Abstract
Background: Dynamic postural instability is a common neuromuscular impairment in cerebral palsy (CP), which often includes balance dysfunction and an associated risk of serious falls. Robotic hippotherapy has recently become a widespread clinical application to facilitate postural core stabilization, strength, and endurance through repetitive vestibular and proprioceptive stimulation to the spine via the sensorimotor system pathways. However, the long-term effects of robotic hippotherapy on dynamic postural instability in CP remain unclear.
Objective: To examine the long-term effects of robotic hippotherapy on dynamic postural stability in CP.
Methods: An advanced three-dimensional biomechanical eight-camera video motion capture (VMC) system was used to compute the center of mass (COM) pathway, which represents intervention-related spinal core instability. The robotic hippotherapy system was used to improve dynamic postural stability and associated balance performance. Robotic hippotherapy exercise was provided for 45 minutes/session, 2–3 times a week over the 12-week period.
Results: Abnormal mean COM pathway length, standard deviation, and range substantially decreased after 12 weeks of robotic hippotherapy. The initial x-axis COM was greater than that of the y-axis. However, the amount of abnormal anterior–posterior and medio-lateral postural sway substantially decreased after robotic hippotherapy.
Conclusions: This study provides the first compelling evidence that the robotic hippotherapy is safe and effective for postural instability control and sitting balance dysfunction that mitigates the risk of falls in CP.
1. Introduction
There is an accumulating body of evidence that corroborates the therapeutic efficacy of horseback riding for facilitating gross motor function in children with cerebral palsy (CP).[Citation1–4] Nevertheless, robotic hippotherapy has recently appeared as an alternative in clinical environments where real horses are not readily accessible or unaffordable.[Citation5] Limited accessibility to horses, weather-dependence, and cost may all contribute to the increased use of robotic horses.[Citation6] Although robotic hippotherapy does not allow patients to interact with a live horse, this therapy has the advantage of allowing regular therapy with no apparent spatiotemporal or weather constraints.[Citation7] Our robotic hippotherapy system is designed to facilitate stretching, rhythmic trunk rotation, core stabilization, strength, endurance, and cardiopulmonary function via the sensorimotor system (vestibular, proprioceptive).[Citation2,Citation6,Citation8–11] The system simulates live horse movements, including walking (6 km/h), trotting (15 km/h), cantering (25 km/h), and galloping (60 km/h). These movements are featured as exercise modes composed of 100 different two-dimensional movement patterns with 100 different exercise modes. Conceptually, robotic hippotherapy was developed based on the collective integration of the best clinical evidence [Citation2,Citation8,Citation9] and the fact that pediatric neurorehabilitation must be fun, motivating, intensive, task-specific, rhythmic, repetitive, and integrated, and should be implemented over a long period of time to produce measurable changes in muscle size,[Citation2,Citation6] motor behavior,[Citation10] and neuroplasticity.[Citation11] Intensive repetitive, rhythmic movement is a hallmark of horse movement, like human locomotion. An average horse cadence is reported to be 100 steps per minute at a preferred or medium walking speed,[Citation12] which can serve as a therapeutic perturbation and a challenge to postural stability, since the client needs to adaptively re-stabilize his or her perturbed equilibrium repeatedly. However, the long-term effects of robotic hippotherapy on dynamic postural instability in CP, which is conceptually defined as an inability to maintain the center of mass (COM) within the base of support (BOS) in response to external perturbation or movement, remain unclear.[Citation13,Citation14] Therefore, the purpose of this study was to examine the long-term effects of robotic hippotherapy on dynamic postural stability. We hypothesized that a long-term robotic hippotherapy intervention would improve dynamic postural stability and balance performance.
