Abstract
Objective
Currently, the sacroiliac screws insertion still faces several challenges in the fixation of pelvic and acetabular injuries. This study was aimed to design a personalized three-dimensional (3D) printing assisted guide plates to assist sacroiliac screws insertion, so as to provide a reference for further clinical applications.
Methods
Eight pelvic specimens (5 males and 3 females) of normal adults were used to simulate actual operation. After thin-layer CT scanning, the 3D models of pelvis were established based on the images data. Furthermore, in Mimics 17.0 software, the screw entry points and screw channels of sacroiliac screws were further simulated and designed, and the appropriate range of the posterior superior iliac spine was selected to establish and print the virtual guide plates. Then, the simulated screws insertion was performed in vitro, the pelvic specimens after screws insertion were scanned again by CT, and the effect of screws insertion was further evaluated.
Results
A total of 16 sacroiliac screw guide plates were designed and printed, and 48 screws were inserted on both sides. Therein, 45 screws were completely located in the sacral vertebra, which was determined as grade 0, with an accuracy rate of 93.2%. The other 3 screws penetrated the anterior cortex or sacral canal of sacral vertebra, including 2 screws in Grade 1 (4.1%) and 1 screw in Grade 2 (2.1%). Compared with the simulated screw channels, the anterior and posterior offset angles of the cross section were (0.912 ± 0.625) ° and (0.802 ± 0.681) ° respectively, with no significant difference (p > 0.05). The upper and lower offset angles of coronal plane were (1.158 ± 0.823) ° and (1.034 ± 0.908) ° respectively, and there was no significant difference (p > 0.05).
Conclusions
3 D printing guide plates assisted sacroiliac screws insertion can enhance the stability of pelvic posterior ring fixation and assist surgeons to reduce the difficulty of operation.
Introduction
Recently, with the rapid development of construction and transportation, the high-energy trauma in modern society is increasing, which results in the incidence of pelvic and acetabular fractures to enhance year by year [Citation1–3]. On one hand, sacroiliac joint complex accounts for about 60% of the stability of the entire pelvis, and the stability of the pelvis depends largely on the sacroiliac joint complex (posterior pelvic ring) [Citation4,Citation5]. On the other hand, high-energy violence can lead to the severe injury to the posterior pelvic ring, and the active surgical intervention is particularly critical [Citation6,Citation7]. Among a variety of surgical interventions, the internal fixation can effectively ensure the accurate reduction of fractures and restore the anatomical structure and mechanical properties of the pelvis, so as to lay a solid foundation for the subsequent functional rehabilitation.
With regard to this, the sacroiliac screws are often used for the fixation of unstable posterior pelvic ring vertical fractures and sacroiliac joint dislocation. Sacroiliac screw is suitable for incision or percutaneous implantation, which has good biomechanical properties [Citation8]. In addition, for percutaneous fixation, it has the superiorities of less bleeding, short operation time, and less trauma to human tissues, but it still has great challenges at the technical level [Citation9,Citation10]. Due to the complex anatomy of sacrum, it is often difficult to insert the sacroiliac screws percutaneously with bare hands [Citation11]. Moreover, previous studies also reported that the incidence of inaccurate position of sacroiliac screws under the traditional X-ray fluoroscopy was 2–15%, and the incidence of symptomatic iliac vascular, L5 and sacral nerves injuries was 0.5–7% [Citation12,Citation13]. Thus, it can be recognized that the difficulty of sacroiliac screws insertion is mainly reflected in complex structure of adjacent tissues and the lack of visualization.
During the process of operation, it is necessary for the surgeons to accurately insert the sacroiliac screws from the ilium wing through ilium, auricular surface and sacrum. With regard to this, how to accurately insert the sacroiliac screws into sacrum, confirm the screws position and ensure its effective stability is an urgent issue to be solved and optimized currently. Hence, this current study intends to design a personalized 3D printing assisted guide plates to assist sacroiliac screws insertion, so as to provide a reference for the further clinical applications.
