Abstract
Purpose
Due to the high perforation rate of cervical pedicle screw placement, we have designed four different types of rapid prototyping navigation templates to enhance the accuracy of cervical pedicle screw placement.
Methods
Fifteen human cadaveric cervical spines from C2 to C7 were randomly divided into five groups, with three specimens in each group. The diameter of pedicle screw used in this study was 3.5 mm. Groups 1–4 were assisted by the two-level template, one-level bilateral template, one-level unilateral template and one-level point-contact template, respectively. Group 5 was without any navigation template. After the surgery, the accuracy of screw placement in the five groups was evaluated using postoperative computed tomographic scans to observe whether the screw breached the pedicle cortex.
Results
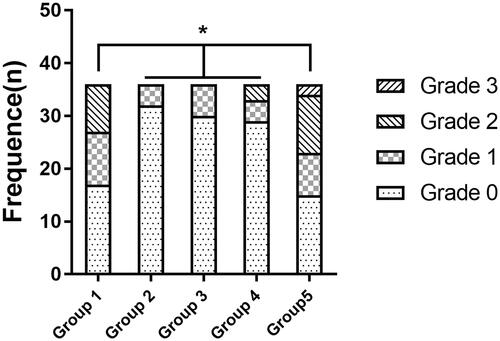
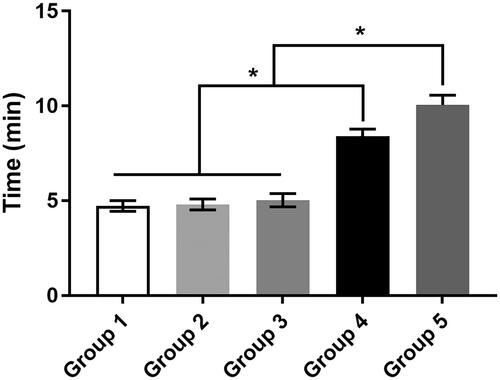
A total of 180 pedicle screws were inserted without any accidents. The accuracy rate was 75%, 100%, 100%, 91.7%, and 63.9%, respectively, from Groups 1 to 5. All the template groups were significantly higher than Group 5, though the two-level navigation template group was significantly lower than the other three template groups. The operation time was 4.72 ± 0.28, 4.81 ± 0.29, 5.03 ± 0.35, 8.42 ± 0.36, and 10.05 ± 0.52 min, respectively, from Groups 1 to 5. The no template and point-contact procedures were significantly more time-consuming than the template procedures.
Conclusion
This study demonstrated that four different design types of navigation templates achieved a higher accuracy in assisting cervical pedicle screw placement than no template insertion. However, the two-level template’s accuracy was the lowest compared to the other three templates. Meanwhile, these templates avoided fluoroscopy during the surgery and decreased the operation time. It is always very challenging to translate cadaveric studies to clinical practice. Hence, the one-level bilateral, unilateral, and point-contact navigation templates designed by us need to be meticulously tested to verify their accuracy and safety.
Introduction
The placement of cervical pedicle screw has become a useful surgical procedure for spinal fixation in many instances because of its major biomechanical advantages and high fusion rate [Citation1–5]. However, medial and lateral breach of the pedicle screw from the cortical bone occurs frequently, leading to a high perforation rate of the pedicle screw, which can cause severe complications such as neurovascular injury [Citation6–8]. This is mainly due to the variation of anatomical structures and the small size of pedicle [Citation7,Citation9]. Hence, the clinical application of pedicle screw placement has been limited. There are a few methods to improve the accuracy of pedicle screw placement, which includes rapid prototyping navigation template (RPNT) [Citation10–24]. The RPNT was created two decades ago to enhance the accuracy of screw placement in vitro and in vivo. In comparison with the traditional methods, the RPNT was found to significantly improve the accuracy of pedicle screw implantation [Citation11,Citation16,Citation19,Citation21–24]. However, different designs of RPNTs were used in different studies, and these templates have not been compared with each other for enhancing the accuracy of pedicle screw insertion.
