Abstract
4-Dimensional hysterosalpingo-contrast sonography (4 D HyCoSy) using SonoVue is regarded as a really good option available for evaluating fallopian tubal patency. This study was designed to assess the pain and adverse effects incurred by women undergoing 4 D HyCoSy. Through evaluating the pelvic pain immediately after 4 D HyCoSy and 30 min after 4 D HyCoSy, the circumstances of the pain relief was also observed. The predictive factors of pain were assessed simultaneously. 827 consecutive women as part of infertility evaluation were included. The pain experienced was then assessed on a 10-cm visual analogue scale (VAS). Each patient was questioned to rate the pain at two different points of time (T1, immediately after 4 D HyCoSy; T2, 30 min after 4 D HyCoSy). 818/827 (98.9%) patients completed the procedure. Pain was experienced by 757/818 (92.5%) of subjects. 30 min after HyCoSy procedure, only 0.5% (4/818) patients feel severe pelvic pain and after 15-30 minutes of rest, these patients were relieved of pain. Age, cycle length, duration of menses, and duration of infertility were not significantly correlated with pain associated with 4 D HyCoSy as assessed by VAS. Women with tubal obstruction experienced a significant increase in 4 D HyCoSy-associated pain. There were significant differences in the degree of pain between different tubal patency (p <0.01). Overall, 4 D HyCoSy, a user-friendly, multidimensional technology, has the advantage of real-time, dynamic, well tolerated, and low serious complications, which make it a good way for evaluating fallopian tubal patency. The technique aids in making choices concerning further procedures for the diagnosis and treatment of infertility. Most of women experience pain associated with the procedure and 30 minute period of observation is useful.
1. Introduction
Tubular and uterine cavity diseases usually influence women's fertility and 14% of couples need professional therapy [Citation1]. For example, uterine anomalies or structural abnormalities of the fallopian tubes are clinically diagnosed in 3% and 16% infertile women, correspondingly [Citation2]. Because of this, tubal and uterine evaluation takes on an essential part in the evaluation of the infertile couples and it is obligatory prior to assisted reproductive techniques (ART) is began [Citation1].
Hysterosalpingo-contrast sonography (HyCoSy) has been presented in clinical process as an useful instrument in the assessment of tubal subfertility as well as the study of uterine and ovarian conditions. It was based on the use of a sonographic contrast medium (e.g. SonoVue, Echovist, Albunex, Infoson, air and sterile saline solution) which, after injection into the uterine cavity, can be seen passing through the fallopian tube.
HyCoSy exhibits high general accuracy in the assessment of both uterine cavity morphology and tubal patency [Citation3–8]. Moreover, HyCoSy prevents both equally being exposed to ionizing rays as well as injection of iodinated contrast medium which could possibly result toxic. Additionally, it can be performed during an out-patient visit, safe, nicely accepted, reduced examination times, and also potentially less side-effects as compared to hysterosalpingography (HSG) [Citation5]. HyCoSy can also be used as a means of therapeutic treatment for infertile women. Lindborg et al. [Citation9] proposed a legitimate reason: small adhesions, mucous plugs or accumulating substances could be eliminated by the passing of the liquid through a partially occluded fallopian tube, thereby restoring tubal patency.
HyCoSy has continued to develop from utilizing a negative contrast agent, for example, saline solution [Citation10] to a positive contrast agent [Citation11] and from 2-dimensional (2 D) to 4-dimensional (4 D) image [Citation12]. In spite of its several unquestionable benefits, HyCoSy is surely an operator-dependent process. Precise movements with the probe on several planes are essential to identify the passing of liquid through the tube in the course of infusion. In addition, since 2 D HyCoSy doesn't provide the entire tube of the image, irregular tubal spasm may be mistaken for occluded tubes and the fluid or even atmospheric flow through the tubes may be wrongly recognized for bowel movements. 4 D HyCoSy overcomes many of these limitations as it improves visualization of the movement of contrast medium throughout the fallopian tube. SonoVue (membrane phospholipids filled with sulfur hexafluoride, Bracco, Milan, Italy) can produce a strong harmonic signal. In 4 D HyCoSy process with SonoVue, the clinician can clearly distinguish between the signals from the microbubbles and the signals from the pelvic organ. This technology has achieved the target of real-time, dynamic and instinctive assessment [Citation13].
