?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
To explore the safety and feasibility of wireless thoracoscope in thoracic surgery. A retrospective analysis was made of all the clinical data of 90 patients with thoracoscope lung resection, from April to August 2021, Shanghai changzheng hospital thoracic minimally invasive center. Compared the thoracoscope preparation time, picture resolution, picture delay, surgeon comfort level, assistant comfort level between the wireless thoracoscope group and wired thoracoscope group. The thoracoscopic preparation time of the wireless thoracoscope group was significantly shorter than that of the wired group (26.66 ± 6.04 vs 62.14 ± 10.07, p < 0.0001). Comfort level of the surgeon (4.64 ± 0.48 vs 3.77 ± 0.42, p < 0.001) and the comfort level of the assistant (4.85 ± 0.36 vs 3.88 ± 0.32, p < 0.001) of the wireless thoracoscope group were higher than that of the wired thoracoscope group. There were no statistically significant differences in video sharpness (4.64 ± 0.48 vs 4.74 ± 0.44, p = 0.31). Although there was one case picture delay in wireless group, it was caused by low power which could be dealt with by a good charge before surgery. The wireless thoracoscope has the advantages of short preparation time, high comfort for the surgeon and the assistant, no less than the wired thoracoscope in picture resolution and picture delay. Wireless connection is more convenient and portability, which is worthy of further application in clinical practice.
Keywords:
Thoracoscopic technology originated in the early twentieth century. As early as 1911, Swedish JACOBEUS [Citation1] first reported the application of thoracoscopic technology [Citation2]. However, due to equipment and technical reasons, thoracoscopic technology was limited to the diagnosis of pleural diseases and the application of thoracic adhesion release for a long period of time. Nowadays, with the rapid development of thoracoscopic technology, thoracoscopic technology has been widely applied in clinical practice, which not only reduces surgical trauma and surgical risk, but also provides better surgical results [Citation3].
The traditional wired thoracoscope consists of two parts: the part on the operating table and the part out of the table. The part out of the table is large, heavy and inconvenient to move [Citation4]. Meanwhile, the part of on the table is complicated [Citation5]. These reasons lead to long preparation time for thoracoscopic surgery, limited intraoperative operation, and easy violation of the principle of asepsis [Citation6]. We cooperated the wireless thoracoscope, which has been initially applied in clinical practice. The report is as follows.
1. Materials and methods
We have been examined and approved by the ethics committee of Shanghai Changzheng Hospital. All research was performed in accordance with relevant guidelines, and consent was obtained from all participants.
1.1. Introduction to wireless thoracoscopic
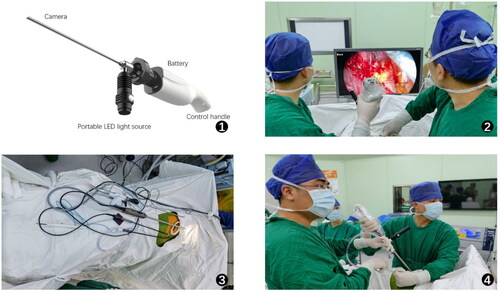
The wireless thoracoscope is composed of two parts: the platform on the operating table and the platform out of the table. The platform on the operating table includes wireless transmission area, functional control area, battery compartment and miniature high-energy LED cold light source (). The platform out of the table consists of a display that can accept 5 G communication technology. Wireless thoracoscope is compatible with all kinds of conventional thoracoscopic lenses. It uses micro high-energy LED cold light source technology to replace traditional optical cable, and uses ultra-high definition imaging technology to replace camera cable [Citation6]. Meanwhile, it has its own power supply battery that can last 3–4 h, and adopts independently developed 5 G module. The image data collected by the camera can be transmitted to the display with low delay even no delay to achieve surgical operation [Citation7].
1.2. Preliminary application of wireless thoracoscope
Clinical data of 90 patients undergoing thoracoscopic pneumonectomy in the Minimally invasive Thoracic Surgery Center of Shanghai Changzheng Hospital in April to August 2021 were retrospectively analyzed. Among them, 47 patients were treated with the wireless thoracoscope (), and 43 patients were treated with traditional wired thoracoscopic 1080p. The two groups were compared in thoracoscope preparation time, picture resolution, picture delay, surgeon comfort level, assistant comfort level and other aspects. All data were scored by the surgeon and recorded by his assistant during the operation immediately. Since there is no official rating scale, the resolution of the picture was evaluated with a 5-point Likert scale (1 = very unclear, 5 = very clear), and the comfort level of the surgeon and the assistant was evaluated with a 5-point Likert scale (1 = very uncomfortable, 5 = very comfortable).
