ABSTRACT
Hospital and community-acquired infections are escalating and pose significant public health unhealthiness worldwide. The advancements of telemedicine and automation of healthcare records are supported by cellphones, laptops and wearable devices. This study focused on the incidence of healthcare workers’ mobile phones becoming contaminated with pathogenic bacteria and their possible roles as vehicles of transmission of antimicrobial-resistant bacteria. A case study at two referral hospitals in Uganda between May and October 2020. Self-administered questionnaires were administered to participants after informed consent. Mobile phones of the participants in different departments of the hospitals were swabbed and samples were collected and transported to the microbiology laboratory for bacterial culture and antimicrobial susceptibility tests. The point prevalence of Healthcare workers’ mobile phone bacterial contamination with one or more species was 93%. Organisms isolated were E. coli 5.6% (1), Micrococcus spp 11.1% (2), Coagulase-negative staphylococci, CoNS, 61.1% (11) and Bacillus spp 22.2% (4). About 45% of the organisms were multidrug-resistant. Resistance was major to penicillin, cotrimoxazole, ciprofloxacin and Gentamicin, respectively. The isolated E. coli was resistant to all antibiotics used in the study. Only 15% (2) of the participants disinfected their phones at least once a week and 8% cleaned their hands after using a mobile phone. Healthcare Workers’ mobile phones can act as fomites for the transmission of multidrug-resistant microorganisms. This study provides strong evidence for developing and strengthening disinfection protocols for mobile phones and does not underscore the importance of hand hygiene in the middle of a patient encounter especially when the HCW grabs a phone but doesn’t re-clean their hands before patient contact.
Abbreviations: MDR, Multidrug-resistant; WHO, World Health Organization; IPC, infection prevention and control; HHC, hand hygiene compliance; JMEDICC, Joint Mobile Emerging Disease Intervention Clinical Capability
Introduction
High incidence of hospital-acquired infections tremendously increases the mortality and morbidity of patients especially in immunosuppressed populations including paediatrics, pregnant women, surgical patients and people with chronic illnesses like HIV/AIDS. (Carcillo et al., Citation2016)
Microorganisms, especially bacteria, are often found almost everywhere like; within the air, water, soil, food, and plants and animals, including humans. It’s greatly observed that inanimate objects also can carry microorganisms originating from the encircling environment. To be specific, Gram-positive cocci (Staphylococcus spp., Micrococcus spp.), but also spore-forming rods (Bacillus spp.) or Gram-negative bacteria, is transmitted through devices like mobile phones or computer keyboards (Selim & Abaza, Citation2015).
Mobile phones became indispensable accessories for professionals and social life. Nevertheless, several kinds of research have shown the potential bacteria colonisation of mobile surfaces and their ability to transmit diseases(Tagoe et al., Citation2011).
With the emergence of telemedicine, the utilisation of cell phones often occurs in hospitals by health care workers, and this can be one environment where hospital-associated (nosocomial) infections are most predominant (Akinyemi et al., Citation2009).
Unlike our hands which are easily disinfected using alcohol-based hand rubs (ABHR) that are made available readily across all hospitals and medical facilities, our mobile phones are quite tricky to scrub or disinfect and this is often evident as few healthcare workers perform decontamination of those devices (Aftab et al., Citation2015).
The role of fomites within the transmission of infectious diseases in healthcare institutions was extensively investigated and mobile phones were more problematic compared to other fomites especially when handling phones during patient care procedures, HCWs could easily transmit microorganisms from patients to their mobile phones and vice versa (Kotris et al., Citation2017).
In Uganda, bacterial infections alone were accountable for 26% of all admissions, 23% of all mortalities and 20% of all deaths in children under the age of 5 in 2018 (Ssekitoleko et al., Citation2020).
The spread of nosocomial infections is worsened by the emergence of antimicrobial-resistant strains of bacterial organisms which significantly increase the mortality and morbidity of bacterial infections furthermore because of the cost of healthcare (Fiore et al., Citation2017).
A reasonable gap between the knowledge about fomites acting as vectors within the spread of nosocomial infections and practices done to reduce this spread is critical. Having adequate knowledge is ineffectual until and unless its translated into the correct application of infection control practices (Aftab et al., Citation2016). Preventing the spread of nosocomial infections across patients and medical examiners are therefore of paramount importance towards reducing morbidity and mortality in resource-limited countries. Little research has been done to analyse the role of mobile phones in the spread of multidrug resistant (MDR) organisms and nosocomial infections, especially in Uganda. The aim of this study, therefore, was to spot bacteria on mobile phones, associated factors and susceptibility patterns to grasp the role of mobile phones as drivers of MDR and hospital-acquired infections in health facilities in Uganda.
