Abstract
This study aimed to compare the accuracy of navigation-assisted percutaneous pedicle screw insertions between traditional posterior superior iliac spine (PSIS) fixed and cutaneously fixed dynamic reference frame (DRF) in minimally invasive surgery of transforaminal lumbar interbody fusion (MIS TLIF). This is a prospective randomized clinical study. Between May 2016 and Nov 2017, 100 patients who underwent MIS TLIF were randomly divided into bone fixed group (with PSIS fixed DRF) and skin fixed group (with cutaneously fixed DRF). The pedicel screws were inserted under navigational guidance using computed tomography (CT) data acquired intraoperatively with a Ziehm 3-dimensional fluoroscopy-based navigation system. Screw positions were immediately checked by a final intraoperative scan. The accuracy of screw placement was evaluated by a sophisticated computed tomography protocol. Both groups had similar patient demographics. Totally Five-hundred Twelve pedicle screws were placed in the lumbar spine. There were 2 moderate (2–4 mm) pedicle perforations in each group. The accuracy showed no significant difference between bone fixed and skin fixed DRF. There were no significant procedure-related complications. The skin fixed DRF provides similar accuracy in pedicle screw insertions with bone fixed DRF using intraoperative 3D image guided navigation in MIS TLIF. Skin fixed DRF not only serves as an alternative method but also saves a separate incision wound for bony attachment.
Introduction
Computer-assisted pedicle screws insertions have been developed using pre-surgical diagnostic computed tomography (CT) scans, 2Dfluoroscopy, and intra-operatively acquired data sets from 3D-fluoroscopy or cone-beam CT [Citation1,Citation2]. MIS TLIF offers patients a safe and effective surgical treatment option to treat degenerative lumbar spine disease [Citation3]. With navigation guidance, 3-dimensional stereotactic navigation based upon intraoperative computed tomography imaging offers remarkable enhanced accuracy of percutaneous lumbar pedicle screw placement when used in MISTLIF [Citation4]. An additional incision on posterior superior iliac spine (PSIS) remained a recommended setting of dynamic reference frame (DRF) in MISTLIF [Citation5], despite a sustained source of streak artifact.
Skin or cutaneously fixed DRF might be a simple and reliable method for 3D navigation in anterior cervical surgery [Citation6]. To the best of our knowledge, this is the first prospective randomised study comparing the accuracy of traditional PSIS fixed and cutaneoulsy fixed DRF for navigation-assisted percutaneous pedicle screw insertions in MIS TLIF.
Methods
Between May 2016 and Nov 2017, 101 patients who underwent MIS TLIF with intraoperative 3-dimensional C-arm (Vision FD Vario 3D, Ziehm Imaging, Nuremberg, Germany) and navigation system (Kick navigation system, Brainlab) for percutaneous pedicle screw insertions in our institute were enrolled prospectively after institutional review board approval.
Indications for surgery were grade 1 spondylolisthesis with spinal stenosis, pars fractures, and degenerative discs with back pain or radiculopathy. The surgical level ranges from the second lumbar vertebra (L2) to the first sacral vertebra (S1). All surgeries were performed by a single surgeon. Patients with previous spine surgery, systemic autoimmune disease, and severe obesity (BMI >35) were excluded.
They were randomly distributed to either bone fixed group or skin fixed group using computer-generated random numbers. Navigation assisted percutaneous pedicle screw insertions were performed before microscope-assisted MIS TLIF. Patients in bone fixed group underwent percutaneous screw insertions with traditional PSIS placement of DRF.
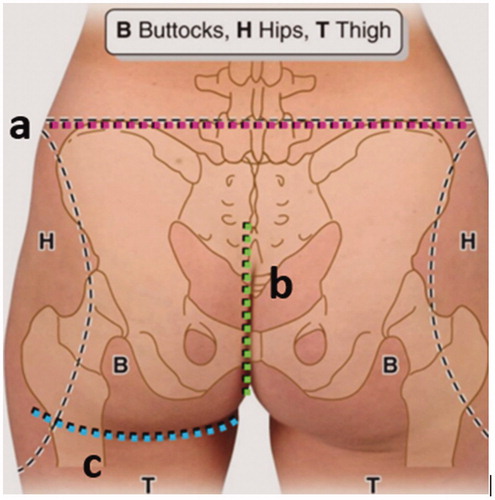
The DRF in skin fixed group was fixed cutaneously on the middle of sacral hiatus area after confirming the landmarks including iliac crest, posterior superior iliac spine, and intergluteal cleft.with sterile tapes as close as possible to the surgical field (). The large transparent drape serves as a barrier to the sterile field and is typically not in contact with the CT device.