Materials and methods
Specimen preparation
This study was approved by the ethics committee of Jiangxi Provincial People's Hospital, The First Affiliated Hospital of Nanchang Medical College, and conducted in the 3D printing research center of Jiangxi Provincial People's Hospital, The First Affiliated Hospital of Nanchang Medical College. During this process, eight pelvic specimens (5 males and 3 females) of normal adults (Medical College, Nanchang University, Nanchang, Jiangxi, China) were used to simulate actual operation after examining by computer tomography (CT) to exclude the bone defects, deformities and apparent degeneration. Furthermore, we have thoroughly removed the anterior and posterior soft tissues of pelvis, preserve the ligaments around the sacroiliac joint and pubic symphysis, expose the complete pelvis, and dry the prepared specimens for standby.
The design of the entry points and channels of sacroiliac screws
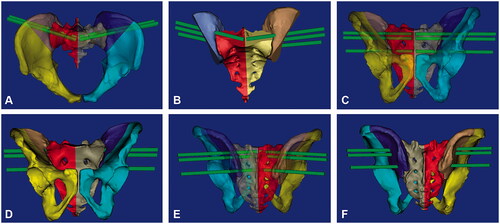
Double source CT (Siemens, Berlin, Germany) was used to conduct the thin-layer scanning of the pelvic specimens, and the scanning parameters were set as follow: tube voltage: 130 kV, current: 21.6 mA, scanning thickness: 0.625 mm, and layer spacing: 0.5 mm. The original CT data was imported into the Mimics 17.0 software (Materialise, Brussels, Belgium) in the Digital Imaging and Communications in Medicine (DICOM) format, and the bone structure was separated by the function of threshold segmentation. The threshold range was set to 200–3000 HU to establish the mask. The mask editing function was used to fill the bone structure defect layer by layer, and then the segmented mask was reconstructed to obtain the 3D model of pelvis. Then, in the medcad module of the Mimics 17.0 software, a cylinder was established to replace the screws for the simulated screws insertion, and the screw entry points and channels were designed by moving the cylinder. Furthermore, the transparency of sacrum was changed and the position, direction and angle of its entry points into the sacrum were adjusted until the cylinder was completely embedded in the sacrum. Ultimately, the screw channels were copied and enlarged to 7.3 mm to form the screw channel, and two screw channels were designed in the S1 vertebral body, and a single screw channel was designed in the S2 vertebral body. We also treated the cylinder on the other side in the same way. In order to ensure that the screws on both sides can be inserted, it was necessary to ensure that the left and right cylinders do not coincide and do not cross the midline of the sacrum. Hence, as shown in the , the ideal screw channels of bilateral S1 and S2 were designed via the above method.
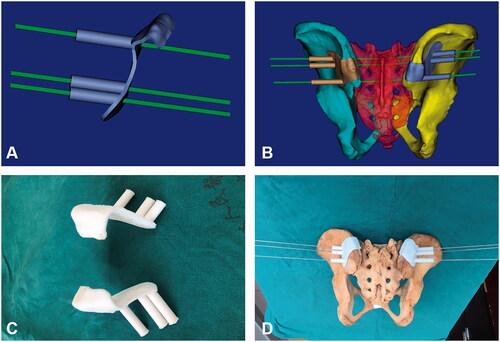
The design and manufacture of sacroiliac screw guide plates
During this process, we imported the 3D models of pelvis and designed cylinder into the UG software (Siemens, Berlin, Germany) in Stereolithography (STL) format, selected the appropriate range of the posterior superior iliac spine, then cut out the selected surface, and thickened it to 3.0 mm to form the base of screw guide plates. A new cylinder with an outer diameter of 7.3 mm was generated with a 2.5 mm cylinder as the center, and a hollow guide rod with an inner diameter of 2.5 mm and an outer diameter of 7.3 mm were formed through Boolean logic operation and connected with the base to generate the complete screw insertion guide plates. Ultimately, the guide plates data were imported into the 3 D printer in STL format to print the guide plates entity. The guide plates were then attached to the posterior superior iliac spine of the specimens in vitro, and the sacroiliac screws were simulated to observe the accuracy of the guide plate ().
