Abstract
Background: Both minimally invasive surgery (MIS) and computer-assisted surgery (CAS) in total knee arthroplasty have been scientifically linked with surgical benefits. However, the long-term results of these techniques are still controversial. Most surgeons assessed the surgical outcomes with regard to knee alignment and range of motion, but these factors may not reflect subjective variables, namely patient satisfaction.
Purpose: To compare satisfaction and functional outcomes between two technical procedures in MIS total knee arthroplasty, namely computer-assisted MIS and conventional MIS procedure, operated on a sample group of patients after 10 years.
Methods: Seventy cases of posterior-stabilized total knee prostheses were implanted using a computer-assisted system and were compared to 74 cases of matched total knee prostheses of the same implant using conventional technique. Both groups underwent arthrotomy by 2 cm limited quadriceps exposure minimally invasive surgery (2 cm Quad MIS). At an average of 10 years after surgery, self-administered patient satisfaction and WOMAC scales were administered and analyzed.
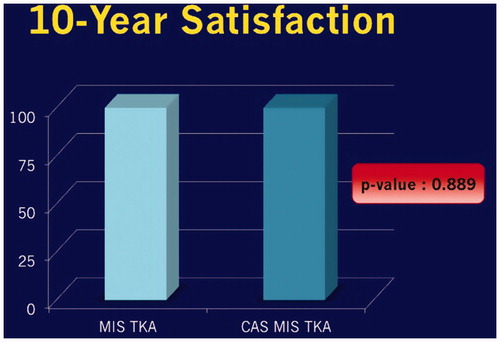
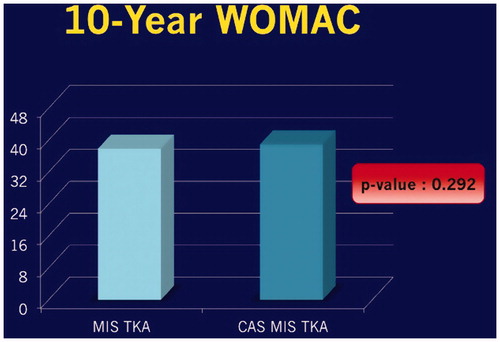
Results: Demographic data of both groups including sex, age, preoperative WOMAC and post-operative duration were not statistically different. Post-operative WOMAC for the computer-assisted group was 38.94 ± 5.68, while the conventional one stood at 37.89 ± 6.22. The median of self-administered patient satisfaction scales of the computer-assisted group was 100 (min37.5–max100), while the conventional one was 100 (min25–max100). p Value was 0.889. There was one re-operative case in the conventional MIS group due to peri-prosthetic infection which was treated with debridement, polyethylene exchanged and intravenous antibiotics.
Conclusions: The 10-year outcomes of computer-assisted MIS total knee arthroplasty are not superior to that of the conventional MIS technique in function and patient satisfaction. 10 years may not be enough to show the difference between these two techniques.
Introduction
Although minimal invasive surgery (MIS) in total knee arthroplasty has many advantages over conventional techniques, such as decreased blood loss, shorter hospital stay and increased range of motion,[Citation1] this technique is often associated with a number of complications including patella tendon injury, lateral femoral condyle fracture and varus tibia.[Citation2] Alignment errors of more than 3° have a strong correlation with early operational failure and less satisfactory functional results.[Citation3,Citation4] Use of computer-assisted surgery (CAS) in total knee arthroplasty improves mechanical alignment, frontal and sagittal femoral axis and frontal tibial axis.[Citation5] However, the long-term result of CAS in MIS total knee arthroplasty is still controversial. Most surgeons assess the surgical outcomes with regard to knee alignment and knee range of motion, but these factors may not reflect the subjective variables, namely patient satisfaction. This paper studies the long-term satisfaction of CAS in MIS total knee arthroplasty.
Objective
The primary objective of this study was to compare patient satisfaction and functional outcome between computer-assisted surgery (CAS) and conventional procedure, both in minimally invasive surgery (MIS) total knee arthroplasty, 10 years after the operation.
The secondary objective was to collect the revision case’s data.
Materials and methods
The research participants were patients diagnosed with osteoarthritis of the knee and treated with posterior-stabilized total knee arthroplasty in the orthopedic department at Phramongkutklao hospital in 2006 by an experienced surgeon. The navigation system that we used was Brainlab Ci CAS with Ci 1.0 imageless software. While using the same type of implant, Group1 was operated on using a computer-assisted system with free hand technique () while group2 by the conventional technique. Both groups underwent arthrotomy by 2 cm limited quadriceps exposure through minimally invasive surgery (2 cm Quad MIS).[Citation6,Citation7] Inclusion criteria were patients, aged between 60–90, with osteoarthritis of the knee who had failed to be cured by conservative treatments and were then treated with total knee arthroplasty in 2006 by the same experienced surgeon. Patients who could not understand or answer the questionnaire by himself/herself or loss to follow up were excluded from this study.