2. Materials and methods
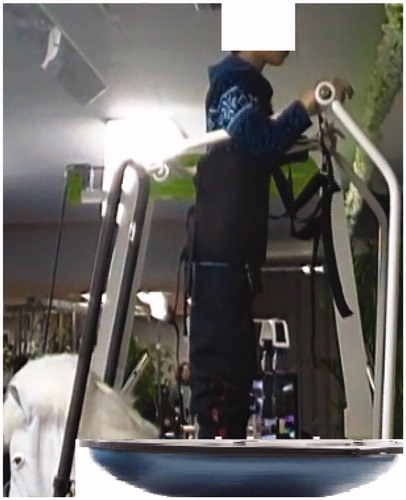
The study included a pre-test, a 12-week hippotherapy intervention, and a post-test. An 11-year-old child diagnosed with CP and associated core instability was the subject in this study. At the pre- and post-tests, intervention-related postural instability was estimated using the trajectories of the COM. The COM was measured using an eight-camera video motion capture (VMC) system using Cortex software, Version 1.0.0.198 (Motion Analysis Corporation, Santa Rosa, CA) and a 50-cm × 50-cm force plate (Kistler; Winterthur, Switzerland). To identify intervention-related changes in dynamic postural stability, 31 reflective markers (9 mm) were attached to anatomical landmarks on the child's head, trunk, and lower extremities to track kinematic motion. As illustrated in , a three-dimensional figure was created in the visual motion capture (VMC) software using reflective surface markers placed on anatomical landmarks. This VMC system was set to record at a sampling rate of 60 Hz with an accuracy of 0.5 mm. A force plate was also used to record ground reaction forces at 300 Hz and was later synchronized to compute the COM. The child was positioned on a customized, motorized barrel in the motion capture volume. The motorized barrel moved reciprocally in an anterioposterior direction at three speeds: 0.5, 0.6, and 0.7 Hz.
Figure 1. Three-dimensional figure created in visual motion capture (VMC) software using reflective surface markers on anatomical landmarks.
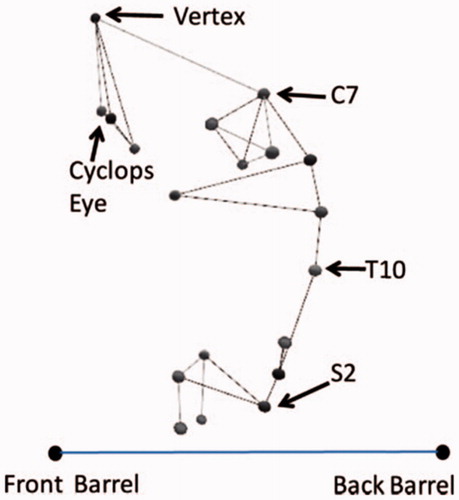
Data analysis for the COM measurement was implemented by synchronizing the kinematic data and kinetic data. Kinematic data obtained from surface marker tracking were edited using Cortex software to configure three-dimensional coordinates for each trial. Data recorded for the second half (7.5 s) of each 15-s trial were processed for further analysis, which represented relatively consistent reciprocating movement of the customized, motorized barrel. The kinematic variables measured from these tracked data included head and trunk segment kinematics angles during motorized barrel perturbation. The head segment kinematic angle was determined by computing the intersection angle between the line segments of the vertex marker and the C7 marker, and the horizontal line segment between the front and the back barrel markers. The trunk segment kinematic angle was determined by the intersection angle between the line segment of the C7 marker and the L5 marker, and the horizontal line of the barrel markers. More detailed information has been described previously.[Citation8]
The robotic hippotherapy system (FORTIS-102, Daewon Fortis, Ha Nam, Kyungi, Korea) was used to improve dynamic postural stability. Robotic hippotherapy exercise was administered by experienced therapists 2–3 times a week over the 12-week period. Each interventional session lasted 45 minutes and included sitting in various positions on a moving robotic horse that walked and/or trotted (e.g., forward astride, side sit, tall kneel, reverse astride, and quadruped). The therapy involved several transitions between positions, some of which occurred while the horse was moving.[Citation9] As described in the manufacturer's guidelines (), therapy involving the device includes 12 visits to the lab. The robotic horse movement level was set at course #100 with a slow speed or in a comfortable walking mode (levels 1–50), which imitates rhythmic horse movement designed for core stabilization; trunk rotation in forward astride position, side-sitting, backward astride, and tall kneel; and improved postural and locomotor movement complexity in all directions.[Citation6]
3. Results
The mean COM pathway length, standard deviation, and range decreased from pre-robotic hippotherapy to post-robotic hippotherapy (). Specifically, the initial X-axis COM was greater than that of the Y-axis. However, the amount of abnormal anterior–posterior and medio-lateral postural sway decreased as a result of the intervention.
Table 1. Static stability variables.
