Abstract
To examine the clinical results of different minimally invasive techniques for the therapy of far lateral disc herniation in middle-aged and elderly patients. An endoscopic approach (percutaneous endoscopic lumbar discectomy; PELD), MIS-TLIF combined with contralateral translaminar screw (MIS-TLIF CTS), and MIS-TLIF combined with bilateral pedicle screws (MIS-TLIF BPS) were evaluated via a retrospective chart review. Data from 74 consecutive middle-aged and elderly patients with far lateral disc herniation were analyzed. All patients underwent surgery; 19 with PELD, 24 with MIS-TLIF CTS, and 31 with MIS-TLIF BPS. Clinical data included the length of the incision, duration of the operation, estimated blood loss, hospitalization time, operation cost, recurrence rate, and fusion rate. Preoperative and postoperative patient outcomes including the VAS, ODI scores and MacNab criteria were assessed and recorded. The mean follow-up time was 26.4 months (range from 14 to 46 months). Compared with the internal fixation groups, the length of the incision, duration of operation, estimated blood loss, and hospitalization time were obviously lower in the PELD group. The difference in operation cost among the three methods was statistically significant. The postoperative VAS scores for LBP and LP decreased significantly as compared with those recorded preoperatively. The postoperative ODI scores were lower than those recorded preoperatively. MacNab criteria rating excellent, good and fair results were in 27, 37 and 10 patients, respectively. Conclusion: PELD, MIS-TLIF CTS, and MIS-TLIF BPS are all effective minimally invasive techniques for the therapy of single segment far lateral lumbar disc herniation in middle-aged and elderly patients. PELD had a shorter operation time and less surgical trauma, being a less invasive and more economical method; however, there was no recurrence of disc herniation after fixation. Compared with MIS-TLIF BPS, MIS-TLIF CTS obtained a similar clinical effect and certain costs were saved.
Introduction
With the development of society and improvements in medical technology, the aging population is becoming increasingly apparent [Citation1]. The facet joints and intervertebral discs play an important role in maintaining exercise in old age. Lumbar and lower extremity pain in middle-aged and elderly patients has been shown to mainly originate from lumbar disc herniation [Citation2]. The far lateral lumbar disc herniation (FLDH) accounts for 0.7–11% of all disc herniation [Citation3].The prolapsed disc often compresses the exiting root and ganglion, leading to severe radicular pain. The traditional posterior midline approach, paraspinal and endoscopic approaches are common surgical approaches for FLDH [Citation4]. Typically, the minimally invasive paraspinal approaches not only minimize the damage to soft tissue, lamina, but also directly expose the far lateral protruding disc [Citation5, Citation6]. As a result of its minimal surgical trauma, paraspinal lateral surgeries such as PELD, MIS-TLIF CTS, and MIS-TLIF BPS have been widely used in recent years [Citation7, Citation8]; however, the surgical comparison of these three approaches in middle-aged and elderly patients with far lateral disc herniation is still lacking. The purpose of this study is to examine the necessity of internal fixation and compare the clinical results of different minimally invasive approaches for treatment of FLDH in middle-aged and elderly patients.
Materials and methods
Data were collected from consecutive patients treated by surgery at the General Hospital of Shenyang Military Region between March 2010 and December 2016. The enrolled criteria were illustrated below: patients who (1) had one segment far lateral disc herniation, lower extremity symptoms, and lower back pain; (2) demonstrted not relieving or aggravating after 3 months of conservative treatment; (3) presented with symptoms that were consistent with single segment lumbar disc herniation on MRI and/or CT. The criteria of exclusion were illustrated below: patients who (1) had multi-segment lumbar intervertebral disc herniation; (2) had undergone spinal surgery; or (3) had a history of fractures, tumors, infections, or other spinal diseases. These patients corresponded to 4.6% of those who experienced lumbar disc surgery at that time. Forty-one patients were men and 33 were women, aged between 57 and 82 years old (mean 63.3). There were 26 cases in L5/S1 level, 32 in L4/5 level, 15 in L3/4 level, and 1 in L2/3 level. Comorbidities included coronary heart disease, diabetes, and tobacco use(Table 1). Clinical data included the length of the incision, duration of operation, estimated blood loss, hospitalization time, operation cost, recurrence rate, and fusion rate. Outcomes included the VAS score for LBP and LP and the ODI score preoperatively and at 1-week and 12-months postoperatively, which were defined as excellent, good, fair or poor based on the MacNab criteria. The study was approved by the Ethics Committee of the General Hospital of Shenyang Military Region.