In current study, we designed four different types of navigation template to assess their accuracy in assisting cervical pedicle screw placement. The following procedures were performed: (1) Design a patient-specific navigation template by medical image processing software and reverse engineering software. (2) Fabricate navigation template model using 3D printing technology. (3) Verify the accuracy of four different types of navigation templates in assisting cervical pedicle screw insertion through cadaveric study to guide clinical applications.
Materials and methods
Specimens
A total of 15 formalin-fixed cadaveric cervical spine specimens (average donor age: 60.5 ± 11.8 years; 8 males and 8 females) including C2–C7 were obtained from the Department of Anatomy and Histology of Xi’an Jiaotong University. All the specimens were examined with computed tomography (CT) scans to exclude tumors, fractures, and other bone structure defects.
Study design
The 15 cadavers were equally divided into five groups. Group 1 (n = 3): the procedure was performed assisted by the two-level navigation template. Group 2 (n = 3): the procedure was implemented assisted by the one-level bilateral template. Group 3 (n = 3): the operation was performed assisted by the one-level unilateral template. Group 4 (n = 3): the operation was conducted with the help of the one-level point-contact template. Group 5 (n = 3): the surgery was performed without any template. All the pedicles of C2–C7 were inserted with titanium pedicle screws, with a diameter of 3.5 mm.
Preparation of template
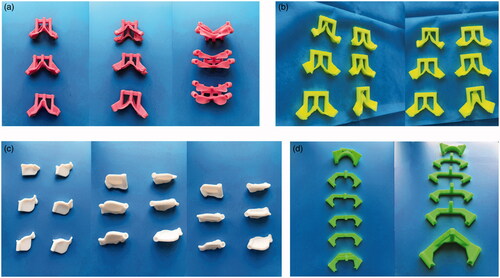
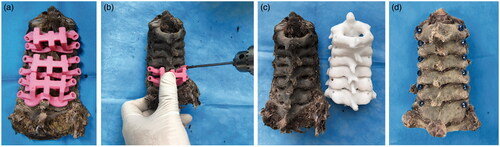
CT scans with a thickness of 0.625 mm were obtained of all specimens and stored as digital imaging and communications in medicine (DICOM) format. Then they were imported into the medical image processing software Mimics 17.0 (Materialise, Leuven, Belgium) to develop 3D reconstruction models of C2–C7 (). Besides, a cylinder with a diameter of 3.5 mm was also constructed with the tool of ‘MedCAD’ to simulate pedicle screws.
Figure 1. The construction workflow of rapid prototyping navigation template. (a) The coronal and sagittal plane of 3D models of C2–C7. (b) The confirmation of C2 channels to ensure that pedicle screw pass through the center of pedicle without penetrating the cortical bone. (c) The design of navigation template of C2 via the location of screw channels. (d) The confirmation of C3–C7 pedicle screw channels. (e) The design of navigation template of C3–C7 via the location of corresponding screw channels. (f) The physical navigation template and vertebra model.
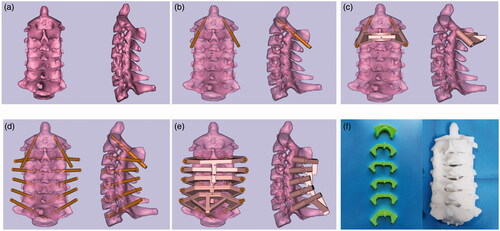
The 3D model of these cervical vertebrae and cylinder were exported in stereolithography format into Geomagic Studio 12 (Geomagic, Cary, NC), a reverse engineering software that was used to determine the optimal entry point and direction of pedicle screw. The rapid prototyping navigation template is designed to completely fit the posterior surface such as lamina and spinous process of the corresponding vertebral body (). Then the physical navigation template and vertebrae models were manufactured using a fused deposition modeling (FDM) 3D printer (Waston, Changzhou, China) (). The navigation template consists of two parts, one part of the template, attach to the posterior vertebrae fitfully, has a thickness of 2.5 mm to ensure sufficient strength, and another part is called hollow orienting guide tube, which is used to confirm the screw entry point and orientation of pedicle screw. In this study, we designed and constructed four different types of navigation templates ().
