Abstract
Image-free navigation has been proven as reliable as that using computed tomography (CT) in positioning the acetabular cup in total hip arthroplasty (THA), but previous studies rarely included hip dysplasia cases. The purpose of the present study was to determine the accuracies of CT-based navigation and image-free navigation for acetabular cup insertion, including hip dysplasia cases. Sixty-three hips were studied, including 57 with hip dysplasia. The hips were divided into two groups based on the registration point of image-free navigation. In Group I, the ipsilateral anterior superior iliac spine (ASIS) and the L5 spinous process were registered in 31 hips. In Group II, bilateral ASIS points were registered in 32 hips. Final component orientation was measured from postoperative CT scans. The accuracy of cup orientation was compared between CT-based and image-free navigation. In Group I, the cup inclination was more accurate with CT-based navigation (1.9°) than with image-free navigation (4.4°, p=.009). Cup anteversion was also more accurate with CT-based navigation (2.9°) than with image-free navigation (7.1°, p<.001). In Group II, the accuracies of cup inclination and anteversion showed no differences between CT-based and image-free navigation. The accuracy of cup positioning was better with CT-based navigation than with image-free navigation when the ipsilateral ASIS and L5 spinous process were digitized. However, accuracy was similar when bilateral ASIS points were digitized.
Introduction
Improper acetabular component positioning during total hip arthroplasty (THA) has been associated with the risk of dislocation [Citation1–3], reducing the range of motion (ROM) free from intraarticular impingement [Citation4,Citation5], and increased acetabular wear, as well as loosening [Citation1,Citation4,Citation6,Citation7]. There have been numerous reports regarding the optimal orientation of the acetabular component in THA [Citation1–7]. Although debate remains on this topic, the classical target for cup orientation in THA is the so-called ‘Lewinnek safe zone’, with an abduction angle of 40°±10° and an anteversion angle of 15°±10° [Citation2,Citation8].
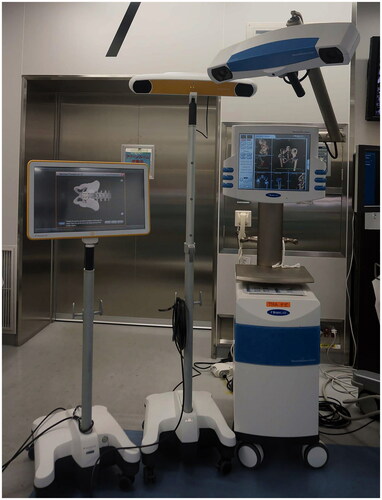
Navigation in THA improves the precision of acetabular cup placement by decreasing the number of outliers from the desired alignment [Citation9–11]. A computed tomography (CT)-based navigation system achieved high accuracy of cup positioning even in patients with hip dysplasia [Citation12–16] (). Image-free navigation proved as reliable as CT-based navigation [Citation7,Citation14,Citation17–19] (), but previous studies rarely included cases of hip dysplasia [Citation14]. For the registration process of the anterior pelvic plane, the surgeon registers bilateral anterior superior iliac spine (ASIS) points and the symphysis pubis. However, the percutaneous palpation of the pubis is quite imprecise [Citation20]. Haimerl et al. [Citation21] assessed basic statistics and variation in anatomical parameters using 420 CT data sets. They found that pubis points could be replaced by points around the acetabulum. The spinous process of the L5 vertebra could lie approximately on the midsagittal plane, and the contralateral ASIS point could be replaced by L5 spinous process. In addition, the distance between the ASIS points was needed. The deviations between a gold-standard APP registration and the new lateral registration approach were found to be 0.15°±2.86° in radiographic inclination and 0.27°±3.46° in anteversion. Davis et al. [Citation19] reported a new method for registration in the lateral decubitus position using image-free navigation. In the new registration methods with an image-free Hip 5.1 navigation system (Brainlab, Feldkirchen, Germany), the ipsilateral ASIS and the spinous process of the L5 vertebra or bilateral ASIS points were registered without registration of the symphysis pubis. The former method (L5 vertebra) enables the surgeon to acquire all registration points with the patient positioned and draped in the lateral decubitus position.
Table 1. The accuracy of cup orientation (difference between the intraoperative record and the postoperative measurement).