Most of women encounter pain in the course of the HyCoSy procedure [Citation14–16]. Several studies have demonstrated the pain, side effects, and tolerability of HyCoSy, using a variety of materials for air microbubble suspensions [Citation14,Citation15]. Some investigators have evaluated the diagnostic accuracy of 4 D HyCoSy [Citation13,Citation16]. Recent study has also found that using paracetamol + codeine before the ultrasound assessment procedure reduces the pain level, but randomized controlled trials are required [Citation17]. However, insufficient data have been available about the pain and side effects associated with 4 D HyCoSy. Particularly, vasovagal responses, pelvic pain, pelvic inflammatory disease, fever, and hemorrhage have been described, however the actual occurrence of these kind of adverse events in a large population of women consecutively undertaking 4 D HyCoSy are unknown. The aims of the present study were to assess the pain and adverse effects in a large series of patients consecutively undergoing 4 D HyCoSy with a standardized technique. The predictive factors of pain associated were assessed simultaneously. Through evaluate the pelvic pain immediately after HyCoSy and 30 min after HyCoSy, we also observed the pain decrease within 30 minutes.
2. Materials and methods
827 consecutive patients (ranging in age from 19 to 46 years, mean age 29.6 years) referred for tubal patency evaluation between January 2015 and December 2016 answered a questionnaire immediately after 4 D HyCoSy examination. Approval for the study was obtained from the institutional review board and ethics committee (the Affiliated Hospital of Nanjing University of Chinese Medicine). All patients were clinically documented as being infertile. Inclusion criteria were as follows: 1) no vaginal bleeding; 2) no inflammation of the reproductive system and 3) no evidence of hydrosalpinx on ultrasound examination. Instantly preceding to the HyCoSy process, participants were asked to finish an anonymous health questionnaire to collect to get information about obstetrics and gynecologic historical anamnesis, which includes earlier pregnancies, menstrual history, and any previous gynecologic diagnoses.
4 D HyCoSy were performed in a single centre by the same group of physicians in a similar fashion. The process as well as possible side effects was stated, and written consent was received from all patients. All ultrasound exams were performed utilizing the GE Medical Systems, Voluson E8 Expert ultrasound device (equipped with dedicated 4 D imaging software program as well as CCI mode), and using a 5-9 MHz transvaginal volume probe. Detailed sonographic examination was performed in longitudinal and transverse planes and any uterine, fallopian tubes and ovarian abnormalities noted. The patient’s vulva as well as vagina was cleaned and a speculum was placed inside the vagina. A Foley’s catheter (dimension 8-10) was presented into the uterine cavity. To guarantee that the catheter was not removed from the uterine cavity, sterile saline solution (1.5-2 ml) was injected into the catheter balloon. The ultrasound probe was reintroduced into the vagina to confirm the position of the balloon after the speculum was taken out. After syringing 5 ml physiologic saline assessment of the uterine cavity followed. 4 D HyCoSy was then carried out applying SonoVue. 5 ml 0.9% physiological saline solution was injected into 59 mg of SonoVue freeze-dried powder to form a microbubble suspension, and then 2 ml of the microbubble suspension was taken and diluted to 20 ml with saline solution for assessment. 4 D HyCoSy was performed as the following [Citation13].
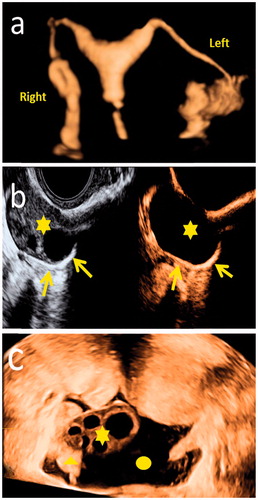
4 D volume acquisition was carried out in the course of injection and the widest possible area of interest was established to ensure that the uterus and the two ovaries were observed and allowing the entire length of the fallopian tube to be found. Instrument parameters were as subsequent: frequency (6-9 MHz); sweep angle (120); sweep velocity (medium quality); 3 D box size (exceeding beyond the uterus and the two ovaries by 1 cm). Specific software permitted the volume data of the contrast to be acquired instantly for the following evaluation. The duration of volume data was about 45 s. The evaluation of tubal patency was carried out during the process. The patency of the tube was decided by the passing of microbubbles (SonoVue contrast agent) through the tube the existence of a ring-like spill of free microbubbles (SonoVue contrast agent) around the ipsilateral ovary, and the fluid collection in pelvic cavity ().