Surgery
Before pedicle screw insertion, the soft tissues on the spinous process and lamina of all vertebrae from the five groups were removed to completely expose the posterior bony surface and facilitate a lock-and-fit relationship between the template and the posterior bony surfaces. Then all the surgeries were performed in the anatomy laboratory by a well-experienced surgeon. Specimens were maintained in a prone position on the operating table. The four different types of templates were applied in the four groups. First, the RPNT was stably and properly placed on the corresponding bony surface. Then a high-speed 3.2 mm drill bit was used to drill the trajectory of pedicle screw along the pre-designed cannulated orienting guide tube on both sides. Finally, after creating all the screw trajectories and removing the template, a hand drill was used to carefully insert the 3.5 mm pedicle screw into the drilled hole trajectory. The pedicle screws of Group 5 were inserted according to the anatomic marks. In the Group 1, the two-level RPNT was attached to C2–C3, C4–C5, and C6-C7, respectively. The average operation time was recorded during the surgery, from the time the surgeon began to place the RPNT on the posterior bony surface to the time the four screws were placed into every adjacent two-level vertebrae ().
Figure 3. The surgical procedure of pedicle screw insertion with the assistance of rapid prototyping navigation template. (a) The navigation templates fit closely to the posterior surface of corresponding vertebral body. (b) A high-speed drill bit was used to drill channels through navigation template. (c) The cervical specimen and corresponding physical vertebra model. (d) Pedicle screw insertion into the cervical specimen through designed screw channels.
Assessment of navigation template accuracy
After all the pedicle screws were inserted into the corresponding vertebrae, postoperative CT scans were obtained to assess the position of pedicle screws with four different types of RPNTs. The accuracy was assessed by two experienced doctors who were not involved with the surgery. Any disagreement was resolved by a third doctor to decide the final result. We evaluated the accuracy of pedicle screws from C2 to C7 with the following grading system [Citation19]. An axial imaging was obtained and the deviation of screws were classified as four grades: Grade 0: the screw was completely within the cortex of the pedicle. Grade 1: the screw perforated the cortex of the vertebrae by less than 2 mm or less than half the screw diameter. Grade 2: the screw breached the cortical bone of the corresponding vertebrae by more than 2 mm but less than 4 mm or half the screw diameter. Grade 3: the screw deviated more than 4 mm or entirely penetrated the cortex of the bone structure. Grades 0 and 1 were considered to be safe placement since major part of the screws remained in the cortical bone, with no harm to adjacent nerves and vessels. The pedicle screw perforation more than 2 mm or half screw diameter was considered to cause neurological and vascular injuries, and Grade 2 or Grade 3 were regarded as critical perforations [Citation3,Citation25–27].
Statistical methods
Statistical analysis was performed with SPSS version 20.0 software (SPSS, Chicago, IL). The Kruskal–Wallis H test was used to analyze the differences in pedicle screw placement accuracy among five different types RPNT groups. The operation time data was presented as the mean ± SD and was assessed with one-way analysis of variance (ANOVA). p Value of less than 0.05 represented statistical significance.
Results
In the Group 1, a total of 36 pedicle screws were placed into the corresponding vertebrae from C2–C7 with the assistance of two-level navigation template. Of these, 17 screws (47.2%) were completely inside the pedicle and were classified as Grade 0, 10 screws (27.8%) were classified as Grade 1, 9 screws (25%) mostly perforated the pedicle and were classified as Grade 2, and no screws were classified as Grade 3. In the Group 2, assisted by the one-level bilateral template, totally 36 pedicle screws were inserted into the targeted vertebrae. Of these, 32 screws (88.9%) were classified as Grade 0, four screws (11.1%) partially breached outside the pedicle and were classified as Grade 1, and no screws were classified as Grade 2 or 3. In the Group 3, with the help of one-level unilateral template, 36 pedicle screws were implanted into the vertebral body. Of these, 30 (83.3%) and 6 screws (16.7%) were classified as Grades 0 and 1, respectively, while no screws were classified as Grade 2 or 3. In the Group 4, 36 pedicle screws were placed into the vertebrae with the aid of one-level point-contact template. Of these, 29 (80.6%) and 4 screws (11.1%) were considered as Grade 0 and 1, 3 screws (8.3%) were regarded as Grade 2, and no screws were classified as Grade 3. In the Group 5, without any template assistance, 15 (41.7%) and 8 screws (22.2%) were classified as Grade 0 and 1, 11 screws (30.6%) were regarded as Grade 2, and 2 screws (5.5%) were classified as Grade 3 ( and ). However, the results showed significant differences among the five groups. Inter-group comparison indicated that the accuracy rate of the no template group was significantly lower than the four template groups. Moreover, the accuracy rates of the other three groups were significantly higher compared with the two-level navigation template group ().
