uptake.
Therapeutic intervention
The patient received treatment with intravenous antibiotics (ceftriaxone 2 g id) and anti-inflammatory drugs (dexamethasone 4 mg id, cetorolac 40 mg 2id and paracetamol 1000 mg 3id). Urgent surgical debridement and drainage of intra-articular content were performed. The pus culture was positive for Prevotella buccae and Streptococcus constellatus, both sensitive to ceftriaxone. Intravenous antibiotics were continued. One week after the initial surgery, the patient’s complaints persisted and inflammatory parameters worsened (C-reactive protein of 220 mg/dL and sedimentation rate of 87 mm/h, with normal white cell count). As a result, the patient underwent a second drainage procedure to remove intra-articular content and a piecemeal resection of necrotic bone (sternal manubrium and clavicular end). Microbiologic analysis revealed a positive result for Escherichia coli, which was sensitive to amoxicillin with clavulanic acid. The patient received intravenous antibiotics (amoxicillin with clavulanic acid, 2.2 g 3 times a day) for three weeks and was discharged four weeks after admission with significant clinical improvement. The patient’s inflammatory parameters were normalized, with a C-reactive protein level of 7.9 mg/dL and a sedimentation rate of 58 mm/h. The anatomopathological study of the resected tissues was negative for malignancy.
The patient completed a six-week course of antibiotics, taking amoxicillin with clavulanic acid 875 + 125 mg twice daily by mouth.
Follow-up and outcomes
Two weeks later, he was evaluated in the outpatient clinic and was found to be symptom-free. Chemoradiotherapy for the squamous cell carcinoma of the hypopharynx began one month later.
Discussion
The authors report a case of septic arthritis of the sternoclavicular joint following surgical tracheostomy. The patient became symptom-free after a six-week course of antibiotics and two surgical interventions. The sequence of events likely began with an infection of the tracheostoma, followed by contiguous infection of the surrounding anatomy, including the right sternoclavicular joint. This is only the second reported case [Citation6]. Septic arthritis of the sternoclavicular joint is a rare and potentially fatal infection. Septic joints that are left untreated can result in a mortality rate of up to 10% and morbidity of over 30%, with abscess formation prevalence as high as 80% [Citation7,Citation8].
It is extremely rare for this condition to be identified as a late complication of surgical tracheostomy. While infection is a relatively common early complication of surgical tracheostomies, it typically involves infection of the skin around the stoma rather than the adjacent joint [Citation2]. The presentation of this condition is usually indolent or subacute [Citation9]. The clinical features of the reported case include fever, chest pain localized to the joint, shoulder pain, reduced upper limb mobility, and local erythema [Citation3]. Leukogram findings were consistently normal [Citation10]. Risk factors most commonly associated with this entity are cancer and immunosuppression [Citation11,Citation12]. In this case, the patient had type 2 diabetes mellitus and hypopharyngeal carcinoma.
Staphylococcus aureus is responsible for up to two-thirds of cases [Citation3], with the remaining cases caused by Pseudomonas aeruginosa (10%), Brucella melitensis (9%), Escherichia coli (5%), and Mycobacterium tuberculosis (<5%). The microorganisms identified in this case were Prevotella buccae, Streptococcus constellatus, and Escherichia coli. Prevotella buccae is a gram-negative anaerobic bacterium that is part of the oral, urogenital, and intestinal microbiota. Respiratory tract infections are commonly associated with it. Additionally, it has been linked to cases of osteomyelitis and periodontal disease [Citation13]. Streptococcus constellatus is a gram-negative coccus that is also present in the oral, urogenital, and intestinal microbiota. It is typically associated with abscess formation in the upper half of the body and respiratory tract [Citation14]. In contrast, Escherichia coli is a gram-negative bacillus found in the intestinal microbiota. Polymicrobial septic arthritis is a relatively rare condition that is often associated with gastrointestinal and genitourinary infections [Citation15]. In cases where small and intermediate joints, such as the sternoclavicular joint, are affected, the condition is more likely to be polymicrobial and caused by Streptococcus, Eikenella, or anaerobic bacteria [Citation16].
To diagnose sternoclavicular arthritis, a CT and MRI of the head, neck, and chest should be performed to determine the extent of the infection and associated bone destruction. Bone scintigraphy can aid in distinguishing between infection and degenerative changes in the joint [Citation17].
The initial step in the therapeutic approach should be intravenous antibiotics. It is recommended to use broad-spectrum antibiotics in the beginning, followed by spectral reduction after microbiological results. The most commonly used antibiotics are cephalosporins, vancomycin, and fluoroquinolones [Citation18]. The duration of treatment varies depending on the severity of the infection. When there is bone involvement, it is recommended to undergo four to six weeks of treatment [Citation19].
Surgical intervention is especially relevant in cases where there is bone involvement, abscess, or a collection of periarticular fluid [Citation20]. En bloc joint resection is the most effective procedure, although other procedures such as simple debridement and piecemeal resection of the affected tissue may also be used. Following the surgical procedure, a dressing with negative pressure should be applied, particularly in more extensive approaches, to promote the formation of granulation tissue and closure of the surgical wound. Hyperbaric oxygen therapy is an alternative treatment option [Citation3]. Postoperative complications may include empyema, pleural effusion, abscess, mediastinitis, and sepsis [Citation21,Citation22]. In our case, high-dose antibiotics and two surgical procedures were used to manage the condition, resulting in complete resolution of symptoms.