Method
Study area
This study was conducted at two hospitals in Uganda, Kabarole Regional Referral Hospital found in western Uganda which is a referral hospital for Kamwenge, Kabarole, Kyegegwa, Ntoroko, Bundibugyo, Kitagwenda and Kyegegwa districts, with a 333-bed capacity. Mulago National Referral Hospital is a component of Mulago Hospital Complex, the teaching facility of Makerere University College of Health Sciences found in Kampala the capital of Uganda, and it has a 1000 bed capacity.
Study design and period
A case study was conducted at two regional referral hospitals between May and October 2020.
Study population
Healthcare workers who had used mobile phones for 3 months or more and consented to participate in the study.
Sampling
A total of 13 mobile phones were conveniently sampled from healthcare workers who verbally consented to participate in the study. A questionnaire was completed by a participant that had parameters like; the situation (Hospital department), usage time of mobile phones, smartphone or non-smartphone, smartphones methods of disinfection and material used if any, the quantity from the last cleaning of the mobile phones, awareness that cell phones can function as a source or drivers of infection, washing hands before and after using the phones and using the phone when during a toilet. Upon completion of the questionnaire, mobile phones were aseptically swabbed on the screen, keypads employing a moistened sterile swab and coded as the individuals’ questionnaire.
Sample processing
Samples collected from Kabarole Hospital were transported and analysed at the JMEDICC Laboratory within the hospital. Those collected from Mulago Hospital were analysed at the school of Health Sciences Clinical Microbiology Laboratory of Makerere University. All samples were transported to the laboratories within 12 hours after collection and plated immediately.
Sample inoculation
The cotton end of the swab with the sample was soaked in 10 ml peptone water and incubated aerobically at 37°C for 24 hours.
Isolation of organisms
We performed pure plating where pure isolated colonies were sub-cultured onto agar plates to grow fastidious organisms and to differentiate bacteria that supported their haemolytic properties. MacConkey agar plates were also want to isolate lactose fermenters.
Identification of organisms
From the pure colonies, gram staining was performed to differentiate gram reactions. The biochemical tests to include catalase, Indole, Citrate, Oxidase, Urease and urease and coagulase were performed.
Antibiotic Susceptibility Tests (AST)
Antibiotic susceptibility tests were performed on the Mueller–Hinton agar using the Kirby-Bauer disc diffusion technique. Four antibiotic discs cherish the drugs most typically utilised in Uganda for treatment of bacterial infections: Penicillin (P) 10 µg, Gentamicin (CN) 10 µg, Ciprofloxacin (CIP) 5 µg and Cotrimoxazole (Cxt) 25 µg. We measured zone diameters on plain Mueller–Hinton agar with a ruler for sensitivity as in (Performance, Citation2016).
Table 1. Shows an interpretation of zone diameters on Mueller–Hinton agar
Quality assurance and quality control
To avoid cross-contamination, the researcher wore a replacement pair of sterile new gloves when sampling each mobile phone after hand rubbing with locally produced alcohol-based hand sanitiser (ABHS) since its been proven to have a high antimicrobial effect (Fred et al., Citation2020; Kratzel et al., Citation2020). Standard operating procedures were followed at each step including the use of American Type Culture Colonies (ATCC) that were compared with the pure colonies isolated.
Results
Healthcare worker demographics
We screened 13 mobile phones owned by 13 healthcare workers (4 Laboratory Technicians, 2 clinicians, 5 Nurses and 2 midwives) as presented in the supplementary material. Of the 13 phones, 2 were non-smartphone, whereas 11 were smartphones as indicated in .
Figure 1. Healthcare workers categorised by cadre (a) and contamination of mobile phones classified as smartphones and non-smartphone.