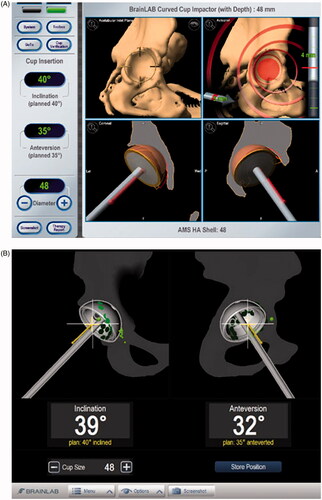
The purpose of the present study was to determine the accuracies of CT-based navigation and image-free navigation for acetabular component positioning in the lateral decubitus position using the new registration methods, including hip dysplasia cases. The accuracies of cup orientation using CT-based navigation and image-free navigation were examined simultaneously ().
Materials and methods
This retrospective study included consecutive patients underwent THA between May 2014 and June 2015. We made no exclusion criteria. Sixty-three hips were studied, including 57 with hip dysplasia. shows the demographics. Three hips were Crowe group 2 and two were group 3 [Citation22]. All the operations were performed by the same surgeon (AS) via a posterior approach. AHFIX Q3 (Kyocera, Kyoto, Japan) was used in 34 hips from May to December 2014, and SQRUM TT (Kyocera) was used in 29 hips after January 2015. The CT-based navigation was 2D–3D (two-dimensional to three-dimensional) matched navigation (Vector vision version 3.5, Brainlab). Using the 2D–3D matching, intraoperative registration of many anatomical landmarks is not required for matching. Preoperative CT images were taken from pelvis to knee joint using a multi-slice CT scanner. CT image data saved in DICOM format were transferred into the navigation system for preoperative planning considering pelvic tilt and intraoperative registration. Two fluoroscopic pelvic images taken from different angles of more than 20° were obtained. We took these images so that they contained the pubic tubercles and bilateral obturator foramens. Mean irradiation time was only a few seconds. After acquisition of these images, one point on the ASIS and two points on the iliac crest on the affected side were registered by direct palpation of these bony landmarks using the pointer. In 2D–3D matching registration, multidirectional fluoroscopic images were matched to the 3D pelvic images reconstructed from preoperative CT data. In the planning module, the anterior pelvic plane (APP) consisting of bilateral ASIS and pubic tubercles was identified [Citation15].
Table 2. Patients' characteristics.
Surgeons placed the cup according to the CT-based navigation planned preoperatively. Vector Vision (Brainlab) is supposed to use operative definition according to Murray [Citation23]. Operative inclination was planned at 40°, and operative anteversion was at 20° adjusted by the APP. The individual’s sagittal pelvic tilt is not taken into account when APP is used for the pelvic coordinates. Because the individual sagittal angle of APP is not always flat in a neutral (zero) position of the hip and it can be affected by an individual’s shape, aging or spinal deformity, we use a functional pelvic plane (FPP) where the pelvis in supine on the CT scan table is axially rotated until the bilateral ASIS touches the same horizontal plane [Citation24]. And the difference between APP and FPP was calculated. If sagittal pelvic tilt is 0°, the aim of operative anteversion was 20°. When the APP was parallel to CT scan table (), the aim of operative anteversion was 20°. When the APP was 15° anteverted compared with CT (), 35° (20°+15°) anteverted was planned (). Image-free navigation was also used, and cup inclination and anteversion were recorded (). In , CT-based navigation showed 40° inclination and 35° anteversion, and image-free navigation showed 39° inclination and 32° anteversion.
Figure 2. 3D computed tomography. (A) APP is flat in a neutral position (parallel to CT scan table). (B) APP is 15° anteverted compared with CT scan table.
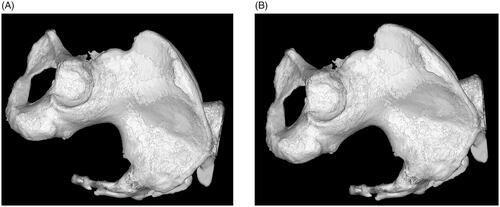
Figure 3. Screen shots of (A) CT-based navigation and (B) image-free navigation at the time of cup placement.