Table 1. Number of pedicle screws perforation and accuracy of screw placement among five groups.
The average operation time for every two-level screw insertion in the no template group was 10.05 ± 0.52 min, which was significantly longer than the template groups, in which the operation time was 4.72 ± 0.28, 4.81 ± 0.29, 5.03 ± 0.35, and 8.42 ± 0.36 min from Group 1 to Group 4, respectively. However, the one-level point-contact navigation template procedure was significantly more time-consuming than the other three template procedures ( and ).
Table 2. The comparison of operation time among four different types of rapid prototyping navigation template groups and no template group.
Illustrative cases
Case 1
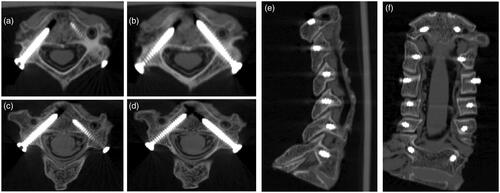
The surgery was performed with the assistance of the one-level bilateral navigation template in a 58-year-old male cervical cadaver specimen. After soft tissues attached to the posterior lamina and spinous were removed, the surgeon inserted pedicle screws from C2 to C7 with the help of the matched one-level bilateral navigation template. After all screws were placed, the postoperative CT scans were carried out to assess the screw positions and evaluate the accuracy. The outcomes showed that the positions of the screws were classified as Grade 0 or 1 ().
Figure 6. Postoperative CT scan showed positions of cervical pedicle screws with the assistance of one-level bilateral navigation template. (a and b) C4 pedicle screws classified as Grade 0 (axial plane). (c and d) C3 pedicle screws classified as Grade 0 (right) and Grade 1 (left) (axial plane). (e_ C2–C7 pedicle screws from sagittal plane. (f) C2–C7 pedicle screws from coronal plane.
Case 2
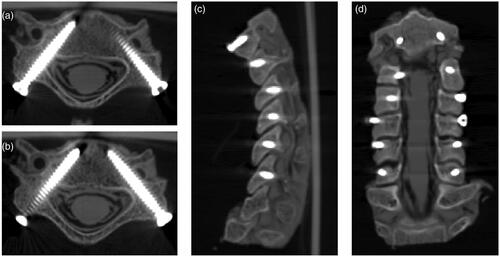
The surgery was performed with the assistance of the two-level navigation template in a 63-year-old female cervical cadaver specimen. After the bony structure of the posterior lamina and spinous were exposed, the surgeon inserted the pedicle screws from C2 to C3, C4 to C5, and C6 to C7 assisted by the corresponding two-level templates. The postoperative CT scans were implemented to assess the screw positions and estimate the accuracy after all screws were inserted. The CT images showed that some of the screw positions were classified as Grade 2 ().
Figure 7. Postoperative CT scan showed positions of cervical pedicle screws with the assistance of two-level navigation template. (a) C5 pedicle screws classified as Grade 2 (left) (axial plane). (b) C5 pedicle screws classified as Grade 0 (right) (axial plane). (c) C2–C7 pedicle screws from sagittal plane. (d) C2–C7 pedicle screws from coronal plane.