Figure 2. Skin fixed DRF on the midline instead of bone fixed DRF on one side of PSIS or spinous process. Skin fixed DRF could be placed as close as possible to the surgical field without hindering the navigation during screw placement.
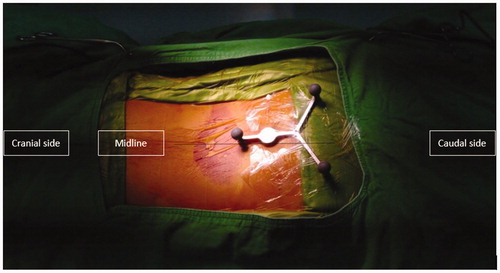
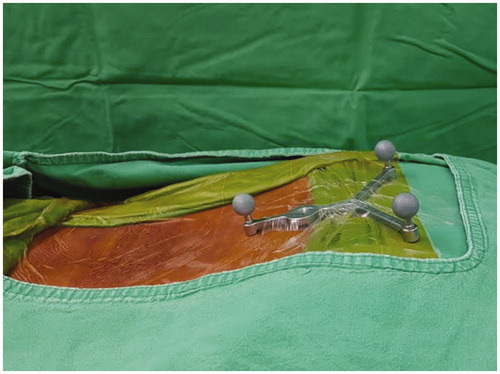
Figure 3. Lateral picture of the skin fixed DRF on the area between iliac crest line and integluteal cleft.
Intraoperative scanning was performed in both groups with CT data set automatically registered to the image guidance system. Before the skin incision was made, the spinal process was used as an anatomical landmark by navigation probe to confirm the accuracy of navigation. The ideal skin entry points were sought with the navigation probe tip in order to determine the precise skin incision based on the virtual elongated navigation trajectory on the intraoperative scanned images. Pedicle entry points were decided on navigation guidance, and pilot holes were made with a 3-mm awl. The direction of the pilot pedicle hole was rechecked with the navigation probe, and 4.5-mm tapping was done to a depth of 20 mm from the entry point. A guidewire was used for screw insertion. After all the screws had been inserted, a second CT scan was performed to verify their actual positions.
Pedicle screw accuracy and penetration of the internal, external, superior, or inferior cortical walls of the pedicles was measured in millimeters in the second CT scan using all 3 planes to seek possible cortical breaches of the pedicle borders. The accuracy of the navigation was assessed mainly on axial and sagittal planes using the classification of 2-mm increment [Citation7,Citation8] from Gertzbein and Robbins, et al.: grade 0, no pedicle breach; grade 1, violation ≤2 mm; grade 2, violation of 2–4 mm; and grade 3, violation ≥4 mm. The assessment of the images and measurements of the pedicle perforations were performed by a junior surgeon who was involved in the surgery and a senior surgeon who was independent of the surgeries immediately after second CT scan was performed. In cases with screw malpositioning (grade 3), repositioning of the screw was done under navigation guidance again, and a final CT scan was performed.
Statistical analysis
Patients’ age, body mass index (BMI), preoperative VAS, preoperative ODI, and operative time were analyzed with independent sample t test. The perioperative accuracy of pedicle screw insertions were analyzed using paired t test. Each patient’s clinical outcome was evaluated pre-operatively, 2-week, 1, and 6 months post-operatively during outpatient follow-up. Evaluations were made by an independent researcher who was not aware of whether the patient was assigned to the study group or the control group. Statistical significance was set at p<.05. All statistical analyses were performed using SPSS version 20 (IBM, Chicago, IL, USA).