Figure 1. Tibial cutting guide was adjusted by free-hand technique correspond to the signal from navigator.

At an average of 10 years after surgery, we studied patient satisfaction and functions using the self-administered patient satisfaction scales.[Citation8] and the Thai version of Western Ontario and McMaster (WOMAC) osteoarthritis index for knee osteoarthritis.[Citation9,Citation10]
The satisfaction scale consists of four criteria focusing on the extent of pain relief, improvement in ability to perform home or yard work, ability to perform recreational activities and overall satisfaction with joint replacement. The Thai version of WOMAC scale was created and validated by Kuptniratsalkul V and Rattanachaiyanont M in 2005. 24-item original WOMAC index [Citation9] was translated into Thai, backtranslated, tested for face and content validities, and then modified to 22-item Thai WOMAC version. Since 2006, this version of Thai WOMAC scale has been widely used with author permission in Thailand for several research and studies. The process of submission and publication of this scale in Clinical rheumatology journal complete in 2007.[Citation10]
We collected demographic data and filled the questionnaire by telephone survey. Demographic data included sex, age, preoperative WOMAC scores and post-operative duration. Patients were classified into CAS MIS total knee arthroplasty and conventional MIS total knee arthroplasty. The data collected during the 10-year were analyzed by statisticians using SPSS of Windows version 20.0 to compare pre-operative and 10-year post-operative WOMAC scores; 10-year WOMAC score between CAS MIS; and conventional MIS and 10-year satisfaction scale between groups. The incidence of revision cases was recorded.
The sample size calculation was based on data from a previous study of N. Mahomed, Rajiv Gandhi, Lawrence Daltroy and J.N. Katz (2011). The authors revealed that the mean of satisfaction score was 2.84 (SD19). The calculated sample size was 40 subjects per group with a power of 80% and type I error of 5%. Statistical analyses were performed using SPSS of Windows version 20.0.
Demographic data were analyzed using Chi-Square test, Fisher’s exact test and independent t-test. The values of p < 0.05 were considered as statistically significant. Results of study were based on the 10-year post-operative WOMAC scores and 10-year satisfaction scale. This data were then analyzed in order to compare the pre-operative and 10-year post-operative WOMAC scores; and 10-year WOMAC score with CAS MIS and conventional MIS using independent t-test. Comparing 10-year satisfaction scale between groups using Mann–Whitney U test, at a p value of <0.05 is considered statistically significant for all analyzed data.
Results
There were 180 patients who were treated with total knee arthroplasty by the same surgeon in 2006. Among these, 15 patients were dead, 3 patients were unable to answer the questionnaire due to cerebrovascular disease and 18 patients were lost to the follow-up process. 20 patients were in conventional MIS group and 16 patients were in CAS MIS group. In addition, one patient was re-operated as a result of peri-prosthetic infection. 144 total knee arthroplasy patients were recruited and categorized into two groups, 74 in the conventional MIS group and 70 in the CAS MIS group.
The patients’ demographic data are summarized in . Mean age and post-operative duration were 76.73 years and 120.15 months, respectively, in the conventional MIS group; and 77.10 years and 120.57 months, respectively, in the CAS MIS group. Other demographic data were sex and age. Data from both groups were not significantly different.
Table 1. Demographic data of the population.
The 10-year WOMAC score was assessed and compared to baseline data before surgery, mean of the pre-operative WOMAC score in conventional MIS were 22.47; and 37.89 in 10-year follow up with p value < 0.01. In the CAS MIS group, mean in pre-operative was 22.51 and 10-year follow up was 38.94, p value < 0.01 was the same as conventional MIS.
Ten-year satisfaction was assessed by self-administered patient satisfaction scales, data in conventional MIS was 100(35.7–100), while in the CAS MIS group was 100(25–100), p value was .889 (). The data of 10-year WOMAC in the conventional MIS group was 37.89 and CAS MIS group was 38.94. p Value was .292 ().
One re-operative case suffered knee pain after one year of conventional MIS surgery. She got a peri-prosthetic infection and was treated with polyethylene exchange and intravenous antibiotics.