The hips were divided into two groups based on the registration points for image-free navigation (Image free Hip 6.0 navigation system, Brainlab). In Group I, the ipsilateral ASIS and the spinous process of the L5 vertebra were registered in 31 hips before November 2014. In Group II, bilateral ASIS points were registered in 32 hips after December 2014. A reference array was fixed onto the iliac spine on the treated side using two 4 mm Schanz screws. In Group I, the patient positioner was placed at a location that ensured free access to the spinous process of the L5 vertebra, which was used as a reference point on the mid sagittal plane. After the preparation of the patient, the L5 landmark was digitized through the drapes. The ASIS on the treated side was re-acquired to exactly reproduce the point acquisition process for a clinical setup performed in the lateral decubitus position. The distance between the ASIS was measured and entered onto the system. In Group II, the treated ASIS and non-treated ASIS were acquired on the tissue according to this pelvic reference in a semi-sterile environment, i.e. the area around the pelvic reference array was draped, whereas the other areas remained non-sterile. After the acquisition of these landmarks, the pointer was discarded and the patient was finally prepared according to the standard surgical procedure in a lateral decubitus position. After removal of the femoral head, the acetabular fossa and the acetabular cavity were digitized. Additionally, a point directly located at the anterior side of the acetabular rim (anterior rim point) was acquired. After inserting the cup, the final cup orientation was verified by the navigation system, and the navigation system recorded the final cup orientation [Citation19].
The final component orientation was measured from CT scans taken two weeks after surgery. CT image data saved in DICOM format were transferred into a three-dimensional template (Kyocera, Kyoto, Japan). First, the pelvic coordinate system was set to the APP on the coronal plane. The sagittal and axial planes were then defined as those perpendicular to the APP. Operative inclination and operative anteversion were measured [Citation15]. All measurements were performed by three independent observers in a blinded manner, and averaged data were used. The accuracy of cup orientation (absolute difference between the intraoperative record and the postoperative measurement) was compared between CT-based navigation and image-free navigation. An outlier was defined as greater than 5°. Operative inclination and anteversion angles were converted to radiographic inclination and anteversion angles. Using radiographic inclination and radiographic anteversion, the number of cups outside the safe zone was determined according to Lewinnek et al. [Citation2]. This study was approved by the local institutional review board, and all patients provided their informed consent.
Statistical analysis
In the final component orientation measured from CT, interclass correlation coefficients (ICCs) for the interobserver variability among three observers were 0.917 for inclination and 0.956 for anteversion in Group I and 0.957 for inclination and 0.988 for anteversion in Group II.
The accuracy of cup orientation was compared between CT-based navigation and image-free navigation using paired t-test. To compare outliers and non-outliers, the Mann Whitney U test was used for continuous data (age, body mass index (BMI), pelvic tilt and absolute value of pelvic tilt) of the two groups. The chi-squared test and Fisher’s exact test were used to compare sets of categorical data (sex, preoperative diagnosis, Crowe groups (1 vs 2, 3), and the number of outliers). A P value <.05 was considered significant.
The data of the first 10 hips were used to determine the sample size. The mean accuracy of cup inclination was1.7° with CT-based navigation and 2.9° with image-free navigation. The standard deviation (SD) of the accuracy of cup inclination was 2.0°. The mean accuracy of cup anteversion was 2.7° with CT-based navigation and 8.6° with image-free navigation. The SD of the accuracy of cup anteversion was 5.8°. The sample size was needed 25 hips for inclination and 10 hips for anteversion (ɑ=0.05, power = 0.8).
Results
The mean postoperative operative inclination and anteversion angles in all 63 hips were 38.6°±2.9° (range, 31.5°–44.8°) and 21.5°±6.8° (range, 7.4°–32.7°), respectively. The mean postoperative radiographic inclination and anteversion angles were 40.8°±3.0° (range, 34.5°–47.6°) and 16.6°±5.3° (range, 6.1°–27.4°), respectively. In all 63 hips, the accuracy of cup inclination was 1.9°±1.5° with CT-based navigation and 3.2°±3.4° with image-free navigation (p=.007). The accuracy of cup anteversion was 3.0°±2.3° with CT-based navigation and 5.6°±5.3° with image-free navigation (p<.001, ). Outliers for inclination occurred in 4 hips (6%) and 14 hips (22%) with CT-based navigation and with image-free navigation, respectively (p=.020). Outliers for anteversion were found in 11 hips (17%) and 23 hips (37%) with CT-based navigation and with image-free navigation, respectively (p=.026). Age, sex, BMI, pelvic tilt, the absolute value of pelvic tilt and Crowe groups showed no differences between outliers and non-outliers.