Results
The mean age of the patients was 67.9 ± 13.3 years (range, 49–84 years) in bone fixed group and 63.0 ± 12.0 years (range, 31–87 years) in skin fixed group. The mean BMI of the patients was 25.2 kg/m2 in bone fixed group and 25.7 kg/m2 in skin fixed group. In bone fixed group, 26 and 24 patients underwent one- and two-level surgery, respectively, whereas in skin fixed group, 27 and 18 patients underwent one- and two-level surgery, respectively. Three-level fusion was performed totally in 6 patients. Patient demographic data and distribution of screws showed no significant difference. ().
Table 1. Patient demographics.
In total, four hundred ninety one pedicle screws had no violation, seventeen screws had a grade 1 violation, and four screws had a grade 2 violation. No grade 3 violations were observed in this study. The immediate scan of all two hundred eighty screws in bone fixed group () and 232 screws in skin fixed group () demonstrated an accuracy rate of 96.0% and 95.7%. All screws with grade 1 violation were acceptable while screws with grade 2 violation were changed intraoperatively with the third additional scan. There was no significant difference between the accuracies in both groups (). Grading of cortical breaches of the pedicle borders by the screws in the lateral and medial directions are illustrated in .
Figure 4. Pedicle screw assessment in the postoperative CT scans. (A) left grade 1 medial encroachment (B) right grade 2 lateral encroachment (C) upper screw with grade 1 cranial encroachment (D) lower screw with grade 1 caudal encroachment.
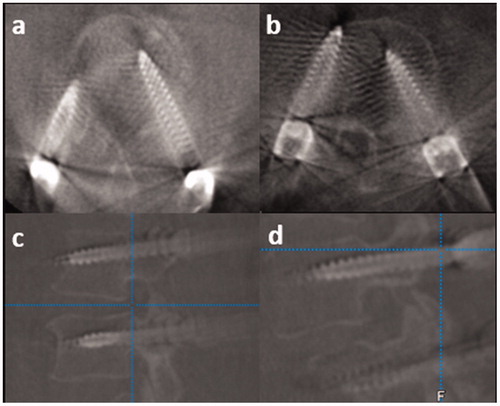
Table 2. Screws position evaluation in PSIS fixed DRF.
Table 3. Screws position evaluation in cutaneously fixed DRF.
Table 4. Screw accuracies in both groups.
Table 5. Perioperative clinical outcomes.
We did not observe any frank misplacement in the penetration in the disc or over-penetration along the anterior position in the reformatted images. Instrumentation related complications, such as nerve root injury, cerebrospinal fluid leakage, and internal organ injury, were not observed in the patient population. All patients did not have any complaint postoperatively, and no revision surgery was needed because of screw misplacement.
The preoperative VAS was 7.2 in group A and 7.3 in group B, and the preoperative ODI was 76.0 in group A and 75.8 in group B. There were no significant differences in preoperative VAS (p=.88) and ODI (p=.90) between the two groups (). The patients VAS and ODI scored significantly improved after surgery in both groups. The VAS scored at 2 weeks was 2.8 in group A and 2.9 in group B. The ODI scored at 1 month was 18.2 in group A and 19.0 in group B, whereas the ODI scored at 6 months was 22.8 in group A and 22.6 in group B. There was no significant difference in clinical outcomes between both groups afterwards.
Discussion
Computerized tomography-based spinal image guidance has evolved from paired point matching, paired point matching combined with surface matching [Citation9], three dimensional rotational X- ray [Citation10], three dimensional CT based navigation [Citation11]. The accuracy of the navigation system depending on the integrity of the connected components of the system, and the stability of DRF, which are the critical parts of navigation surgery. Traditionally, the DRF is fixed in the spinal process [Citation12] or PSIS [Citation5,Citation11] to prevent the movement, synchronization of the visual data set, and the actual anatomical positions. However, placement of DRF on PSIS may require another separate incision wound, hinder the surgical procedure, interfering with the navigation, and compromising the accuracy in MIS TLIF [Citation13].
Some studies reported successfully placed the reference frame away from the surgical field with acceptable screw placement accuracies in cervico-occipital surgeries [Citation14,Citation15]. In lumbar spine surgery; however, the surgical field is larger and sometimes exceeds the navigation field. For lumbosacral surgeries, the close proximity of the reference frame may also cause streak artifacts with an increased risk of screw malposition.