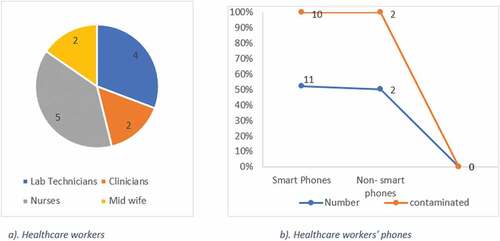
In principle, all the 13 healthcare workers were interviewed and 54% (n = 7) of these had knowledge on mobile phones acting as reservoirs for microorganisms, and from our analysis, only 15% (n = 2) of the participants disinfected their phones at least once a week, 8% (n = 1) cleaned their hands after using a mobile phone. Captivatingly, 31% (n = 4) of the participants used the phones with gloved hands and 31% (n = 4) used the phones while in a toilet as shown in .
Table 2. Associated Factors to bacterial contamination of Healthcare worker’s mobile phones, n represents the total number of participants
Results suggest that the majority of the healthcare workers do not routinely disinfect their phones and also miss the opportunity of hand hygiene after using their phones in the middle of a patient encounter.
Bacterial isolates and susceptibility testing
In total, 13 swabs from 13 mobile phones of healthcare workers were collected and analysed. In this way,100% (n = 2) of the None smartphones and 90.9% (n = 11) of the smartphones were contaminated with one or more species of bacteria, . A total of 18 isolates were obtained with overall bacterial contamination registered at 92.3% (n = 12). unveils organisms isolated as; E. coli 5.6% (Carcillo et al., Citation2016), Micrococcus spp 11.1% (Selim & Abaza, Citation2015), Coagulase-negative staphylococci, CoNS, 61.1% (Fred et al., Citation2020) and Bacillus spp 22.2% (Akinyemi et al., Citation2009). About 90% (n = 10) of the CoNS isolates were resistant to Penicillin, 80% (n = 9) resistant to cotrimoxazole, 60% (n = 6) resistant to ciprofloxacin and all susceptible to Gentamicin.
Figure 2. Bacterial isolates and resistance patterns to four commonly used antibiotics in healthcare facilities in Uganda.
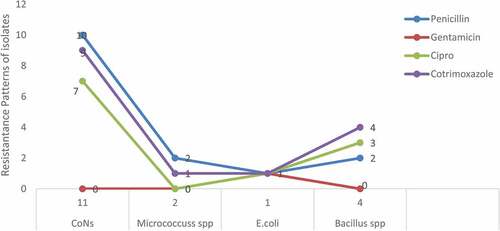
In the present case study, about 46% of the isolated organisms were multidrug-resistant, highest resistance registered with penicillin, cotrimoxazole, ciprofloxacin and Gentamicin, respectively. E. coli was resistant to all the antibiotics used in the study as indicated in and supplementary material.
Discussion
From this current study, the overall point prevalence of bacterial contamination of Healthcare workers’ mobile phones with one or more species was at 93%. Organisms isolated were majorly Coagulase Negative Staphylococcus Aureus (CoNS) in both hospitals, despite this being a skin normal flora it could be exogenously from surgical staff and can cause neonatal sepsis and also be able to transfer resistant genes to coagulase-positive staphylococcus aureus using horizontal gene transfer mechanism (Marchant et al., Citation2013; May et al., Citation2014). Other organisms were Bacillus spp., Micrococcus spp., which are predominantly associated with dusty environments habitual with Sub-Saharan Africa mainly rural and semi-urban settings (Matinyi et al., Citation2018) and E. coli which is suggestive of faecal contamination. Our study is of great public health importance with a perspective of faecal contamination and HAI transmission respectively. E. coli has been found to complicate wound sepsis resulting in poor patient prognosis (Moremi et al., Citation2017), agreeing with a study by Jana Koscova et al who majorly isolated skin coagulase-negative staphylococci aureus, species of the genus Bacillus and E.coli.
From this study, no conclusive factor was found to be associated with bacterial contamination of the Healthcare workers phones we however took into consideration the following hypotheses as factors associated with bacterial contamination, a smaller number of the HCW knew about mobile phones acting as reservoirs for micro-organisms, only two of the participants disinfected their phones at least once a week, some HCW used the phones with gloved hands and some used the phones while in a toilet similar findings by Ulger et al. indicate differences in personal hygiene and behaviours and failure of disinfecting the phones after contact as contributing factors to contamination (Ulger et al., Citation2015).