Discussion
Posterior internal fixation surgery has been proven to be a reliable cervical spine fusion surgery to treat degenerative cervical diseases. Studies have testified that screw fixation, particularly using pedicle screws, is the most credible method to guarantee the fixation and stabilization of corresponding spinal segments in the cervical vertebrae [Citation2,Citation4,Citation28]. However, because of the anatomic variations and small size of pedicle, the malposition rate of pedicle screws was high, which posed a great risk to adjacent nerves and blood vessels [Citation6]. Hence, it is critical to avoid such neurovascular complications and improve pedicle screw placement accuracy.
In the past several decades, a few methods have been used to achieve accurate cervical pedicle screw insertion, including anatomic landmarks, image-guided technology, and computer-assisted surgery systems. Besides, a new technology called rapid prototyping navigation template (RPNT) was first used in hip and knee surgeries, and was subsequently introduced in posterior cervical surgeries. The RPNT has been proven to improve the accuracy in assisting cervical pedicle screw insertion [Citation10–24,Citation29]. In 2001, Goffin et al. [Citation10] designed a three-dimensional computed tomography-based personalized drill guide for posterior cervical fusion at C1-C2 using rapid prototyping technology. These types of templates were designed to connect only to lamina, or lamina and spinous process. Subsequently, Berry et al. [Citation11] developed a personalized imaged-based template for intra-operative guidance in a cadaveric study. They designed four types of templates, which were in contact with several points on the posterior side of the spine. These types of templates [Citation10,Citation11] were similar to the one level point-contact template designed by us, but our template is comparatively concise and more accurate than theirs. Ryken et al. [Citation15] and Kawaguchi et al. [Citation27] developed a template that covered only one side of the bone structure in cadaveric and clinical applications, respectively. Similar to our one-level unilateral template, the accuracy rate of the screw placement was very high. Lu et al. [Citation13,Citation16] and Hu et al. [Citation18] introduced a template that covered two sides of the corresponding posterior cervical vertebra in cadaveric and clinical studies. Their screw insertion accuracy rate was high, ranging from 96.6% to 100% [Citation13,Citation16,Citation18], which was similar to the accuracy rate of our one-level bilateral template. Recently, Merc et al. [Citation30] designed a multi-level rapid prototyping template for pedicle screw placement in lumbar and sacral spine, and their results indicated that the screw placement error rate was up to 26%, which was similar to our two-level navigation template in which the screw placement accuracy rate was 75%. The accuracy of our four different types of navigation templates was higher than the no template group, indicating that navigation templates improve the accuracy of pedicle screw insertion. However, the accuracy of the two-level navigation template was much lower than the other three types of templates, mainly because the contact areas between the navigation template and the dorsal parts of the cervical vertebra was preoperatively designed, and any relative movement between two adjacent vertebrae could cause the entry point and screw tunnel to deviate from the pre-designed contact areas. The dorsal muscle of the vertebrae was removed before surgery, so the vertebra could easily shift relatively when we impose a pressure on the template. D’Urso et al. [Citation31] suggested that templates fitted to the dorsal elements of only one vertebra were more accurate. Although the accuracy showed no significant difference among the other three types of template, three pedicle screws were considered as Grade 2 in the one-level point-contact navigation template group, whereas the screws in the other groups were all assessed as Grade 0 or 1 in our study. During the surgery, we imposed a fixed force to the point-contact template to prevent displacement of template during drilling. However, misplacement still occurred, indicating that one-level point-contact template is not as stable as the other two types of templates. However, we do not have to remove all the muscles on the dorsal parts of the vertebrae for this type of template, because the template is only in contact with the spinous process and other points. Although the accuracy of one-level bilateral and unilateral navigation template groups was similar, we took a longer time to design and manufacture the unilateral template.