Discussion
Nowadays, the procedures for total knee arthroplasty have developed a lot and MIS is one of advanced techniques. Although MIS in total knee arthroplasty has many advantages over conventional techniques such as decreased blood loss, shorter hospital stay, and increased range of motion, this technique is often associated with a number of complications including patella tendon injury, lateral femoral condyle fracture, varus tibia and alignment errors more than 3° – all of which have a strong correlation with early operational failure and less satisfactory functional results. CAS has been developed to improve the accuracy of bone cutting and mechanical alignment including frontal, sagittal femoral axis and frontal tibial axis. The aim of CAS is to increase longevity of the implants and patient satisfaction, but the 10-year results from this study do not show a significant difference between CAS MIS and conventional MIS when it comes to patient satisfaction. This is possibly due to the fact that the conventional MIS with new model implants is already one of the best techniques capable of providing optimal results. Use of CAS in this type of surgery may neither increase the satisfaction nor produce better function, especially when it has failed to score a significantly better mark on patient’s 10-year satisfaction.
There was one revision case, which was the patient who had been treated for osteoarthritis of knee with the conventional MIS procedure. After one year of surgery, she picked up an infection and was treated with debridement, polyethylene exchange and intravenous antibiotics. There were no infected cases in the CAS MIS group, however, this might be due to the insufficient number of patients. Incidence of infection in this study was 0.63%.
The upside of this paper was the 10-year follow-up study and the use of CAS with the MIS procedure. Limitations of this study were that 15 patients (8.33%) had later died, 3 patients (1.67%) had cerebrovascular accidents and 18 patients (10.0%) were unable to answer the questionnaires due to medical conditions such as dementia, cerebral atrophy. For these reasons when the patients get older, they have more comorbidities that affect their functions. So, functional evaluation will be more difficult to do interpretation. WOMAC score is generally reliable score to assess pain, stiffness and physical function in patients with hip and/or knee osteoarthritis (OA) but not specific to post-total knee arthroplasty patients. This score may not be able to show the slight difference of post-operative patient functions and in elderly patients who are less active in daily living.
Conclusions
Computer-assisted total knee arthroplasty improve alignment of the knee but satisfaction and functional outcomes may not be differed. Our study from 10 years post-operation did not show statistically significant difference with the results. 10 years may not be enough to show the differences between these two techniques, the study should be conducted in more than 10 years post-operative patients for a better comparison between the techniques.
Disclosure statement
We declare that we have no conflict of interest.
References
- Tria AJ. Jr. Minimally invasive total knee arthroplasty: the importance of instrumentation. Orthop Clin North Am. 2004;35:227–234.
- Chen AF, Alan RK, Redziniak DE, Tria AJ Jr. Quadriceps sparing total knee replacement. The initial experience with results at two to four years. J Bone Joint Surg Br. 2006;88:1448–1453.
- Ecker ML, Lotke PA, Windsor RE, Cella JP. Long- term results after total condylar knee arthroplasty. Significance of radiolucent lines. Clin Orthop Relat Res. 1987;216:151–158.
- Feng EL, Stulberg SD, Wixson RL. Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop Relat Res. 1994;299:60–71.
- Bathis H, Perlick L, Tingart M, et al. Radiological results of image- based and non-image-based computer-assisted total knee arthroplasty. Int Orthop. 2004;28:87–90.
- Chotanaphuti T, Ongnamthip P, Teeraleekul K, Kraturerk C. Comparative study between computer assisted-navigation and conventional technique in minimally invasive surgery total knee arthroplasty, prospective control study. J Med Assoc Thai. 2008;91:1382–1388.
- Chotanaphuti T, Ongnamthip P, Karnchanalerk K, Udombuathong P. Comparative study between 2 cm limited quadriceps exposure minimal invasive surgery and conventional total knee arthroplasty in quadriceps function: prospective randomized controlled trial. J Med Assoc Thai. 2008;91:203–207.
- Mahomed N, Gandhi R, Daltroy L, Katz JN. The Self-Administered Patient Satisfaction Scale for primary hip and knee arthroplasty. Clin Orthop Relat Res. 2010;468:57–63.
- Bellamy N, Campbell J, Hill J, Band P. A comparative study of telephone versus onsite completion of the WOMAC 3.0 Osteoarthritis Index. J Rheumatol. 2002; 29:783–786.
- Kuptniratsalkul V, Rattanachaiyanont M. Validation of a modified Thai version of the Western Ontario and McMaster (WOMAC) osteoarthritis index for knee osteoarthritis. Clin Rheumatol. 2007;26:1641–1645.