Figure 1. 4-dimensional HyCoSy using SonoVue: (a) Both the fallopian tube and uterus were clearly visible. (b) contrast agent ringlike diffusion (arrow) around the ovary (asterisks). (c) the fallopian tubes (triangle) located on the side of ovary (asterisks) and the fluid collection (round) was an indirect sign of tubal patency.
Following the examination and discussion of the results, the women remained in the waiting room for 30 minutes to diagnose and treat potential late side effects. Pain scores were obtained using a Visual Analog Scale (VAS) immediately after 4 D HyCoSy (designated as T1) and 30 min after 4 D HyCoSy (designated as T2). The individuals were familiar with the scale before the process was carried out. Patients pointed out the maximum pain intensity encountered by making a vertical line on the VAS. In accordance to Savelli et al [Citation18], we considered “absent” pelvic pain to be a score as 0 VAS, “mild” pelvic pain to be a score from 1 to 4 VAS, “moderate” from 5 to 7 VAS, and “severe” from 8 to 10 VAS.
3. Statistical analysis
Pain scores documented by VAS were documented as mean ± standard error. The Mann-Whitney U and Kruskal-Wallis tests were utilized to evaluate non-parametric continuous measures. Spearman correlation coefficients were calculated to correlate predictors of pain with the VAS outcomes. Data were assessed utilizing IBM SPSS Statistics software (Version 19, IBM Corporation, Somers, NY). Values of P < 0.05 were taken to indicate statistical significance.
4. Results
In 818 of the 827 patients (98.9%), the procedure was completed, without technical failure during the 4 D HyCoSy. The study was discontinued in 9 women (1.1%) because of cervical stenosis or uterine flexion that prevented the insertion of the catheter (4 patients), or intolerance to speculum insertion and inadequate collaboration (5 patients). The time between the attachment and removal of the catheter varied from 15 to 30 minutes. The amount of the contrast substance used ranged from 10–37 ml (mean, 28.02 ± 5.79). The clinical qualities along with the outcomes are listed ( and ).
Table 1. Clinical qualities and the 4 D HyCoSy outcomes.
Table 2. Pain perception and side effects.
Pain was experienced by 757/818 (92.5%) of subjects. Immediately after examinations, the minority of patients (61/818;7.5%) considered HyCoSy a non-painful procedure, whereas 36.3% (297/818) reported mild pelvic pain (1 to 4 VAS) and 35.1% (287/818) classified the discomfort as “moderate” (5 to 7 VAS). 21.1% (173/818) of the population experienced severe pelvic pain (8 to 10 VAS). When present, pain was referred as uterine cramping or dysmenorrhea-like discomfort; three women reported mild right shoulder pain in addition. Only 0.5% (4/818) patients feel severe pelvic pain 30 min after 4 D HyCoSy. Then after 15-30 minutes of rest, the four patients were relieved of pain. A mild, self-limiting vasovagal reaction (manifesting as pallor, sweating, nausea, bradycardia, and hypotension) was experienced by 18 out of 818 patients (2.2%). These patients were looked after until recovery, which was spontaneous and complete within 30 minutes.
Of the demographic and clinical variables assessed, only tubal blockage was significantly correlated with pain during 4 D HyCoSy as measured by VAS. Regarding tubal blockage, the mean pain scores were 4.43 ± 2.62 for bilateral passage, 6.69 ± 2.98 for monolateral patency, and 6.42 ± 3.32 for bilateral obstruction. Tubal occlusion at the time of the procedure was positively correlated with experience of pain. Age, cycle length, duration of menses, and duration of infertility were not significantly correlated with pain associated with 4 D HyCoSy as assessed by VAS. showed the pain perception in patients with different degrees of patency. There were significant differences in the degree of pain between different tubal patency (P < 0.01).