Table 1. Patient baseline characteristics.
Surgical techniques
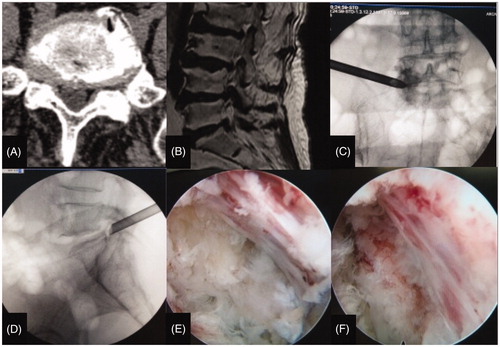
The PELD group
The PELD was performed under local anesthesia in the prone position. Firstly, location of body surface incision was guided by C-arm, and a 0.7-mm guiding wire was inserted via the anaesthetic puncture needle. A double-channel eccentric guide rod with an outer diameter of 6 mm was placed toward the prolapse, and the dilator was inserted into the extraforaminal lumbar disc herniation. An inner diameter of 6.5 mm surgical working tube with a beveled opening was then pushed ventrally over the dilatator to protect the nerve roots. The beveled opening of the tube was adjusted and pushed toward the prolapse. Secondly, nerve root decompression was performed under gravity-controlled liquid flow and visual control. In addition, a high frequency semi-active flexible bipolar probes were used for coagulation hemostasis and soft tissue formation(Figure 1).
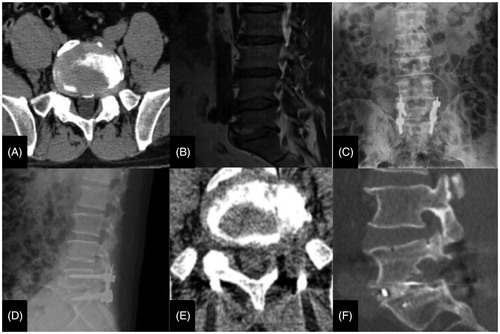
The MIS-TLIF CTS group
Patients received general anesthesia in the prone position, and the localization of target segment was guided by preoperative C-arm which parallel to the upper end plate. A 30-mm vertical skin incision was performed approximately 1–2 cm lateral to the midline of the spine, followed by transmuscular dilatation between the polyfissure and longissimus muscles. The working channel was inclined approximately 5–10° toward the disc space to localize the disc prolapse (21). The surgical methods were as follows: decompression, excision of the articular process and part of the yellow ligament; exposure of the exiting nerve root; opening the exiting nerve root canal; discectomy; end plate treatment; and intervertebral bone graft and cage implantation. The ipsilateral pedicle screws were positioned directly. For the purpose to keep the balance of spine, the translaminar screw was placed along the base of the superior spinous process and contralateral lamina to opposite facet joint(Figure 2).
The MIS-TLIF BPS group
Patients underwent the similar surgical procedures, and the contralateral percutaneous pedicle screws were inserted under the guidance of a C arm(Figure 3).
Statistical analysis
SPSS 19.0 was used for statistical analysis. The comparison was demonstrated as follows: homogeneity of variance and normal distribution using an independent sample t-test, and variance of arrhythmia and normal distribution using a t-test. Attribute data were analyzed with χ2 test. A p value < .05 was considered statistically significant.