In Group I, the accuracy of cup inclination was 1.9°±1.5° with CT-based navigation and 4.4°±4.2° with image-free navigation (p=.005). The accuracy of cup anteversion was 2.9°±2.3° with CT-based navigation and 7.1°±6.3° with image-free navigation (p=.002). Outliers for inclination were found in 2 hips (6%) and 10 hips (32%) with CT-based navigation and with image-free navigation, respectively (p=.022). Outliers for anteversion were found in five hips (16%) and 14 hips (45%) with CT-based navigation and with image-free navigation, respectively (p=.026).
In Group II, the accuracy of cup inclination was 2.0°±1.5° with CT-based navigation and 2.1°±1.8° with image-free navigation (p=.757). The accuracy of cup anteversion was 3.2°±2.4° with CT-based navigation and 4.1°±3.6° with image-free navigation (p=.158). Outliers for inclination were found in two hips (6%) and 4 hips (13%) with CT-based navigation and with image-free navigation, respectively (p=.672). Outliers for anteversion were found in six hips (19%) and nine hips (28%) with CT-based navigation and with image-free navigation, respectively (p=.556).
Among the 63 hips, three cups (5%) were outside the safe zone.
Discussion
The accuracy of cup positioning was better with CT-based 2D–3D matched navigation than with image-free navigation when the ipsilateral ASIS and L5 spinous process were digitized. However, the accuracy was similar when bilateral ASIS points were digitized with image-free navigation. Davis et al. [Citation19] demonstrated that the mean error in component position was −1.1°±3.1° for inclination and 0.9°±4.3° for anteversion when the ipsilateral ASIS and L5 spinous process were digitized. This compared favorably with the error of −1.8°±1.8° for inclination and −4.8°±2.7° for anteversion when using the traditional APP registration (). In this study, absolute differences were not provided, which must be one of the reasons for such a good result with the registration of the ipsilateral ASIS and L5 spinous process. Bilateral ASIS registration is considered to be important to reduce image-free navigation error.
Intraoperative palpation of defined bony landmarks by the surgeon using a referenced pointer is a decisive step during the computer navigation data entry process. This procedure remains an important source of inaccuracy in imageless navigation systems [Citation17]. Ybinger et al. [Citation25] demonstrated the correlation between thickness of soft tissue overlying the pubic tubercles and error in anteversion measurements. Wolf et al. [Citation26] developed a mathematical model for calculating the resulting errors in anteversion and inclination from registration errors of the APP. Thus, a total error in the APP registration of only 4 mm can result in an error of 7° in anteversion and 2° in inclination. The usefulness of image-free navigation for hip dysplasia has required further investigation [Citation16]. Tsukada and Wakui [Citation18] showed no difference in terms of navigation accuracy between acetabular dysplasia and non-dysplasia cases. The present study showed a similar finding.
Nowadays, ‘Lewinnek safe zone’ could not be considered a safe zone given that the majority of these contemporary THAs that dislocated were within those target values [Citation27]. ‘Lewinnek safe zone’ is not always predictive of stability after THA. The concept of combined anteversion, the sum of cup anteversion and stem anteversion, has been proposed. Stem-first combined anteversion technique has been accepted as the optimal technique [Citation28]. Recent studies have focused on functional safe zone based on lateral spine-pelvis-hip radiograph. Femoral mobility is important [Citation29]. We use 3D planning before THA, and a combined anteversion is considered to prevent impingement. When the stem anteversion is less than 10° or more than 50°, we try to insert the stem with version control. In some cases, we select modular neck stem or Wagner type stem. The hips in this study were not used modular neck stem or Wagner type stem.
The limitations of this study included the small sample size and the lack of clinical results. In addition, there was a difference in operated periods between Group I and Group II, and mere learning curve might be the cause of the results. L5 spinous process was not easy to digitize for every patient. Some patients might have abnormal shapes of spinous processes. In addition, spino-pelvic mobility could be influenced. Sacral slope would change from intraoperative lateral decubitus position to supine position at the time of CT. The slope could also change during THA. It might be one of the reasons of the results. There were patients with anatomically asymmetric pelvis and/or rotated lumber spine, it might become another reason. However, the present study is the first to simultaneously compare CT-based 2D–3D matched navigation and image-free navigation with the new registration system.
Conclusion
The accuracy of cup positioning was better with CT-based navigation than with image-free navigation when the ipsilateral ASIS and L5 spinous process were digitized. However, the accuracy was similar when bilateral ASIS points were digitized in image-free navigation without pubis registration, which might be imprecise for overlying adipose tissue.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Kennedy JG, Rogers WB, Soffe KE, et al. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplast. 1998;13(5):530–534.
- Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220.