Insert the screws under the guidance of guide plates
Next, we fixed the pelvic specimens on the operating table. In order to reduce the interference of human factors, the specimens were then covered with the hole towels to ensure that we could only observe the bilateral posterior superior iliac spine during the process of screws insertion. Subsequently, we placed the guide plate buckle on posterior superior iliac spine, so that it is in close contact with the posterior surface of the iliac bone. After confirming that the position of guide plates was positioned correctly and anchored firmly, the 2.5 mm Kirschner wires were drilled through hollow guide holes of the guide plates. A probe was used to further confirm the position and direction of the screw channel, and a hollow screw with a diameter of 7.3 mm was then screwed in after tapping. Each specimen underwent bilateral sacroiliac screws insertion, and a total of 48 screws were inserted ().
The observational indicators of this current study
The observational indicators of this study mainly included the safety and accuracy of screws insertion at the level of imaging examination. As for the imaging evaluation of the safety, after the insertion was completed, we conducted a thin-layer CT scanning again (the scanning parameters were the same as above), and understood the position of each screw through the cross-sectional and sagittal images (). The accuracy of sacroiliac screws insertion was assessed by the method introduced by the Smith et al. [Citation14]: (1) Grade 0: the screws were completely in the sacral vertebra; (2) Grade 1: the screws penetrated through the anterior cortex or spinal canal of the sacral vertebra, and the penetrating part was less than 2 mm; (3) Grade 2: the screws penetrated into the anterior cortex or spinal canal of the sacral vertebra, and the penetrating part was less than 4 mm; (4) Grade 3: the screws penetrated into the anterior cortex or spinal canal of the sacral vertebra, and the penetrating part was greater than 4 mm.
Figure 3. CT scan was used to evaluate the accuracy of sacroiliac screws insertion. (A): Measurement of the anterior and posterior offset angles (α) on cross section. The red solid line represented the preoperative simulated screw channel axis, and the black solid line represented actual screw channel axis; (B): Measurement of the upper and lower offset angles (β) on the coronal plane. The red solid line represented the preoperative simulated screw channel axis, and the black solid line represented actual screw channel axis.
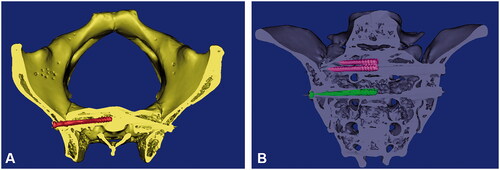
In terms of the evaluation of accuracy, we re-imported the postoperative thin-layer CT data of the pelvic specimens into Mimics 17.0 software to reconstruct the 3D models of the pelvis and screws. Postoperative models were fitted with preoperative models, and the position deviation between the actual screw trajectories and the simulated screw channels was directly observed, and the relevant data was then measured. According to the angles between the axis of actual screw channels and the ideal screw channels, the front and back offset angles of actual screw channels and ideal screw channels in the cross section were calculated (α1, α2), as well as the upper and lower offset angles on the coronal plane (β1, β2) ().
Statistical assessment
Statistical assessment was conducted using the SPSS 19.0 (SPSS, Inc, Chicago, IL). Compared with the preoperative simulated screw channels, when a screw had an offset in the direction of the spinal canal relative to the preoperative simulated screw channel, its posterior deviation angle was recorded as α1. Meanwhile, it was considered that there was no front offset, and the front offset angle (α2) was counted as 0. The same method was used to process the data of external offset in the cross section and the up and down offset angle in the sagittal plane (β1, β2). Levene method was used to test the homogeneity of variance, paired t-test was used when the variance was homogeneous, and Wilcoxon signed rank test was used when the variance was uneven. A p < 0.05 was considered to be statistically significant.
Results
The screws insertion under the guidance of guide plates
A total of 16 guide plates were designed and printed. All the guide plates were fitted and anchored accurately, and each guide plate was firmly closed without any shaking during the process of drilling. A total of 48 screws were then successfully inserted into the both sides, and there was no overlap of the screw channels.
The safety and accuracy of screws insertion
Through the interpretation of cross-sectional and sagittal CT images, 45 of the 48 screws were completely inserted in the sacral vertebra, which was determined as Grade 0, with an accuracy rate of 93.2%. The other 3 screws penetrated the anterior sacral vertebra or sacral canal, including the 2 screws in Grade 1 (4.1%) and 1 screw in Grade 2 (2.1%). As shown in , comparing the real screw channels with the ideal screw channels, there were 26 anterior offset screws and 22 posterior offset screws occurred on cross section, and the anterior offset angle (α1) was (0.867 ± 0.787) °, the posterior offset angle (α2) was (0.783 ± 0.792) °. Moreover, there were 25 upper offset screws and 23 lower offset screws occurred on the coronal plane, and the upper offset angle (β1) was (1.362 ± 1.380) °, the lower offset angle (β2) was (1.314 ± 1.300) °. There was no significant difference between the anterior and posterior offset angles, as well as the upper and lower offset angles.