Results
The mean follow-up time was 26.4 months (range from 14 to 46 months). The three groups had equivalent average age, gender distribution, level distribution, and comorbidities. Compared with the internal fixation groups, the length of the incision, duration of operation, estimated blood loss, and hospitalization time were obviously lower (p < .05) in the PELD group. The difference in operation cost was statistically significant; PELD was the least, followed by MIS-TLIF CTS, and then MIS-TLIF BPS(Table 2). The postoperative VAS scores for LBP and LP decreased significantly as compared with those recorded preoperatively. The postoperative ODI scores were lower than those recorded preoperatively (p < .05), with the postoperative LBP in the PELD group being significantly lower than others. In addition, there was no significant difference in the ODI or VAS scores according to MacNab criteria among the three groups postoperatively (p > .05). MacNab criteria rating excellent, good and fair results were in 27, 37 and 10 patients, respectively(Table 3).
The PELD group had two cases of postoperative recurrence, and the other two groups had no recurrence; however, there was no significant difference (p > .05). There was also no significant difference in the fusion rate at 1-year follow-up between the two groups with internal fixations. Incision infection occurred in 2 cases in all three groups, but no other complications occurred.
Discussion
Far lateral disc herniation (FLDH) is also known as foraminal, intraforaminal, or extreme lateral disc herniation, which is defined as a disc herniation or prolapse that resides lateral and beneath to the upper and lower pedicles and compresses the exiting root and ganglion [Citation10, Citation11]. FLDH rarely causes compression of the dural sac, cauda equina and dysfunction of the bowel and bladder. In the current research, the average patient age was 63.3 years old (range from 57 to 82), which is consistent with that in previous studies [Citation11] and shows that FLDH predominately occurs in middle-aged and elderly patients. Although conservative treatment can occasionally be effective, surgery is usually required [Citation12]. Various surgical approaches have been performed for the operative treatment of FLDH. With the improvement and popularity of minimally invasive spine technology, PELD, MIS-TLIF CTS, and MIS-TLIF BPS have become widely used as ameliorative treatments [Citation13]. Compared with traditional midline approaches, these three minimally invasive techniques are implemented with a mini-incision, require smaller muscle soft tissue dissection, supraspinal interspinous ligaments and spinous process are retained. One previous study reported that PELD has shown comparable results to the standard surgery [Citation14]; however, another study reported that PELD in elderly patients had a higher reoperation rate during the first 3.4 years of follow-up than traditional discectomy [Citation15]. Due to this discrepancy, the present study compared the clinical results of PELD, MIS-TLIF CTS, and MIS-TLIF BPS for the treatment of FLDH in middle-aged and elderly patients and examined the necessity of internal fixations. For elderly patients with severe osteoporosis or other diseases, who could not tolerate general anesthesia, we used PELD to remove the prolapse under local anesthesia. Those complicated with degenerative instability, spondylolisthesis, isthmus, or giant disc calcification, we performed MIS-TLIF CTS or MIS-TLIF BPS.
In the present study, the length of the incision, duration of the operation, estimated blood loss, and hospitalization time in the PELD group were apparently lower than other groups, reflecting that PELD for patients with FLDH has a lot of advantages. Recent studies have also documented good results by PELD for FLDH [Citation16]. Lower blood loss and a shorter operation time appear to be the benefits of a PELD surgical approach, resulting in little soft tissue damage due to the gravity-controlled liquid flow and the application of high frequency semi-active flexible bipolar probes. Guiding by lens optics under controlled liquid not only enables clear visual environment but also reduces hemorrhage. The bipolar probes can be applied in the immediate vicinity of neural structures and avoid intraoperative bleeding [Citation17]. Patients with FLDH who undergo PELD can recover faster and walk down early. The reasons are as follows: (1) faster recovery of lower waist soft tissue after PELD with little tissue resection and almost no injury to the bony structure helps to strengthen the waist and enable earlier occupational and athletic levels of activity; (2) less trauma reduces the theoretical probability of poor wound healing and fat liquefaction as compared with traditional surgery; and (3) rehabilitative measures are not necessary. Kambin et al. reported that a few patients presented with postoperative hip or leg causalgia secondary to immature operation of the dorsal root ganglion; however, no patients experienced causalgia in the present study and the clinical effect was satisfactory. As for the reasons; exact preoperative measurement is necessary and the manipulation of PELD has a prolonged learning curve. Firstly, in most patients presented with FLDH, the outreaching angle and the distance between the incision and the midline needs to be measured. The purpose was to make possible tangential reaching of the sagittal and coronal localization of the prolapse. Secondly, the recognition of the shape and orientation of the disc, ligaments, nerve, and vessels plays a vital role in the endoscopic environment; and continuing improvement of endoscopic instruments enables a wider and more efficient decompression than ever. Thirdly, the degree of intraoperative decompression mainly depends on the range of the fluid-controlled nerve root motion and the patients' expression of leg pain relief. As a result, adequate exposure and decompression could be obtained and causalgia was avoided.