Conclusion
Septic arthritis of the sternoclavicular joint is a rare condition, accounting for only 1% of all cases of septic arthritis. It is an extremely uncommon complication of surgical tracheostomy. This condition can have life-threatening complications that require aggressive medical management and surgery.
Informed consent statement
Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Disclosure statement
The authors report there are no competing interests to declare.
References
- Frost EA. Tracing the tracheostomy. Ann Otol Rhinol Laryngol. 1976;85(5 Pt.1):618–624. doi:10.1177/000348947608500509.
- Das P, Zhu H, Shah RK, et al. Tracheotomy-related catastrophic events: results of a national survey. Laryngoscope. 2012;122(1):30–37. doi:10.1002/lary.22453.
- Tanaka Y, Kato H, Shirai K, et al. Sternoclavicular joint septic arthritis with chest wall abscess in a healthy adult: a case report. J Med Case Rep. 2016;10:69. doi:10.1186/s13256-016-0856-0.
- Ross JJ, Shamsuddin H. Sternoclavicular septic arthritis: review of 180 cases. Medicine (Baltimore). 2004;83(3):139–148. doi:10.1097/01.md.0000126761.83417.29.
- Bar-Natan M, Salai M, Sidi Y, et al. Sternoclavicular infectious arthritis in previously healthy adults. Semin Arthritis Rheum. 2002;32(3):189–195. doi:10.1053/sarh.2002.37284.
- Sharif KF, Baik FM, Jategaonkar AA, et al. Septic arthritis of the sternoclavicular joint: a unique late complication after tracheostomy. Am J Otolaryngol. 2018;39(5):646–648. doi:10.1016/j.amjoto.2018.05.005.
- Septic arthritis of the sternoclavicular joint. J Am Board Fam Med. 2012;25(6):908–912. Womack J. doi:10.3122/jabfm.2012.06.110196.
- Thompson MA, Barlotta KS. Septic arthritis of the sternoclavicular joint. J Emerg Med. 2018;55(1):128–129. doi:10.1016/j.jemermed.2018.02.044.
- Yood RA, Goldenberg DL. Sternoclavicular joint arthritis. Arthritis Rheum. 1980;23(2):232–239. doi:10.1002/art.1780230215.
- Tasnim S, Shirafkan A, Okereke I. Diagnosis and management of sternoclavicular joint infections: a literature review. J Thorac Dis. 2020;12(8):4418–4426. doi:10.21037/jtd-20-761.
- Song HK, Guy TS, Kaiser LR, et al. Current presentation and optimal surgical management of sternoclavicular joint infections. Ann Thorac Surg. 2002;73(2):427–431. doi:10.1016/s0003-4975(01)03390-2.
- Nguyen M, Moffatt-Bruce SD, Merritt RE, et al. Clinical Effectiveness of Negative Pressure Wound Therapy Following Surgical Resection of Sternoclavicular Joint Infection: a Case Report. Cureus. 2016;8(10):e815. doi:10.7759/cureus.815.
- Tanaka S, Yoshida M, Murakami Y, et al. The relationship of Prevotella intermedia, Prevotella nigrescens and Prevotella melaninogenica in the supragingival plaque of children, caries and oral malodor. J Clin Pediatr Dent. 2008;32(3):195–200. doi:10.17796/jcpd.32.3.vp657177815618l1.
- Claridge JE, Attorri S, Musher DM, et al. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (“Streptococcus milleri Group”) Are of Different Clinical Importance and Are Not Equally Associated with Abscess. Clin Infect Dis. 2001;32Issue(10):1511–1515. volume15: doi:10.1086/320163.
- Vogt RL, Dippold L. Escherichia Coli O157: h 7 Outbreak Associated with Consumption of Ground Beef, June-July 2002. Public Health Rep. 2005;120(2):174–178. doi:10.1177/003335490512000211.
- Lipatov KV, Asatryan A, Melkonyan G, et al. New classification for septic arthritis of the hand. World J Orthop. 2023;13(11):993–1005. doi:10.5312/wjo.v13.i11.993.
- Carlos GN, Kesler KA, Coleman JJ, et al. Aggressive surgical management of sternoclavicular joint infections. J Thorac Cardiovasc Surg. 1997;113(2):242–247. doi:10.1016/S0022-5223(97)70319-2.
- Murga A, Copeland H, Hargrove R, et al. Treatment for sternoclavicular joint infections: a multi-institutional study. J Thorac Dis. 2017;9(6):1503–1508. doi:10.21037/jtd.2017.05.76.
- Tone A, Nguyen S, Devemy F, et al. Six-week versus twelve-week antibiotic therapy for nonsurgically treated diabetic foot osteomyelitis: a multicenter open-label controlled randomized study. Diabetes Care. 2015;38(2):302–307. doi:10.2337/dc14-1514.
- Gorospe L, Ayala-Carbonero AM, Jover-Díaz R. Septic sternoclavicular arthritis complicated with bilateral pleural effusions. Asian Cardiovasc Thorac Ann. 2017;25(5):404–405. doi:10.1177/0218492316644082.
- Chen WS, Wan YL, Lui CC, et al. Extrapleural abscess secondary to infection of the sternoclavicular joint. Report of two cases. J Bone Joint Surg Am. 1993;75(12):1835–1839. doi:10.2106/00004623-199312000-00015.
- Dajer-Fadel WL, Ibarra-Pérez C, Borrego-Borrego R, et al. Descending necrotizing mediastinitis and sternoclavicular joint osteomyelitis. Asian Cardiovasc Thorac Ann. 2013;21(5):618–620. doi:10.1177/0218492312463570.