Welcome to this special issue of the IISE Transactions on Ergonomics and Human Factors (Please see a note below about papers in a joint special issue of the IISE Transactions on Healthcare Systems Engineering). This special issue was driven by the arguably self-evident conclusion drawn by both the Human Factors and Healthcare Systems Engineering communities: People are central to healthcare systems (HCS) and quality patient care. Without skilled, knowledgeable, and well-prepared professional personnel, the healthcare system will not work, regardless of how sophisticated the technology provided is. Ultimately, healthcare is a sociotechnical system (Carayon et al., Citation2011), and its optimal functioning hinges on the quality of the interaction between the humans and the technological aspects (defined broadly) of the system. Therefore, we assert, the quality of human factors within the system will have a critical effect on the people in the HCS and thus the system’s safety and effectiveness.
For this introduction, we adopt the International Ergonomics Association’s definition of human factors (HF - used synonymously here with ergonomics per the international definition): “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance” (IEA Council, 2014). We note in particular that the design of any sociotechnical system calls for careful decisions affecting the demands placed on human perceptual, cognitive, and motor systems (e.g., Helander, Citation2006). These systems, and the organizational structures of their implementation, will also influence the psychosocial aspects for the human in the system – factors such as control at work, coworker and supervisor support, and effort-reward imbalances affect stress and can contribute to musculoskeletal disorders in personnel (e.g., Moon & Sauter, Citation1996). Human responses to the demands placed on them by the system, and the consequences of overload of any of these systems, will determine both human well-being and system performance. Human Factors, therefore, are a central element to all of engineering design. It’s unfortunate, however, that engineers are not frequently trained to understand the consequences of their design choices in terms of HF (Broberg, Citation1997; Neumann, Winkel, Medbo, Magneberg, & Mathiassen, Citation2006; Salmon & Read, Citation2018). It is further problematic that the organization of the design process fosters this gap by relegating HF to specialists or consultants who are often separated from the design process by time, location, and organizational goals (Neumann & Village, Citation2012). It is the intent of this special issue to contribute to the closing of this gap and to motivate people to do so in their own research and HCS design work.
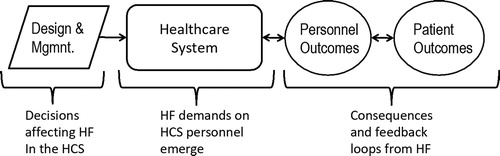
The Systems Engineering Initiative for Patient Safety (SEIPS) model, originally proposed by Pascale Carayon et al. (Citation2006) and extended (Holden et al., Citation2013), is probably the most widely spread model of the sociotechnical nature of healthcare systems. This model is a useful way to consider how the consequences of HCS design will affect the relevant personnel, in better or worse ways, which will in turn affect the quality of care delivered, and hence determine patient outcomes, for better or for worse. In short, poor HF in design is likely to have negative consequences on caregivers and compromise patient health (Aiken et al., Citation2011; Kieft, de Brouwer, Francke, & Delnoij, Citation2014). We present a simplified illustration of this argument in , which highlights that engineers and other decision makers determining healthcare system design have a responsibility to meet the needs of the system users – the caregivers and other personnel – if they hope to meet the care delivery needs of patients. As the papers in this special issue illustrate, this responsibility goes well beyond mere issues of “usability” that are sometimes considered in the design of HCS technologies.
Figure 1 Chain of effects illustrating how HCS design and operational management decisions will determine HF demands on personnel, with cascading effects for both personnel and patients. Resulting feedback cycles can be negative (vicious) or positive (virtuous).