Our results showed that the average operation time among the five groups was different, the operation in the point-contact navigation template group was significantly more time-consuming than in the other three template groups, mainly due to the less contact area between the template and the bone structure, which required more time to fix the template to the specific points and prevent the template from shifting. We also set up a group using traditional no template method to place the cervical pedicle screw according to certain anatomic marks, and the operation time in that group was significantly longer than the template groups, mainly because it took time to locate the entry point. Some studies [Citation13,Citation19,Citation25] have demonstrated that the application of navigation template decreased the operation time compared to the traditional method, because when using traditional method for screw insertion, surgeons need to use intra-operative X-rays to assess the position of screws and adjust the screw tunnel to avoid perforating the pedicle, which increases the operation time as well as the radiation exposure to the surgeon and patient [Citation25]. Our navigation templates avoided these tedious steps and simplified the surgical process.
The cost of our proposed navigation templates is about $50 per segment, which is much cheaper than standard navigation system. The accuracy of screw placement of our navigation templates and standard navigation system are both higher than conventional methods like free-hand and two-dimensional image guide. The intraoperative use of standard navigation system significantly reduces the screw malposition rate. According to a peer-review report [Citation32], about 52–73% surgeons refused to use standard navigation system, they prefer conventional methods. Compared with our navigation template, the standard navigation system has some defects. First of all, the learning curve of using our techniques is much shorter than navigation system. Second, the use of navigation system increased the intraoperative time, the surgeon needs to match the spinal position with CT image reconstruction. Finally, if relative position of the adjacent vertebrae has been moved, it may influence the accuracy of screw placement. These factors restrict the use of standard navigation system and our proposed navigation templates are worth promoting.
Although we designed four different types of navigation templates, this technique had some limitations. First, the workflow of template construction was complicated. The design and fabrication of a template is time-consuming and requires 1–7 days [Citation10,Citation13,Citation16,Citation18], so it cannot be used in emergency surgery. Second, this technique requires complete clearance of posterior parts of the vertebrae, including muscles and fat tissues, which may cause damage to the patient. Third, the surgeons need to be proficient in the related software and surgical skills, which requires a long learning curve. Given these limitations, this technique needs to be urgently improved in the near future.
Conclusion
This study compared the accuracy of four different types of navigation templates and demonstrated that except the two-level navigation template, the other three types of navigation templates achieved a high accuracy in assisting cervical pedicle screw placement. They all showed a higher accuracy than the no template group. Besides, the operation time was shortened and fluoroscopy was avoided during the surgery. However, it is always very challenging to translate cadaveric studies to clinical practice, so the one-level bilateral, unilateral and point-contact navigation templates designed by us need further verification of their accuracy and safety.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Hojo Y, Ito M, Suda K, et al. A multicenter study on accuracy and complications of freehand placement of cervical pedicle screws under lateral fluoroscopy in different pathological conditions: CT-based evaluation of more than 1,000 screws. Eur Spine J. 2014;23(10):2166–2174.
- Barnes AH, Eguizabal JA, Acosta FJ, et al. Biomechanical pullout strength and stability of the cervical artificial pedicle screw. Spine (Phila, PA, 1976). 2009;34(1):E16–E20.
- Yukawa Y, Kato F, Yoshihara H, et al. Cervical pedicle screw fixation in 100 cases of unstable cervical injuries: pedicle axis views obtained using fluoroscopy. SPI. 2006;5(6):488–493.
- Kothe R, Ruther W, Schneider E, et al. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine (Phila, PA, 1976). 2004;29(17):1869–1875.
- Abumi K, Takada T, Shono Y, et al. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine (Phila, PA, 1976). 1999;24(14):1425–1434.
- Abumi K, Shono Y, Ito M, et al. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila, PA, 1976). 2000;25(8):962–969.
- Yukawa Y, Kato F, Ito K, et al. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2009;18(9):1293–1299.
- Odgers CT, Vaccaro AR, Pollack ME, et al. Accuracy of pedicle screw placement with the assistance of lateral plain radiography. J Spinal Disord. 1996;9(4):334–338.
- Tian W, Liu Y, Zheng S, et al. Accuracy of lower cervical pedicle screw placement with assistance of distinct navigation systems: a human cadaveric study. Eur Spine J. 2013;22(1):148–155.
- Goffin J, Van Brussel K, Martens K, et al. Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1-C2. Spine (Phila, PA, 1976). 2001;26(12):1343–1347.