The difference in cost among the three groups was statistically significant. The main reason for the lower cost of PELD is that the surgery is performed under local anesthesia and does not implant internal fixations. The appraisal of the spend of internal fixtures demonstrated that the application of MIS-TLIF CTS for one level fusion increased the spend by nearly 20% as compared with PELD. In terms of cost savings, a shorter hospitalization time also played a key role.
The present data show that the postoperative VAS scores for LBP and LP decreased significantly compared with those recorded preoperatively; and all three minimally invasive operations had reduced VAS scores at 1-week and 12-months post-surgery. Postoperative LBP in the PELD was significantly lower than the others.
In terms of neurofunctional recovery, the postoperative ODI scores were significantly lower than those recorded preoperatively, indicating that minimally invasive surgeries can restore nerve function and provide relief from the radiating pain. In the present study, endoscopic decompression, nucleus pulposus excision, and decompression of the exiting nerve root canal in the PELD group were similar to the procedures in the MIS-TLIF CTS and MIS-TLIF BPS groups.
Moreover, there were no statistically differences in MacNab criteria and postoperative ODI scores among the three groups, demonstrating that the function of these approaches in the therapy of middle-aged and elderly patients with FLDH is relatively comparable.
The main goal of the implant is to fix the spine and ensure bone graft fusion; thus, the fusion rate is the most important index to evaluate. Bridwell et al., introduced the four grading criteria of radiographic fusion [Citation18]; both grades I and II are considered radiographic signs of solid fusion. Previous studies have showed that postoperatively scoliosis occurs more frequently in unilateral than bilateral groups [Citation19]; however, the scoliotic patients did not have obvious clinical symptoms in recent researches. To avoid the occurrence of scoliotic deformities, the patients with FLDH were treated with MIS-TLIF CTS or MIS-TLIF BPS. Although there exists a difference in the operation cost, the difference of fusion rate was not significantly different between the two groups at 1-year follow-up. Best NM et al., also reported that there were no apparent differences in range of motion, fixation stiffness, or multi-directional activities between the combination of unilateral pedicle screws and the translaminar screw and bilateral pedicle screw fixation [Citation20].
The PELD group had two cases of postoperative recurrence, which were revised by MIS-TLIF CTS; nevertheless, the difference in the recurrence rate was not statistically significant. However, there was no recurrence of disc herniation after internal fixations. There were two cases of incision infection in all three groups, which were cured by conservative treatment.
There were many limitations in the current study. Firstly, this is a retrospective study with a small sample size; an additional multicenter and prospective study with a larger sample is needed. Secondly, patient selection has some limitations; multifocal lumbar disc herniation needs further research. Thirdly, the included studies were short- or medium-term. Long-term follow-up periods of the three methods should be evaluated in the future.
Conclusion
PELD, MIS-TLIF CTS, and MIS-TLIF BPS were all effective minimally invasive methods for the therapy of single segment far lateral lumbar disc herniation in middle-aged and elderly patients. PELD had a shorter operation time and less surgical trauma, being a less invasive and more economical method; however, there was no recurrence of disc herniation after fixation. Compared with MIS-TLIF BPS, MIS-TLIF CTS obtained a similar clinical effect and certain costs were saved.