Table 3. The pain perception in patients with different degrees of patency.
5. Discussion
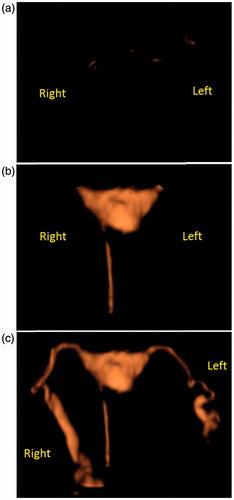
This study is the first large sample to report the pain associated with 4 D HyCoSy for assessing fallopian tube patency. In this work, all 4 D HyCoSy were performed in a single centre by the same group of physicians in a similar fashion. HyCoSy is an essential part of the assessment of subfertile women, because it can be utilized to evaluate intrauterine pathology as well as tubal patency. 3 D HyCoSy overcame the drawbacks associated with 2 D HyCoSy. 4 D HyCoSy not just inherited the benefits of 3 D HyCoSy but additionally surpassed it in lots of aspects. The dynamic character of 4 D HyCoSy allowed viewing of the whole process of contrast advancement instead of an instantaneous catch (). The dynamic observation feature avoids false positive conclusions due to a tubal circuit or tubal stenosis.
Figure 2. 4 D HyCoSy process: (a) contrast agent was not injected in the beginning. (b) contrast agent was injected into the catheter and next entered in the uterus. (c) Lastly, contrast agent developed in the bilateral fallopian tubes.
Within this test of sequential, unselected, infertile women going through routine infertility investigations, 4 D HyCoSy came out to be both technically feasible for the operators to execute and acceptable as an out-patient process to those people undertaking examination. It was possible to finish all of the 4 D HyCoSy process for 818 (98.9%) women. Only 1.1% (9/827) of the examinations was not finished due to vasovagal reactions or technical difficulty with the catheterization process. Majority of individuals undergoing 4 D HyCoSy encounter pain in some form connected with the procedure. Based on the outcomes acquired, about 50% of individuals explained only mild discomfort and there were no serious late complications, for instance post procedural fever, acute pelvic infection, or peritonitis. This agreed with previous studies [Citation19]. The pain encountered by the individuals is generally similar to the cramping pain sensed within a normal menstrual cycle. Despite many patients reporting pain during the procedure, all of the patients reported satisfaction with the procedure.
Prior articles documented that the mean times (12 to 13.9 minutes) and the contrast agent doses (5 to 15 ml) for 2 D HyCoSy [Citation5,Citation20–22]. In our research, the longest whole assessment time attained 30 minutes, and the maximum SonoVue dosage arrived at 37 ml, primarily due to lack of experience in the beginning. The method utilized as well as the experience of the physician carrying out the HyCoSy process considerably have an effect on level of patient discomfort and pain [Citation23]. We attempted to look for a better assessment process and the proficiency of intubation and operation reduced the use less of the SonoVue and the overall examination time. Similar research were documented by Savelli et al. [Citation18] The authors examined the mean numeric rating scale in 669 infertile women going through 2 D HyCoSy. Compared with Savelli et al, our study found patients with a higher mean numeric rating scale (4.7 ± 2.6 vs 2.7 ± 2.5) and higher proportion of patients who felt moderate or severe pain. However, we observed that our study had higher proportion of bilateral fallopian tube obstruction and unilateral fallopian tube obstruction. In addition, the contrast agent dose (10-37 ml VS 5-10 mL) were more. These may be the reason for the high pain value.