- Berry E, Cuppone M, Porada S, et al. Personalised image-based templates for intra-operative guidance. Proc Inst Mech Eng H. 2005;219(2):111–118.
- Owen BD, Christensen GE, Reinhardt JM, et al. Rapid prototype patient-specific drill template for cervical pedicle screw placement. Comput Aided Surg. 2007;12(5):303–308.
- Lu S, Xu YQ, Lu WW, et al. A novel patient-specific navigational template for cervical pedicle screw placement. Spine (Phila, PA, 1976). 2009;34(26):E959–E966.
- Lu S, Xu YQ, Zhang YZ, et al. A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J. 2009;18(9):1379–1385.
- Ryken TC, Owen BD, Christensen GE, et al. Image-based drill templates for cervical pedicle screw placement. SPI. 2009;10(1):21–26.
- Lu S, Xu YQ, Chen GP, et al. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg. 2011;16(5):240–248.
- Hu Y, Yuan ZS, Spiker WR, et al. Deviation analysis of C2 translaminar screw placement assisted by a novel rapid prototyping drill template: a cadaveric study. Eur Spine J. 2013;22(12):2770–2776.
- Hu Y, Yuan ZS, Kepler CK, et al. Deviation analysis of atlantoaxial pedicle screws assisted by a drill template. Orthopedics. 2014;37(5):e420–e427.
- Kaneyama S, Sugawara T, Sumi M. Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine (Phila, PA, 1976). 2015;40(6):E341–E348.
- Jiang L, Dong L, Tan M, et al. Accuracy assessment of atlantoaxial pedicle screws assisted by a novel drill guide template. Arch Orthop Trauma Surg. 2016;136(11):1483–1490.
- Deng T, Jiang M, Lei Q, et al. The accuracy and the safety of individualized 3D printing screws insertion templates for cervical screw insertion. Comput Assist Surg (Abingdon). 2016;21(1):143–149.
- Yu Z, Zhang G, Chen X, et al. Application of a novel 3D drill template for cervical pedicle screw tunnel design: a cadaveric study. Eur Spine J. 2017;26(9):2348–2356.
- Guo F, Dai J, Zhang J, et al. Individualized 3D printing navigation template for pedicle screw fixation in upper cervical spine. PLoS One. 2017;12(2):e171509.
- Bundoc RC, Delgado GG, Grozman SA. A novel patient-specific drill guide template for pedicle screw insertion into the subaxial cervical spine utilizing stereolithographic modelling: an in vitro study. Asian Spine J. 2017;11(1):4–14.
- Guo S, Lu T, Hu Q, et al. Accuracy assessment of using rapid prototyping drill templates for atlantoaxial screw placement: a Cadaver study. Biomed Res Int. 2016;2016:5075879.
- Neo M, Sakamoto T, Fujibayashi S, et al. The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine (Phila, PA, 1976). 2005;30(24):2800–2805.
- Kawaguchi Y, Nakano M, Yasuda T, et al. Development of a new technique for pedicle screw and Magerl screw insertion using a 3-dimensional image guide. Spine (Phila, PA, 1976). 2012;37(23):1983–1988.
- Kotani Y, Abumi K, Ito M, et al. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99(3 Suppl):257–263.
- Fan Y, Du JP, Wu Q N, et al. Accuracy of a patient-specific template for pedicle screw placement compared with a conventional method: a meta-analysis. Arch Orthop Trauma Surg. 2017;137(12):1641–1649.
- Merc M, Drstvensek I, Vogrin M, et al. Error rate of multi-level rapid prototyping trajectories for pedicle screw placement in lumbar and sacral spine. Chin J Traumatol. 2014;17(5):261–266.
- D'Urso PS, Williamson OD, Thompson RG. Biomodeling as an aid to spinal instrumentation. Spine (Phila, PA, 1976). 2005;30(24):2841–2845.
- Hartl R, Lam KS, Wang J, et al. Worldwide survey on the use of navigation in spine surgery. World Neurosurg. 2013;79(1):162–172.