Table 1. Comparison of the anterior and posterior offset angles of actual screw channels and the simulated screw channels in cross section and the upper and lower offset angles in coronal plane.
Discussion
The application of sacroiliac screws is an effective approach for the treatment of complicated and unstable posterior pelvic ring injuries in clinic, with the advantages of short operation time and rapid functional recovery [Citation15]. However, the proper sacroiliac screws insertion requires the familiarity with the anatomical structure of the sacroiliac joint and depends on the careful preoperative planning to reduce the risk of iatrogenic sacral peripheral nerve and vascular structure [Citation16,Citation17]. Thus, the key lies in the design of screw entry points and the screw channels. In fact, the ideal sacroiliac screw channels are located in the sacral vertebra without damaging the cauda equina nerve, lumbosacral trunk, iliac vessels, presacral vessels and L5/S1 intervertebral disk. In order to prevent the screws from penetrating through the bone and damaging the vital vessels and nerves, reduce the potential exposure of patients and surgeons to X-ray radiation, and improve the accuracy and safety of insertion, the novel auxiliary screws insertion technologies have been generally emerged. For example, the O-ARM navigation system, 3D printing technology, orthopedic robots, and so on [Citation18–20]. The O-ARM navigation system can display high-resolution images in sagittal plane, coronal plane and cross section at the same time. The surgeons can clearly observe the positional relationship between the fracture lines and screws on these three planes, and then insert the screws under the guidance of virtual guide needle, so as to improve the accuracy of insertion to a certain extent. However, the overall operation of O-ARM navigation system is complicated, and the operation and processing of navigation system also cost a lot of time. Moreover, orthopedic robots can conduct the position planning through the preoperative imaging and intraoperative real-time tracking. However, the cost of instruments and equipment is expensive, which is difficult to popularize in primary hospitals [Citation21]. Hence, there is still no ultimate conclusion on which technology is most suitable for the insertion of sacroiliac screws.
In this current study, the screw entry points and screw channels of sacroiliac screws were simulated by the Mimics 17.0 software, and then the 3D printing guide plates were used to guide the screws insertion on specimens. The results indicated that there was no statistical difference between the values simulated by the Mimics software and the actual values after using the 3D printing guide plates. Hence, using the Mimics software for virtual setting can fully exhibit the overall 3D anatomical structure of the pelvis, and accurately locate the sacroiliac joint, so that the whole screws insertion process can be conducted within the positioning range, with the effective safety and accuracy. On this basis, it can be concluded that using the 3D printing guide plates can maximize the success rate of the screws insertion.
In addition, after several years of continuous researches and development, the 3D printing technology has been widely applied in a variety of medical fields, especially in the field of orthopedics, which can assist in the personalized and accurate surgical treatment [Citation22]. Compared with the traditional insertion method, the application of 3D printing technology can improve the preoperative planning in sacroiliac joint surgeries. With regard to this, Wu et al. [Citation23] retrospectively analyzed 28 patients with the sacral fractures, of which 10 patients were assisted by the 3D printing guide plates to insert sacroiliac screws. This study indicated that the screws insertion assisted by 3D printing guide plates has the reliable accuracy, which can reduce the number of intraoperative fluoroscopy shrinkage, shorten the operation time, and avoid the neurovascular injury caused by improper screws position. Moreover, 3D digital models can be constructed by the Mimics software to simulate and design the insertion points, insertion angles and insertion depth of the sacroiliac screws, and the surgeons can also design the guide plate according to the simulation results.