In this study, DRF can be fixed on the skin as close to the surgical field as possible and the risk of a misplaced incision can be minimized. The magnitude of the additional sources of error may be mitigated by reducing the distance between reference frame and the end of the base as well as by integrating the reference frame on the needle. On the other hand, a drill connected to the navigation system was recommended to prevent shifting from the severely degenerated facet joints, especially in overweight patients. Despite the absence of any bony attachment, minimal movement of the DRF can be secured during the procedure. Therefore, the accuracy of navigation and pedicle screw insertions remain acceptable. Moreover there was no significant difference between the two groups.
Accuracy results for 50 patients (95%) who had all pedicle screws installed with computer assistance proved statistically better than results for a control group of 100 patients (85%) instrumented with a conventional technique using biplanar fluoroscopy [Citation16]. Similar screw placement accuracies are reported in multiple recent studies with navigation-assistance, all using postoperative CT scan to determine the screw placement accuracy [Citation11,Citation12,Citation17–20]. Most studies reported 98% to 99% of their screws being placed within a 2 mm pedicle breach margin despite slightly different methods of screw placement.
In general, perforations of less than 2 mm medially or laterally on CT scans are not considered to be associated with clinical sequelae. Injury to the neurological structures through the medial cortex is not common with approximately 2–5 mm width of the safety zone between the medial pedicle cortex and dura, and a neurological complication rate of 0.5% was reported [Citation21]. Injury to the vascular structures through the lateral and anterior cortex should be minimized by preoperative planning, especially in thoracic spine [Citation16].
Superiorly and inferiorly placed pedicle screw is more common in cervical spine than thoracolumbar spine [Citation22]. Average distance from the lumbar pedicle to the adjacent nerve roots superiorly and inferiorly through the cranial to caudal lumbar levels ranged from 4.12 to 5.52, and from 1.10 to 1.06 mm, respectively [Citation23]. As a result, it is very important not to perforate the inferior cortex at all lumbar levels [Citation24].
The screw malposition rate was not significantly different in both groups in the current study. Intraoperative CT scans were minimized to the required level of surgical interest, and the whole process took less than approximately 30 seconds. Each patient had two scans with the exception of 4 patients with grade 2 violation had a third scan. Intraoperative scans allowed immediate evaluation and correction of the screw which would decrease surgical revision rate.
The main limitation of this study was that only medial and lateral deviations in the axial plane, and superior and inferior deviations in the sagittal plane were assessed. The navigation system did not provide actual deviation of each screw. The advantages of cutaneously fixed DRF include, first, the preservation of another incision wound on PSIS with easier set-up process. Second, less interference was noted during the navigation with the DRF fixed on the skin than fixed on PSIS. Reviewing the literature, this is the first study comparing the two methods of navigation. However, further studies regarding clinical outcomes including pain and functional scores are necessary.
Conclusions
The skin fixed DRF provides similar accuracy in pedicle screw insertions with bone fixed DRF using intraoperative 3D image guided navigation. Skin fixed DRF may serve as an alternative method in MIS TLIF.
Acknowledgements
The study was supported by Division of Spine Surgery, Orthopaedic Department, Taipei Veterans General Hospital. We thank Hsin-Yi Huang from the Biostatistics Task Force, Taipei Veterans General Hospital, for the statistical assistance.
Disclosure statement
The authors declare that no benefits in any forms have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- Girardi FP, Cammisa FP, Jr, Sandhu HS, et al. The placement of lumbar pedicle screws using computerised stereotactic guidance. J Bone Joint Surg Br. 1999;81–85:825–829.
- Balling H. Time demand and radiation dose in 3d-fluoroscopy based navigation-assisted 3d-fluoroscopy-controlled pedicle screw instrumentations. Spine (Phila Pa 1976). 2018;43(9):E512–E519.
- Tsahtsarlis A, Wood M. Minimally invasive transforaminal lumber interbody fusion and degenerative lumbar spine disease. Eur Spine J. 2012;21(11):2300–2305.