4. Discussion
The present investigation highlighted the long-term effects of robotic hippotherapy on dynamic postural stability in a child with CP. As anticipated, after 12 weeks of robotic hippotherapy, our biomechanical analysis results demonstrated that both X- and Y-axis COM pathway lengths decreased in anterior–posterior and medio-lateral spinal core instability during a motorized barrel perturbation. This finding supports hippotherapy's effectiveness for improving postural stability during dynamic movement using objective quantification of spinal core stability in a child with CP.[Citation6,Citation8,Citation9,Citation15] These objective improvements in dynamic postural stability were correlated to functional movement performance, specifically dynamic sitting and standing balance, after the intervention. As a result of the therapy, the child was more stable and upright while sitting and standing. Prior to the intervention, the child demonstrated greater postural sway, as evidenced by the COM pathway length measurement. This leads to postural instability, poor balance, and a higher risk of falling.[Citation16] The child's parent reported that the child occasionally fell prior to the intervention. These falling episodes were associated with poor postural stability. The therapy allowed the child to be more confident while walking, jumping, and running. In addition, there was a significant reduction in apparent abnormal postural sway and staggering locomotor behavior ().
The underlying neurophysiological rationale for such improvements in postural core stability and balance performance may result from the integrative and repetitive vestibular and proprioceptive sensorimotor stimuli provided during robotic hippotherapy. Robotic hippotherapy may have facilitated upright posture, anticipatory postural adjustment control, equilibrium reaction, stretching of shortened hip abductors and strengthening of the lumbopelvic musculature. Such neurophysiological outcomes were reflected in improved postural alignment, symmetry, and muscle size and strength in trunk muscles as a result of the robotic hippotherapy.[Citation6] These findings are also represented by our data regarding COM postural stability measurements. In the present study, the typical robotic hippotherapy session lasted 45 minutes and the total sensorimotor stimulations included as many as 3000–5000 repetitions of postural control challenge. This exceeded the required number of repetitions that are typically offered in conventional neurorehabilitation or may be equivalent to the hippotherapy.[Citation5,Citation6] Lang et al. [Citation17] demonstrated that the number of repetitions in customary neurorehabilitation (physical and occupational therapy) care sessions included 6.0 and 291.5 repetitions per session for balance and gait (steps), particularly in stroke rehabilitation. However, previous experimental studies showed that as many as 400–600 repetitions are needed to produce neuroplasticity and associated motor recovery after ischemic lesions.[Citation11,Citation18] In this context, innovative robotic hippotherapy and virtual reality systems should be considered as an alternative movement therapy to provide interactive and motivating virtual reality exercises with a greater number of repetitions (Lang). In fact, Lee et al. [Citation6] reported that robotic hippotherapy can provide rhythmic two-dimensional postural control and lumbopelvic core stabilization exercise with large numbers of repetitions (3000–5000 per each session), which surpasses conventional neurorehabilitation and potential requirements for neuroplasticity and may allow functional motor recovery to occur. Recent robotic hippotherapy studies [Citation5] demonstrated that robotic hippotherapy was capable of therapeutic stimulation with safe, repetitive, and variable modes of movement perturbation. Park et al. [Citation5] showed that the robotic hippotherapy acceleration was approximately five times less than that of real horse movement (0.67 m/s2 vs. 3.22 m/s2, respectively). This suggests the issue of patient safety when performing hippotherapy exercises with a real horse, especially for patients who exhibit inherently unstable postural control if not carefully screened.
Undoubtedly, the four-legged robotic horse system provides 6 degrees of freedom (DOF), which mimics real horse movement; this can be useful for training novice ‘healthy’ riders, but can be dangerous for people with postural control dysfunction, because of a higher risk of falls.[Citation12,Citation13] Moreover, as documented previously,[Citation5] greater acceleration movement was observed with real horse hippotherapy because it involves multiple DOFs just like the four-legged robotic horse, which render a great challenge for children with moderate or severe CP. Hence, in a real hippotherapy situation, two-side walkers including a therapist usually work together to ensure patient safety. In robotic hippotherapy, there is a greater liberty to progress and adjust the robotic horse movement from slow amplitudes to large, fast movement amplitudes. This enables a therapist to accommodate patients with moderate and severe postural control dysfunction, and then build up the challenge in fine increments as they progress in their postural core stability, endurance, strength, and coordination. Such postural core improvements will not only reduce the risk of falls in children with CP, but also help to address the common neuromuscular impairments in CP such as scoliosis, lordosis, and kyphosis; this is because previous evidence has demonstrated decreased deep core muscle size such as transversus abdominis muscle in adolescent scoliosis.[Citation6,Citation19,Citation20] Taken together, these results provide therapeutic evidence that robotic hippotherapy can be used as an alternative therapy in the management of CP patients with core instability. Nevertheless, further clinical trials are needed to generalize our findings. The objective quantification of these outcome measures using advanced motion analysis systems can provide important clinical evidence regarding the results of robotic hippotherapy. Such data will further inform clinicians and third-party supporters about the benefits of robotic hippotherapy.