1.3. Statistical analysis
SPSS 20.0 was used for data analysis. The measurement data were described by mean ± standard deviation (±s), and the counting data were described by frequency. T test was used to analyze and compare the scores of the two groups. p Value < 0.05 was considered statistically significant.
2. Results
2.1. There was no statistical difference in the general data between the two groups, which was comparable ()
Table 1. General data between the two groups.
2.2. The thoracoscopic preparation time of the wireless thoracoscope group was significantly shorter than that of the traditional wired group (26.66 ± 6.04 vs 62.14 ± 10.07, p < 0.0001)
The comfort level of the surgeon (4.66 ± 0.47 vs 3.77 ± 0.42, p < 0.001) and the comfort level of the assistant (4.85 ± 0.36 vs 3.88 ± 0.32, p < 0.001) of the wireless thoracoscope group were higher than that of the traditional wired group. There were no statistically significant differences in picture resolution (4.64 ± 0.48 vs 4.74 ± 0.44, p = 0.31). There was one case picture delay in wireless group ().
Table 2. Comparison of outcome indicators between the two groups.
3. Discussion
Thoracoscopic surgery is an inevitable development of medicine. It not only meets the needs of patients for more ‘minimally invasive’ surgery, but also achieves better surgical results for doctors. Traditional wired thoracoscope consists of two parts: the part on the operating table and the part out of the table. The wires on the table are complicated, and the part under the table are large, heavy, and inconvenient to move [Citation4]. These reasons lead to long preparation time for thoracoscopic surgery, limited intraoperative operation, and easy violation of the principle of asepsis. The wireless thoracoscope developed by us has the characteristics of clear imaging, wireless connection and convenient portability, which well solves the problem of appeal.
The traditional wired thoracoscope includes lens, camera and operation handle, optical cable, cold light source, camera system, monitor, connection line, etc. The part outside the operation table is generally installed on a vehicle 1.5 m or so. The thoracoscopic connection needs to be completed by the surgeon and the instrument nurse before the operation, and the thoracoscopic protective sleeve is required to ensure sterility of the handle [Citation8], so a large amount of preparation time is required. However wireless thoracoscope without performer and instrument nurses, the part on and out of the operating table fully connected through wireless communication technology, separated the two parts completely, shorten the preparation time of thoracoscope, our research results also proved that the average preparation time was more than doubled.
For surgery, due to the existence of a variety of wires in the traditional wired thoracoscope, the operating table needs to have a special space for these wires. As the surgery progresses, the use of various surgical instruments and the intertwining of connecting wires will further disturb the spatial order of the operating table. The disorderly operating table is easy to cause the fall of surgical instruments, bringing inconvenience to the operator and the lens operator [Citation6] (). In addition, the intraoperative rearrangement of the wires also increases the operation time. At the same time, because the assistant needs to use thoracoscopic protective sleeve to ensure sterility, damage of the protective sleeve or loosening of the binding interface during the operation will violate the principle of sterility and increase the risk of surgical infection [Citation8]. The wireless thoracoscopic does not need connecting wires, which, on the one hand, makes the operating table clean and tidy, and on the other hand, avoids possible violation of the principle of asepsis ().
Our study also found that the wireless thoracoscope improved the comfort level of the surgeon and the assistant during surgery. Though the thoracoscopic preparation time of the wireless thoracoscope group was significantly shorter than that of the traditional wired group, this difference was clinically minimal. But our surgeon and assistant found that easy connection of wireless thoracoscope and the cleanliness of the operating table can improve the surgical comfort of the surgeon and the assistant to a certain extent. In addition, without the limitation of connecting wires, on the one hand, the interference of connecting wires to the operation of surgical instruments can be avoided, especially the interference of optical cable angle change to operator in uniport thoracoscopic surgery. On the other hand, the assistant is no longer limited by the length of connecting wires and can freely adjust the distance and direction of the lens. All of these increase the comfort of the surgeon and the assistant.