- Seagrave KG, Troelsen A, Malchau H, et al. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop. 2017;88(1):10–17.
- D'Lima DD, Urquhart AG, Buehler KO, et al. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321.
- McCarthy TF, Alipit V, Nevelos J, et al. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplast. 2016;31(9 Suppl):264–268.
- Del Schutte H, Jr, Lipman AJ, Bannar SM, et al. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplast. 1998;13(6):621–626.
- Lass R, Kubista B, Olischar B, et al. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplast. 2014;29(4):786–791.
- Parratte S, Ollivier M, Lunebourg A, et al. No Benefit after THA performed with computer-assisted cup placement: 10-year results of a randomized controlled study. Clin Orthop Relat Res. 2016;474(10):2085–2093.
- Gandhi R, Marchie A, Farrokhyar F, et al. Computer navigation in total hip replacement: a meta-analysis. Int Orthop (Sicot). 2009;33(3):593–597.
- Beckmann J, Stengel D, Tingart M, et al. Navigated cup implantation in hip arthroplasty. Acta Orthop. 2009;80(5):538–544.
- Liu Z, Gao Y, Cai L. Imageless navigation versus traditional method in total hip arthroplasty: a meta-analysis. Int J Surg. 2015;21:122–127.
- Sugano N, Takao M, Sakai T, et al. Does CT-based navigation improve the long-term survival in ceramic-on-ceramic THA? Clin Orthop Relat Res. 2012;470(11):3054–3059.
- Iwana D, Nakamura N, Miki H, et al. Accuracy of angle and position of the cup using computed tomography-based navigation systems in total hip arthroplasty. Comput Aided Surg. 2013;18(5–6):187–194.
- Kalteis T, Handel M, Bäthis H, et al. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88-B(2):163–167.
- Yamada K, Endo H, Tetsunaga T, et al. Accuracy of cup positioning with the computed tomography-based two-dimensional to three-dimensional matched navigation system: a prospective, randomized controlled study. J Arthroplast. 2018;33(1):136–143.
- Tsutsui T, Goto T, Wada K, et al. Efficacy of a computed tomography-based navigation system for placement of the acetabular component in total hip arthroplasty for developmental dysplasia of the hip. J Orthop Surg (Hong Kong). 2017;25:1–7.
- Sendtner E, Schuster T, Wörner M, et al. Accuracy of acetabular cup placement in computer-assisted, minimally-invasive THR in a lateral decubitus position. Int Orthop (Sicot). 2011;35(6):809–815.
- Tsukada S, Wakui M. Decreased accuracy of acetabular cup placement for imageless navigation in obese patients. J Orthop Sci. 2010;15(6):758–763.
- Davis ET, Schubert M, Wegner M, et al. A new method of registration in navigated hip arthroplasty without the need to register the anterior pelvic plane. J Arthroplast. 2015;30(1):55–60.
- Barbier O, Skalli W, Mainard L, et al. Computer assisted orthopedic surgery–france (caos-france). The reliability of the anterior pelvic plane for computer navigated acetabular component placement during total hip arthroplasty: prospective study with the EOS imaging system. Orthop Traumatol Surg Res. 2014;100(6):S287–S291.
- Haimerl M, Schubert M, Wegner M, et al. Anatomical relationships of human pelvises and their application to registration techniques. Comput Aided Surg. 2012;17(5):232–239.
- Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23.
- Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75(2):228–232.
- Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg. 2013;5(1):1–9.
- Ybinger T, Kumpan W, Hoffart HE, et al. Accuracy of navigation-assisted acetabular component positioning studied by computed tomography measurements: methods and results. J Arthroplast. 2007;22(6):812–817.
- Wolf A, Digioia AM, III, Mor AB, et al. Cup alignment error model for total hip arthroplasty. Clin Orthop Relat Res. 2005;437:132–137.
- Abdel MP, von Roth P, Jennings MT, et al. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res. 2016;474(2):386–391.
- Okada T, Fukunishi S, Takeda Y, et al. Total hip arthroplasty using stem-first technique with navigation: the potential of achievement of the optimal combined anteversion being a risk factor for anterior cup protrusion. Eur J Orthop Surg Traumatol. 2019;29(4):807–812.
- Tezuka T, Heckmann ND, Bodner RJ, et al. Functional safe zone is superior to the Lewinnek safe zone for total hip arthroplasty: why the Lewinnek safe zone is not always predictive of stability. J Arthroplast. 2019;34(1):3–8.