Furthermore, inserting the screws directly from guide plate holes can also reduce the difficulty of operation, improve the accuracy, shorten the insertion time, and reduce the X-ray radiation exposure [Citation24]. 3D printing technology is also equipped with high clinical practical value, and it provides options other than the computer navigation and orthopedic robots for the screws insertion, and it can also be expanded in primary and secondary hospitals [Citation21]. In addition, the 3D printing guide plates are mainly composed of the guide plate holes and guide plate base. Whether the guide plates can be accurately anchored to the established position and maintain the stability of position during drilling is the key to ensure the accuracy of screws insertion [Citation25,Citation26]. Meanwhile, the overall stability is mainly determined by the guide base in direct contact with bone surface. In this current study, we designed the guide base with the posterior superior iliac spine as the anchor mark. The convexity of this part was rough and irregular, and the guide plate was fitted here. It was not easy to cause the guide plate to shake and change the position when the screws were inserted, and the accuracy was relatively reliable. However, how to balance the fit degree and exposure the range of the guide plates still needs further exploration.
Ultimately, it is still essential to recognize the shortcomings of this current study. Firstly, the correct placement of the guide plates is vital. If there is an error between the guide plates and the bone surface, it may also result in the displacement of the screws position and cause iatrogenic damage. The invasiveness of using 3D printing assisted guide plates insertion should be emphasized. According to the 3D printing assisted guide plates, it is necessary to expose not only the area of the posterior superior iliac spine, but have to expose good part of the outer table of the posterior iliac wing to anchor the guide plate. This operation will definitely be associated with more complications (such as bleeding, infection and other wound issues) in comparison to current standard percutaneous insertions. When placing the guide plates, it is necessary to cut and peel the soft tissue on the bone surface of the base of guide plates to expose the bone signs of posterior superior iliac spine, which is more traumatic than traditional surgical method. Secondly, another important limitation is that the operators would need anatomic reduction of any displaced injury around the sacroiliac joint to ensure the accuracy of guided screws insertion. Actually, in significantly displaced sacroiliac injuries, it is usually not able to have anatomical reduction and some minor displacements might be accepted by us. Due to the narrow channel of sacroiliac screws insertion, those minor displacements would be significant limiting factors of 3D printing assisted guide plates insertion that rely on the anatomic relation between the intact pelvis, posterior ilium and sacral body. Thirdly, the variation between both pelvic sides should be studied, because in case of a displaced unilateral posterior pelvic disruption, the operators should further discover a method (such as mirror reset) for relying on the 3D anatomy of intact contralateral side. Fourth, in cases of the bilateral posterior pelvic ring injuries, the accuracy of this technique will be much lower if both sides have some displacement. Fifth, the sample size of this study is relatively small, which is still essential to improve the sample size in the next research stage. Sixth, in order to further verify the clinical efficacy and prognosis of this 3D printing guide plates in assisting the sacroiliac screws insertion, more prospective studies and larger sample size data are still needed in the future.
Conclusions
To sum up, 3D printing guide plates assisted sacroiliac screws insertion has high practical value and can help the sacroiliac screws to be inserted safely. Especially for the severe sacroiliac joint fracture or dislocation, it can enhance the stability of pelvic posterior ring fixation and assist surgeons to reduce the difficulty of operation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- de Ridder VA, Olson SA. Operative treatment of pediatric pelvic and acetabulum fractures. J Orthop Trauma. 2019;33(Suppl 8):S33–s37.
- Kelly J, Ladurner A, Rickman M. Surgical management of acetabular fractures - a contemporary literature review. Injury. 2020;51(10):2267–2277.
- Veerappa LA, Tippannavar A, Goyal T, et al. A systematic review of combined pelvic and acetabular injuries. J Clin Orthop Trauma. 2020;11(6):983–988.
- Abdelfattah A, Moed BR. Ligamentous contributions to pelvic stability in a rotationally unstable open-book injury: a cadaver study. Injury. 2014;45(10):1599–1603.
- Sichting F, Rossol J, Soisson O, et al. Pelvic belt effects on sacroiliac joint ligaments: a computational approach to understand therapeutic effects of pelvic belts. Pain Physician. 2014;17(1):43–51.
- Wang H, Fu YH, Ke C, et al. Minimally invasive stabilisation of posterior pelvic ring instabilities with pedicle screws connected to a transverse rod. Int Orthop. 2018;42(3):681–686.