At the same time, our study showed that the use of wireless thoracoscope did not reduce the picture resolution and signal transmission speed, and there was no significant difference from the use of traditional thoracoscopy in the above two aspects. On the one hand, thanks to the use of 5G communication technology, on the other hand, thanks to the use of HIGH-DEFINITION displays. We customize the protocol so that the transmitted video signal operates in a specific frequency band. Therefore, on the one hand, our delay fluctuates between 60 and 100 ms, which does not affect the procedure of the surgeon; on the other hand, as a dedicated frequency band, it is not easy to be interfered by external signals. However, we found in the process of use that the picture tone of wireless thoracoscope is a little darker than that of traditional wired thoracoscope, which needs to be compensated by adjusting the illumination direction and angle of the light source. We guess it is due to the image acquisition system RGB three primary color Settings are not perfect. We are continuously debugging in the subsequent process, in order to present better surgical images. In the 47 cases of wireless thoracoscope group, there was delay about 2 s in one case, so we replaced the traditional wired thoracoscope in time and continued the operation to ensure safety. Afterwards, we found it was caused by the insufficient electric power of the operating handle. Because the operation handle showed low power, and after we replaced the battery, the delay disappeared. However, no delay was found in the case of sufficient electric power. The battery power is 7000 mAh, the operating handle voltage is 5 V, the motherboard power is 5 W, and the light source power is 5 W. According to the calculation, the battery can last 3.5 h (7000 mAh*5V/(5W + 5W)). In the actual use process, we found that the power supply battery of the wireless thoracoscope can be used for 3–4 h continuously when the operating handle and light source are supplied at the same time, which is enough to meet the needs of a conventional thoracoscopic lung surgery (which takes about two hours to complete a lung surgery on average). So we don’t have to replace the battery during the operation. At the same time, for patients with long estimated operation time before surgery, we used separate power supply between the light source and the operating handle to maintain the electric power of the lineless cavity lens at 7–8 h. However, for the surgery with thoracoscopic adhesion, anatomical variation and other complex conditions, the power supply mode with stronger endurance needs to be further discussed.
Wireless thoracoscope uses a miniature high-energy LED cold light source to replace the fiber optic cable line and video receiving line, and only requires a monitor outside the operating table that can be connected wirelessly to the part on the operating table, greatly reducing the volume of the thoracoscope outside the table and making it portable. Therefore, it is possible to use wireless thoracoscopy in emergency rooms, wards, outpatient clinics and even patients’ homes.
The wireless thoracoscope developed by us has the characteristics of clear imaging, wireless connection and convenient portability, which greatly reduces the operation preparation time, improves the comfort of the surgeon and the assistant, and ensures the real-time transmission and high definition of the surgical video, which is worthy of further promotion in clinical practice.
Author contributions
(I) Conception and design: Hua Tang, Kenan Huang; (II) Administrative support: Zhifei Xu; (III) Provision of study materials or patients: Xiaoyu Wu, Junjie Hu, Kenan Huang; (IV) Collection and assembly of data: Ning Xin, Rongqiang Wei, Zihao Chen; (V) Data analysis and interpretation: Ning Xin, Xiaoyu Wu, Junjie Hu; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Jacobeus H. Kurze ubersicht uber meine erfahrungen mit Laparo-Thracoscopie. Munchen Med Wochenschr. 1911;58:1911.
- Nakamura H. Systematic review of published studies on safety and efficacy of thoracoscopic and robot-assisted lobectomy for lung cancer. Ann Thorac Cardiovasc Surg. 2014;20(2):93–98.
- Zhao Z, Hong Z. Development of surgical thoracoscopy. Clin J Lung Dis. 2018;11(5):3.
- Baker E, Drummond J, Stefanidis D, et al. Use of a novel, cordless ultrasonic dissector for gynecologic minimally invasive surgical procedures. J Minim Invasive Gynecol. 2015;22(6S):S43–S44.
- Gjeraa K, Spanager L, Konge L, et al. Non-technical skills in minimally invasive surgery teams: a systematic review. Surg Endosc. 2015;30(12):1–15.
- Chen CH, Chang H, Liu TP, et al. Application of wireless electrical non-fiberoptic endoscope: potential benefit and limitation in endoscopic surgery. Int J Surg. 2015;19:6–10.
- Lacy AM, Bravo R, Otero‐pieiro A, et al. 5G‐assisted telementored surgery. Br J Surg. 2019;106(12):1576–1579.
- Tsirline VB, Lau KN, Swan RZ, et al. Evaluation of an innovative, cordless ultrasonic dissector. Surg Innov. 2013;20(5):524–529.