5. Conclusion
Robotic hippotherapy is an effective method of enhancing dynamic postural stability in CP patients with postural instability, poor balance, and a high fall risk. In this study, a long-term robotic hippotherapy intervention decreased COM anterior–posterior and medio-lateral sway. These data suggest that robotic hippotherapy improves spinal core stability and balance.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
This study was funded by Daewon Fortis, Ha Nam, Kyungi, Korea, and in part by “Brain Korea 21 PLUS Project (Grant No. 2016-51-0009)” sponsored by the Korean Research Foundation for Department of Physical Therapy in Graduate School, Yonsei University.
References
- Casady RL, Nichols-Larsen DS. The effect of hippotherapy on ten children with cerebral palsy. Pediatr Phys Ther. 2004;16:165–172.
- You SH, Jang SH, Kin YH, et al. Virtual reality-induced cortical reorganization and associated locomotor recovery in chronic stroke: an experimenter-blind randomized study. Stroke. 2005;36:1166–1171.
- Frank A, McCloskey S, Dole RL. Effect of hippotherapy on perceived self-competence and participation in a child with cerebral palsy. Pediatr Phys Ther. 2011;23:301–308.
- Zadnikar M, Kastrin A. Effects of hippotherapy and therapeutic horseback riding on postural control or balance in children with cerebral palsy: a meta‐analysis. Dev Med Child Neurol. 2011;53:684–691.
- Park JH, Shurtleff T, Engsberg J, et al. Comparison between the robo-horse and real horse movements for hippotherapy. Biomed Mater Eng. 2014;24:2603–2610.
- Lee DR, Lee NG, Cha HJ, et al. The effect of robo-horseback riding therapy on spinal alignment and associated muscle size in MRI for a child with neuromuscular scoliosis: an experimenter-blind study. NeuroRehabilitation. 2011;29:23–27.
- Zurek G, Dudek K, Pirogowicz I, et al. Influence of mechanical hippotherapy on skin temperature responses in lower limbs in children with cerebral palsy. J Physiol Pharmacol. 2008;59:819–824.
- Shurtleff TL, Engsberg JR. Changes in trunk and head stability in children with cerebral palsy after hippotherapy: a pilot study. Phys Occup Ther Pediatr. 2010;30:150–163.
- Shurtleff TL, Standeven JW, Engsberg JR. Changes in dynamic trunk/head stability and functional reach after hippotherapy. Arch Phys Med Rehabil. 2009;90:1185–1195.
- Han JY, Kim JM, Kim SK, et al. Therapeutic effects of mechanical horseback riding on gait and balance ability in stroke patients. Ann Rehabil Med. 2012;36:762–769.
- Nudo RJ, Wise BM, SiFuentes F, et al. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science. 1996;272:1791–1794.
- Clayton HM, Walk this way. USDF Connection; 2002. p. 39–42.
- Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989;70:510–517.
- Pai YC, Patton J. Center of mass velocity-position predictions for balance control. J Biomech. 1997;30:347–354.
- Shurtleff T, Engsberg J. Long-term effects of hippotherapy on one child with cerebral palsy: a research case study. Br J Occup Ther. 2012;75:359–366.
- Hasson CJ, Van Emmerik RE, Caldwell GE, et al. Predicting dynamic postural instability using center of mass time-to-contact information. J Biomech. 2008;41:2121–2129.
- Lang CE, MacDonald JR, Gnip C. Counting repetitions: an observational study of outpatient therapy for people with hemiparesis post-stroke. J Neurol Phys Ther. 2007;31:3–10.
- Kleim JA, Barbay S, Nudo RJ. Functional reorganization of the rat motor cortex following motor skill learning. J Neurophysiol. 1998;80:3321–3325.
- Linek P, Saulicz E, Kuszewski M, et al. Ultrasound assessment of the abdominal muscles at rest and during the ASLR test among adolescents with scoliosis. Clin Spine Surg. 2016. [Epub ahead of print]. doi: 10.1097/BSD.0000000000000055.
- Linek P, Saulicz E, Wolny T, et al. Ultrasound evaluation of the symmetry of abdominal muscles in mild adolescent idiopathic scoliosis. J Phys Ther Sci. 2015;27:465.