The relationship between pain perception and other independent variables related to 4 D HyCoSy (i.e. age, cycle length, duration of menses, duration of infertility, unilateral or bilateral tubal blockage) was also investigated. The only strong association discovered concerned tubal patency, given that women with bilateral tubal stenosis encountered higher rates of serious discomfort, pain and/or vagal effects in comparison with patients with patent tubes. In patients having tubal obstruction, the increased volume of SonoVue microbubble suspension collected in the uterine cavity in the course of 4 D HyCoSy and the intrauterine pressure attained through the process may lead to over distension of the uterine muscular fibers. Prostaglandin release (due to the mechanical expansion of the uterine wall) caused uterine cramps, which is the cause for the pain or the discomfort that some patients encounter during and after the process [Citation24]. These results may help with more personalized counseling. Patients at high-risk for tubal occlusion ought to be counseled prior to the procedure that they may encounter more pain or pelvic discomfort through the process. This kind of counseling may enhance patient anticipations and therefore satisfaction with the procedure, and assist reduce discomfort. Of note, during the 4 D HyCoSy, emotional support (at the bedside speaking to the patient and holding her hand) contributed to the patients’ satisfaction. We recommend taking time before the procedure for exhaustive preliminary counseling to inform the patient that mild pelvic discomfort normally occurs, probably due to uterine contractions.
Poor pain control can often limit the quality of the examination. Furthermore, anticipation of pain may preclude patient acceptance of the examination and cause unnecessary anxiety. Intrauterine placement of the catheter and balloon inflation can cause probable discomfort or pain experience of the patients due to cervical manipulation and uterine expansion. While over 80% of our patients noted pain during the process, it vanished in the majority of cases after 4 D HyCoSy process. This was possibly because the discomfort and cramping occured not just to the injections but also to the balloon catheter within the uterine cavity. Inflation of the catheter’s balloon induced the nerve fibers of the uterine cervix, leading to pelvic pain and vasovagal response. In addition, local prostaglandins release (due to of the uterine expansion) caused uterine cramps and pain [Citation25]. In our study, we found that inflating the balloon inside the uterine cavity was more painful and could result in a larger number of vasovagal reactions. Therefore, we recommend inflating the balloon slowly with suitable volume of saline enough to block the cervical canal and prevent a backflow of contrast agent without creating much discomfort for the patient. As the pain perceived by the patient could be related to the grade of distension of the uterine cavity, we suggest using the least amount of the contrast agent possible, injecting them slowly.
This study also observed the pain decrease within 30 minutes. 30 min after 4 D HyCoSy, the vast majority patients have been eased, but still 4 patients feel severe pelvic pain. The common feature of these patients was a diagnosis of unilateral patency or bilateral tubal occlusion. This result suggests more time for observation and rest in patients with a high degree of suspicion for tubal obstruction. We found a 30 minutes period of observation is useful after 4 D HyCoSy. First, some patients still have pain after the end of the fallopian tube reaction and need a short break; the second is the need to diagnose and treat potential late side effects.
This research has limitation. Although all exams were carried out by the same group of physicians, the degree of proficiency of each inspection process was different as a result of this new technology. Therefore, the beginning of the inspection time was much longer, and then became shorter.
6. Conclusion
Overall, 4 D HyCoSy, a user-friendly, multidimensional technology, has the advantage of real-time, dynamic, well tolerated, and low serious complications, which make it a good way for evaluating fallopian tubal patency. The technique aids in making choices concerning further procedures for the diagnosis and treatment of infertility.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- ESHRE Capri Workshop Group. Diagnosis and management of the infertile couple: missing information. Hum Reprod Update. 2004;10:295–307.
- Spira A. Epidemiology of human reproduction. Hum Reprod. 1986;1:111–115.
- Luciano DE, Exacoustos C, Johns DA, et al. Can hysterosalpingo-contrast sonography replace hysterosalpingography in confirming tubal blockage after hysteroscopic sterilization and in the evaluation of the uterus and tubes in infertile patients? Am J Obstet Gynecol. 2011;204:79. e1–79. e5.
- Graziano A, Monte GL, Soave I, et al. Sonohysterosalpingography: a suitable choice in infertility workup. J Med Ultrason (2001). 2013;40:225–229.
- Ayida G, Kennedy S, Barlow D, et al. A comparison of patient tolerance of hysterosalpingo–contrast sonography (HyCoSy) with Echovist®‐200 and X‐ray hysterosalpingography for outpatient investigation of infertile women. Ultrasound Obstet Gynecol. 1996;7:201–204.
- Lim CP, Hasafa Z, Bhattacharya S, et al. Should a hysterosalpingogram be a first-line investigation to diagnose female tubal subfertility in the modern subfertility workup? Hum Reprod. 2011;26:967–971.