Table 2. Surgical outcomes.
Table 3. Pre- and postoperative LP VAS score, ODI score and Macnab criteria assessment.
Additional information
Funding
References
- The World Population Prospects. 2015 Revision.at <http://esa.un.org/unpd/wpp/Publications/Files/Key_Findings_WPP_2015.pdf>
- Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol. 2007;213:626–634.
- Kim DG, Eun JP, Park JS. New diagnostic tool for far lateral lumbar disc herniation: The clinical usefulness of 3-Tesla magnetic resonance myelography comparing with the discography CT. J Korean Neurosurg Soc. 2012;52:103–106.
- Blamoutier A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res. 2013;99:S187–S196.
- Quaglietta P, Cassitto D, Corriero AS, et al. Paraspinal approach to the far lateral disc herniations: retrospective study on 42 cases. Acta Neurochir. 2005;92:115–119.
- Lee JS, Woo JY, Jang JS, et al. Combined interlaminar and paraisthmic approach for co-existing intracanal and foraminal lesion. Korean J Spine. 2015;12:256–260.
- Sethi A, Lee S, Vaidya R. Transforaminal lumbar interbody fusion using unilateral pedicle screws and a translaminar screw. Eur Spine J. 2009;18:430–434.
- Wang Y-P, An J-L, Sun Y-P, et al. Comparison of outcomes between minimally invasive transforaminal lumbar interbody fusion and traditional posterior lumbar intervertebral fusion in obese patients with lumbar disk prolapse. Tcrm. 2017;13:87–94.
- Al-Khawaja DO, Mahasneh T, Li JC, et al. Surgical treatment of far lateral lumbar disc herniation: a safe and simple approach. J Spine Surg. 2016;2:21–24.
- Yue JJ, Scott DL, Han X, et al. The surgical treatment of single level multi-focal subarticular and paracentral and/or far-lateral lumbar disc herniations: the single incision full endoscopic approach. Int J Spine Surg. 2014;8:16.
- Phan K, Dunn AE, Rao PJ, et al. Far lateral microdiscectomy: a minimally-invasive surgical technique for the treatment of far lateral lumbar disc herniation. J Spine Surg. 2016;2:59–63.
- O’Toole JE, Eichholz KM, Fessler RG. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction: cadaveric dissection and technical case report. Spine J. 2007;7:414–421.
- Ruetten S, Komp M, Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach–technique and prospective results of 463 patients. Spine 2005;30:2570–2578.
- Kim CH, Chung CK, Park CS, et al. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine 2013;38:581–590.
- Kim CH, Chung C, Choi KY, et al. The selection of open or percutaneous endoscopic lumbar discectomy according to an age cut-off point: national-wide cohort study. Spine 2015;40:E1063–E1070.
- Jang JS, An SH, Lee SH. Transforaminal percutaneous endoscopic discectomy in the treatment of foraminal and extraforaminal lumbar disc herniations. J Spinal Disord Tech. 2006;19:338–343.
- Ruetten S, Meyer O, Godolias G. Application of holmium:YAG laser in epiduroscopy: extended practicabilities in the treatment of chronic back pain syndrome. J Clin Laser Med Surg. 2002;20:203–206.
- Bridwell KH, Lenke LG, McEnery KW, et al. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 1995;20:1410–1418.
- Wang L, Wang Y, Li Z, et al. Unilateral versus bilateral pedicle screw fixation of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF): a meta-analysis of randomized controlled trials. BMC Surg. 2014;14:87.
- Best NM, Sasso RC. Efficacy of translaminar facet screw fixation in circumferential interbody fusions as compared to pedicle screw fixation. J Spinal Disord Tech. 2006;19:98–103.
- Ikuta K, Tono O, Senba H, et al. Translaminar microendoscopic herniotomy for cranially migrated lumbar disc herniations encroaching on the exiting nerve root in the preforaminal and foraminal zones. Asian Spine J. 2013;7:190–195.