- Bourgeois AC, Faulkner AR, Bradley YC, et al. Improved accuracy of minimally invasive transpedicular screw placement in the lumbar spine with 3-dimensional stereotactic image guidance: a comparative meta-analysis. J Spinal Disord Tech. 2015;28(9):324–329.
- Best NM, Sasso RC, Garrido BJ. Computer-assisted spinal navigation using a percutaneous dynamic reference frame for posterior fusions of the lumbar spine. Am J Orthop (Belle Mead NJ). 2009;38(8):387–391.
- Jang SH, Cho JY, Choi WC, et al. Novel method for setting up 3D navigation system with skin-fixed dynamic reference frame in anterior cervical surgery. Comput Aided Surg. 2015;20(1):24–28.
- Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15(1):11–14.
- Wang MY, Kim KA, Liu CY, et al. Reliability of three-dimensional fluoroscopy for detecting pedicle screw violations in the thoracic and lumbar spine. Neurosurgery. 2004;54(5):1138–1142; discussion 42–43.
- Holly LT, Bloch O, Johnson JP. Evaluation of registration techniques for spinal image guidance. J Neurosurg Spine. 2006;4(4):323–328.
- van de Kraats EB, van Walsum T, Verlaan JJ, et al. Three-dimensional rotational X-ray navigation for needle guidance in percutaneous vertebroplasty: an accuracy study. Spine (Phila Pa 1976). 2006;31(12):1359–1364.
- Joseph JR, Smith BW, Patel RD, et al. Use of 3D CT-based navigation in minimally invasive lateral lumbar interbody fusion. J Neurosurg Spine. 2016;25(3):339–344.
- Rampersaud YR, Pik JH, Salonen D, et al. Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine (Phila Pa 1976). 2005;30(7):E183–E190.
- Lang Z, Tian W, Liu Y, et al. Minimally invasive pedicle screw fixation using intraoperative 3-dimensional fluoroscopy-based navigation (CAMISS Technique) for Hangman fracture. Spine (Phila Pa 1976). 2016;41(1):39–45.
- Nottmeier EW, Young PM. Image-guided placement of occipitocervical instrumentation using a reference arc attached to the headholder. Neurosurgery. 2010;66(3Suppl Operative):138–142.
- Hott JS, Papadopoulos SM, Theodore N, et al. Intraoperative Iso-C C-arm navigation in cervical spinal surgery: review of the first 52 cases. Spine (Phila Pa 1976). 2004;29(24):2856–2860.
- Amiot LP, Lang K, Putzier M, et al. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine (Phila Pa 1976) 2000;25(5):606–614.
- Acosta FL, Jr, Thompson TL, Campbell S, et al. Use of intraoperative isocentric C-arm 3D fluoroscopy for sextant percutaneous pedicle screw placement: case report and review of the literature. Spine J. 2005;5(3):339–343.
- Rajasekaran S, Vidyadhara S, Ramesh P, et al. Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa 1976) 2007;32(2):E56–E64.
- Tian NF, Xu HZ. Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop. 2009;33(4):895–903.
- Cho JY, Chan CK, Lee SH, et al. The accuracy of 3D image navigation with a cutaneously fixed dynamic reference frame in minimally invasive transforaminal lumbar interbody fusion. Comput Aided Surg. 2012;17(6):300–309.
- Schulze CJ, Munzinger E, Weber U. Clinical relevance of accuracy of pedicle screw placement. A computed tomographic-supported analysis. Spine (Phila Pa 1976). 1998;23(20):2215–2220; discussion 20–21.
- Hojo Y, Ito M, Suda K, et al. A multicenter study on accuracy and complications of freehand placement of cervical pedicle screws under lateral fluoroscopy in different pathological conditions: CT-based evaluation of more than 1,000 screws. Eur Spine J. 2014;23(10):2166–2174.
- Soyuncu Y, Yildirim FB, Sekban H, et al. Anatomic evaluation and relationship between the lumbar pedicle and adjacent neural structures: an anatomic study. J Spinal Disord Tech. 2005;18(3):243–246.
- Du JY, Wu JS, Wen ZQ, et al. Treatment strategies for early neurological deficits related to malpositioned pedicle screws in the lumbosacral canal: a pilot study. Bone Joint Res. 2016;5(2):46–51.