This study further revealed that about 46% of the isolated organisms were multidrug-resistant, highest resistance registered with penicillin, cotrimoxazole, ciprofloxacin and Gentamicin, respectively. E. coli was resistant to all the antibiotics used in the study and this can be explained by the intrinsic resistance of E. coli by way of possessing cascades that guard cell membrane permeability as well as producing Amp C B-lactamases (Davin-Regli & Pagã¨s, Citation2015). Coagulase Negative Staphylococcus Aureus (CoNS) is considered a normal flora; however, its drug resistance in this study is suggestive of being acquired exogenously from the hospital environment (Matinyi et al., Citation2018).
Even when the study registers a lot of strengths, we still had limitations as the study sample size was small due to lack of funding and this could also have been the reason for the lack of statistical significance of conclusive factors associated with bacterial contamination of HCW mobile phones. Bacteria quantification was not performed since the laboratories never had bacteria quantification capacity at the time of the study and in this way the study did not quantify the isolates from each mobile phone.
Conclusion
Healthcare Workers’ mobile phones can act as fomites for the transmission of multidrug-resistant microorganisms. This paper is particularly relevant because both the data-gathering and sample analysis took place during the COVID-19 pandemic, where the protocols were meant to be rigorous. Advancements in telemedicine and automated healthcare have not been matched by advancements in sanitising and decontaminating protocols for phones and other mobile devices; this is a time bomb of microbial transmission. This study provides strong evidence for developing and strengthening disinfection protocols for mobile phones and not underscore the importance of hand hygiene in the middle of a patient encounter especially when the HCW grabs a phone but doesn’t re-clean his/her hands before patient contact.
Consent for publication
All authors have read and agreed to publish the finding.
Contributors
Kibombo Daniela, Kusiima Brendaha and Luggya Tonnyb
a The Joint Mobile Emerging Disease Clinical Capability (JMEDICC) laboratory, Fort Portal Regional Hospital.
bMakerere University Microbiology Laboratory. All contributors provided support during sample collection and analysis.
Definition of Terms
Disinfection; the process of cleaning an inanimate object especially with a chemical/detergent, to destroy microorganisms.
Smart Phone: is a portable device that combines telephone and computing functions into one unit with an extensive mobile operating system like a mini-computer which facilitates wider software, internet and multimedia function capabilities alongside core phone functions such as voice calls and text messaging.
Non-smart Phone: is a phone that does not have an operating system, computing capabilities, GPRS, syncing capabilities, video conferencing or a basic or a feature phone. A basic phone is any phone that allows the user basic features such as sending/receive calls and texts.
Ethics approval and consent to participate
This study was a sub-study of the National IPC survey, and participants provided informed consent before participation.
Supplemental Material
Download MS Word (15.1 KB)Availability of data and material
Technical appendix, statistical appendix, and dataset will be available upon formal request.
Supplementary material
Supplemental data for this article can be accessed here.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aftab, H.B., Zia, B., Zahid, M.F., Raheem, A., & Beg, M.A. (2016). Knowledge, attitude, and practices of healthcare personnel regarding the transmission of pathogens via fomites at a tertiary care hospital in Karachi (pp. ofv208). In Oxford University Press.
- Aftab, H.B., Zia, B., Zahid, M.F., Raheem, A., & Beg, M.A.K. (2015, December). Attitude, and Practices of Healthcare Personnel Regarding the Transmission of Pathogens via Fomites at a Tertiary Care Hospital in Karachi, Pakistan. Open Forum Infectious Diseases, 3(1), ofv208–ofv208. https://doi.org/10.1093/ofid/ofv208
- Akinyemi, K., Atapu, A., Adetona, O., & Coker, A. (2009, September). The potential role of mobile phones in the spread of bacterial infections. Journal of Infection in Developing Countries, 3(8), 628–632. https://doi.org/10.3855/jidc.556
- Carcillo, J.A., Dean, J.M., Holubkov, R., Berger, J., Meert, K.L., Anand, K.J., et al. (2016). Inherent Risk Factors for Nosocomial Infection in the Long Stay Critically Ill Child Without Known Baseline Immunocompromise: A Post–Hoc Analysis of the CRISIS Trial. The Pediatric Infectious Disease Journal, 35(11), 1182. https://doi.org/10.1097/INF.0000000000001286
- Davin-Regli, A., & Pagã¨s, J.-M. (2015). Enterobacter aerogenes and Enterobacter cloacae; versatile bacterial pathogens confronting antibiotic treatment. Frontiers in Microbiology, 6, 392. https://doi.org/10.3389/fmicb.2015.00392
- Fiore, M., Maraolo, A.E., Gentile, I., Borgia, G., Leone, S., Sansone, P., Passavanti, M.B., Aurilio, C., & Pace, M.C. (2017). Nosocomial spontaneous bacterial peritonitis antibiotic treatment in the era of multi-drug resistance pathogens: A systematic review. World Journal of Gastroenterology: WJG, 23(25), 4654. https://doi.org/10.3748/wjg.v23.i25.4654
- Fred, T., Sophia, K., Alex, S., Emmanuel, B., Tom, L., & Lucas, A. (2020). Comparison of Antibacterial Efficacy of Locally Produced Alcohol Based Hand Sanitizer and Commonly Available Commercial Hand Sanitizer Used in Healthcare Facilities in Uganda. Open Access Library Journal, 7(4), 1–13.