- Tanawattanacharoen S, Suwajanakorn S, Uerpairojkit B, et al. Transvaginal hysterosalpingo‐contrast sonography (hycosy) compared with chromolaparoscopy. J Obstet Gynaecol Re. 2000;26:71–75.
- Stacey C, Bown C, Manhire A, et al. HyCoSy-as good as claimed? Br J Radiol. 2000;73:133–136.
- Lindborg L, Thorburn J, Bergh C, et al. Influence of HyCoSy on spontaneous pregnancy: a randomized controlled trial. Hum Reprod. 2009;24:1075–1079.
- Mitri FF, Andronikou AD, Perpinyal S, et al. A clinical comparison of sonographic hydrotubation and hysterosalpingography. Br J Obstet Gynaecol. 1991;98:1031–1036.
- Ayida G, Harris P, Kennedy S, et al. Hysterosalpingo-contrast sonography (HyCoSy) using Echovist®-200 in the outpatient investigation of infertility patients. Bjr. 1996;69:910–913.
- Exacoustos C, Di Giovanni A, Szabolcs B, et al. Automated sonographic tubal patency evaluation with three‐dimensional coded contrast imaging (CCI) during hysterosalpingo‐contrast sonography (HyCoSy). Ultrasound Obstet Gynecol. 2009;34:609–612.
- He Y, Geng Q, Liu H, et al. First experience using 4‐dimensional hysterosalpingo‐contrast sonography with sonovue for assessing fallopian tube patency. J Ultras Med. 2013;32:1233–1243.
- Marci R, Marcucci I, Marcucci AA, et al. Hysterosalpin-gocontrast sonography (HyCoSy): evaluation of the pain perception, side effects and complications. Bmc Med Imaging. 2013;13:28.
- Socolov D, Boian I, Boiculese L, et al. Comparison of the pain experienced by infertile women undergoing hysterosalpingo contrast sonography or radiographic hysterosalpingography. Int J Gynaecol Obstet. 2010;111:256–259.
- Wang W, Zhou Q, Gong Y, et al. Assessment of fallopian tube fimbria patency with 4‐dimensional hysterosalpingo‐contrast sonography in infertile women. J Ultras Med. 2017. DOI:10.1002/jum.14244
- Ludwin I, Martins WP, Nastri CO, et al. Pain intensity during ultrasound assessment of uterine cavity and tubal patency with and without painkillers: prospective observational study. J Minim Invas Gyn. 2017;24:599–608.
- Savelli L, Pollastri P, Guerrini M, et al. Tolerability, side effects, and complications of hysterosalpingocontrast sonography (HyCoSy). Fertil Steril. 2009;92:1481–1486.
- Saunders RD, Shwayder JM, Nakajima ST. Current methods of tubal patency assessment. Fertil Steril. 2011;95:2171–2179.
- Hamilton JA, Larson AJ, Lower AM, et al. Evaluation of the performance of hysterosalpingo contrast sonography in 500 consecutive, unselected, infertile women. Hum Reprod. 1998;13:1519–1526.
- Boudghene FP, Bazot M, Robert Y, et al. Assessment of Fallopian tube patency by HyCoSy: comparison of a positive contrast agent with saline solution. Ultrasound Obstet Gynecol. 2001;18:525–530.
- Lanzani C, Savasi V, Leone FPG, et al. Two-dimensional HyCoSy with contrast tuned imaging technology and a second-generation contrast media for the assessment of tubal patency in an infertility program. Fertil Steril. 2009;92:1158–1161.
- Zhou L, Zhang X, Chen X, et al. Value of three–dimensional hysterosalpingo–contrast sonography with SonoVue in the assessment of tubal patency. Ultrasound Obstet Gynecol. 2012;40:93–98.
- Guney M, Oral B, Bayhan G, et al. Intrauterine lidocaine infusion for pain relief during saline solution infusion sonohysterography: a randomized, controlled trial. J Minim Invas Gyn. 2007;14:304–310.
- Moro F, Selvaggi L, Sagnella F, et al. Could antispasmodic drug reduce pain during hysterosalpingo–contrast sonography (HyCoSy) in infertile patients? A randomized double‐blind clinical trial. Ultrasound Obstet Gynecol. 2012;39:260–265.