- Eastman JG, Shelton TJ, Routt MLC, Jr, et al. Posterior pelvic ring bone density with implications for percutaneous screw fixation. Eur J Orthop Surg Traumatol. 2021;31(2):383–389.
- Suero EM, Greiner A, Becker CA, et al. Biomechanical stability of sacroiliac screw osteosynthesis with and without cement augmentation. Injury. 2021;52(10):2707–2711.
- Wang JQ, Wang Y, Feng Y, et al. Percutaneous sacroiliac screw placement: a prospective randomized comparison of robot-assisted navigation procedures with a conventional technique. Chin Med J (Engl). 2017;130(21):2527–2534.
- Shetty AP, Renjith KR, Perumal R, et al. Posterior stabilization of unstable sacral fractures: a Single-Center experience of percutaneous sacroiliac screw and lumbopelvic fixation in 67 cases. Asian Spine J. 2021;15(5):575–583.
- Teo AQA, Yik JH, Jin Keat SN, et al. Accuracy of sacroiliac screw placement with and without intraoperative navigation and clinical application of the sacral dysmorphism score. Injury. 2018;49(7):1302–1306.
- Zhou W, Xia T, Liu Y, et al. Comparative study of sacroiliac screw placement guided by 3D-printed template technology and X-ray fluoroscopy. Arch Orthop Trauma Surg. 2020;140(1):11–17.
- Zhang R, Yin Y, Li S, et al. Percutaneous sacroiliac screw versus anterior plating for sacroiliac joint disruption: a retrospective cohort study. Int J Surg. 2018;50:11–16.
- Smith HE, Yuan PS, Sasso R, et al. An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine (Phila Pa 1976). 2006;31(2):234–238.
- Chen HW, Liu GD, Fei J, et al. Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: a comparative study. J Orthop Sci. 2012;17(5):580–587.
- Mirkovic S, Abitbol JJ, Steinman J, et al. Anatomic consideration for sacral screw placement. Spine (Phila Pa 1976). 1991;16(6 Suppl):S289–S94.
- Zhao Y, You L, Lian W, et al. Anatomical relation between S1 sacroiliac screws’ entrance points and superior gluteal artery. J Orthop Surg Res. 2018;13(1):15.
- Chen X, Zheng F, Zhang G, et al. An experimental study on the safe placement of sacroiliac screws using a 3D printing navigation module. Ann Transl Med. 2020;8(22):1512.
- Feng W, Wang W, Chen S, et al. O-arm navigation versus C-arm guidance for pedicle screw placement in spine surgery: a systematic review and Meta-analysis. Int Orthop. 2020;44(5):919–926.
- Al-Naseem A, Sallam A, Gonnah A, et al. Robot-assisted versus conventional percutaneous sacroiliac screw fixation for posterior pelvic ring injuries: a systematic review and Meta-analysis. Eur J Orthop Surg Traumatol. 2021. doi:10.1007/s00590-021-03167-x.
- Dong XP, Zhang YW, Pei YJ, et al. Three-dimensional printing for the accurate orthopedics: clinical cases analysis. Bio-Des Manuf. 2020;3(2):122–132.
- Zhang YW, You MR, Zhang XX, et al. The novel application of three-dimensional printing assisted patient-specific instrument osteotomy guide in the precise osteotomy of adult talipes equinovarus. Biomed Res Int. 2021;2021:1–10.
- Wu C, Deng J, Tan L, et al. Effectiveness analysis of three-dimensional printing assisted surgery for unstable pelvic fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(4):455–461.
- Zhang YW, Xiao X, Xiao Y, et al. Efficacy and prognosis of 3D printing technology in treatment of high-energy trans-syndesmotic ankle fracture dislocation – “Log-Splitter” injury. Med Sci Monit. 2019;25:4233–4243.
- Zhang YW, Deng L, Zhang XX, et al. Three-Dimensional Printing-Assisted cervical anterior bilateral pedicle screw fixation of artificial vertebral body for cervical tuberculosis. World Neurosurg. 2019;127:25–30.
- Zhang YW, Xiao X, Gao WC, et al. Efficacy evaluation of three-dimensional printing assisted osteotomy guide plate in accurate osteotomy of adolescent cubitus varus deformity. J Orthop Surg Res. 2019;14(1):353.