- Kotris, I., Drenjančević, D., Talapko, J., & Bukovski, S. (2017, February 1). Identification of microorganisms on mobile phones of intensive care unit health care workers and medical students in the tertiary hospital. Medicinski Glasnik off Publication Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina, 14(1), 85–90.
- Kratzel, A., Todt, D., V’kovski, P., Steiner, S., Gultom, M., Thi Nhu Thao, T., Ebert, N., Holwerda, M., Steinmann, J., Niemeyer, D., Dijkman, R., Kampf, G., Drosten, C., Steinmann, E., Thiel, V., & Pfaender, S. (2020). Inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 by WHO-Recommended Hand Rub Formulations and Alcohols. Emerging Infectious Diseases Journal Internet, 26(7), 1592–1595. https://wwwnc.cdc.gov/eid/article/26/7/20-0915_article
- Marchant, E.A., Boyce, G.K., Sadarangani, M., & Lavoie, P.M. (2013). Neonatal sepsis due to coagulase-negative staphylococci. Clinical & Developmental Immunology, 2013.
- Matinyi, S., Enoch, M., Akia, D., Byaruhanga, V., Masereka, E., Ekeu, I., & Atuheire, C. (2018). Contamination of microbial pathogens and their antimicrobial pattern in operating theatres of peri-urban eastern Uganda: A cross-sectional study. BMC Infectious Diseases, 18(1), 1–9. https://doi.org/10.1186/s12879-018-3374-4
- May, L., Klein, E.Y., Rothman, R.E., & Laxminarayan, R. (2014, March). Trends in Antibiotic Resistance in Coagulase-Negative Staphylococci in the United States, 1999 to 2012. Antimicrobial Agents and Chemotherapy, 58(3), 1404. https://doi.org/10.1128/AAC.01908-13
- Moremi, N., Claus, H., Vogel, U., & Mshana, S.E. (2017). Surveillance of surgical site infections by Pseudomonas aeruginosa and strain characterization in Tanzanian hospitals does not provide proof for a role of hospital water plumbing systems in transmission. Antimicrobial Resistance and Infection Control, 6(1), 1–8. https://doi.org/10.1186/s13756-017-0216-x
- Performance, C. (2016). Standards for Antimicrobial Susceptibility Testing. CLSI supplement M100S Wayne. PA Clinical and Laboratory Standards Institute.
- Selim, H.S., & Abaza, A.F. (2015, February 2). Microbial contamination of mobile phones in a health care setting in Alexandria, Egypt. GMS Hygiene and Infection Control, 10, Doc03–Doc03. https://doi.org/10.3205/dgkh000246
- Ssekitoleko, R.T., Oshabaheebwa, S., Munabi, I.G., Tusabe, M.S., Namayega, C., Ngabirano, B.A., Matovu, B., Mugaga, J., Reichert, W.M., & Joloba, M.L. (2020, Oct). The role of medical equipment in the spread of nosocomial infections: A cross-sectional study in four tertiary public health facilities in Uganda. BMC Public Health, 20(1), 1561. https://doi.org/10.1186/s12889-020-09662-w
- Tagoe, D.N., Gyande, V.K., & Ansah, E.O. (2011).Bacterial contamination of mobile phones: When your mobile phone could transmit more than just a call.
- Ulger, F., Dilek, A., Esen, S., Sunbul, M., & Leblebicioglu, H. (2015). Are healthcare workers’ mobile phones a potential source of nosocomial infections? Review of the literature. Journal of Infection in Developing Countries, 9(10), 1046–1053. https://doi.org/10.3855/jidc.6104