When HF aspects are not adequately considered in the design and management of HCS, then problems are likely to emerge. Possible problems include fatigue, injury, and errors caused by excess demands to the sensory (poor font sizes), cognitive (complex procedures and control panels), and motor (low back loads or excess shoulder loads from materials handling) systems. Such problems can emerge in the context of the use of a device or machine, where poor design often leads to ineffective or inefficient use, as well as increased use errors (i.e., mistakes) that can lead to harm. In this issue, Milloy & Bubric (Citation2018) provide an example of a project that produced improved HF in the design of a hospital “crash cart”. Problems related to HF can also affect the work environment of personnel, leading to excess workloads that increase injury risks for staff. Research with nurses has shown strong links between poor work environments and declines in care quality for patients (Poghosyan et al., Citation2010; Spence Laschinger, Shamian, & Thomson, 2001). In this special issue, we include papers that aim to improve the work of nurses in acute care, for doctors, for pharmacists, for hospital cleaners, for nurses providing chemotherapy treatments, and for inter-professional teams. These are all examples of the wide range of personnel who are affected by HF in the design of the HCS – with those effects, in turn, affecting care quality for patients. These papers contribute to the knowledge needed to ensure that HCS personnel have good working environments, which supports the delivery of high-quality care. While the link between HF and quality has been studied in other sectors, such as manufacturing (e.g., Kolus et al., Citation2018), it is in the healthcare sector that problems related to poor work environment can prove injurious or fatal for the patient, making the issue particularly acute.
To provide an overview of this special joint issue, we present a summary table () examining the studies included in the issue. This summary was created based on the theoretical framework given in . We considered the sub-system or context of the study, the personnel under study, and the organizational factors considered in the study. These aspects provide insight into the design factors that are under consideration in the study. Subsequently, we examined the nature of the HF under study: the perceptual, cognitive, or motor demands of the HCS personnel’s tasks, followed by an assessment of the effects on personnel themselves, or effects on patients. While somewhat subjective, this approach yielded an overview of the studies in this special issue, and raised some interesting points about the research being conducted in this area.
TABLE 1 Summary of the papers in the special issue and key features of each
The astute reader may already be asking, why psychosocial factors are not explicitly included in the summary table? We know that psychosocial factors are important, and indeed are central to problematic personnel outcomes such as burnout (Bourbonnais et al., Citation1998; Hinderer et al., Citation2014); a serious problem among nurses and physicians. The answer is that only one paper in this special joint issue, the study of Arsenault-Knudsen, Brzozowski, and Steege (2018), addressed psychosocial aspects directly. While a product of the design of the work systems (Neumann et al., Citation2006), relatively few engineering journals have dealt with how their designs affect the psychosocial environment of employees, nor what effects the design of the psychosocial environment has on employee wellbeing and performance. This area poses a weak-spot in our research knowledge in HCS engineering specifically, and in industrial and systems engineering research in general. We encourage researchers to address these aspects in their work.
This special issue contains ten papers that reflect the breadth of HF research and applications in healthcare systems engineering. The included studies and application projects address a range of healthcare workers, including nursing students, physicians, cleaning staff, nurses, pharmacy assistants, and pharmacists, across several healthcare contexts (rural settings, acute care hospitals, ambulatory clinics, emergency rooms, and hospital pharmacies). Authors of these papers used diverse methods and research approaches (e.g., simulation, observation, quasi-experimental designs) to develop and contribute new knowledge that increases our understanding of and guides recommendations for improvements to the interactions between healthcare staff and: (1) tools and technologies (Milloy & Bubric, Citation2018; Weiler et al, Citation2018); (2) tasks (Bargal et al., Citation2018; Doss et al., Citation2018; MacDonald & Keir, 2018; Xie et al., Citation2018); (3) the physical environment (Arsenault-Knudsen et al., 2018; Weiler et al., Citation2018); and (4) organizational structures (Arsenault-Knudsen et al., 2018; Bargal et al., Citation2018; Ibrahim Shire, Thomas Jun, & Robinson, Citation2018; Podtschaske, Salazar, & Rao, Citation2018). Importantly, diverse areas of study within human factors and ergonomics (perception, cognition, physical ergonomics, organizational ergonomics) are considered within these papers and most papers address more than one area.
We now briefly introduce each of the papers in this special issue:
Several studies focused on and engaged nursing professionals. Doss, Robathan, Abdel-Malek, and Holmes (Citation2018) emphasized physically-demanding aspects of nursing work, specifically patient handling, and associated risks for the development of musculoskeletal injuries in nurses. Their multi-modal training program (verbal instruction and real-time auditory feedback) aimed at improving patient handling techniques in a student nurse population. Their results support the effectiveness of a short training protocol on improving trunk kinematics immediately following training. This type of program could help in educating future healthcare professionals, to increase safety and reduce rates of injury due to patient handling tasks.
MacDonald and Keir (2018) also assessed physical risk factors for musculoskeletal disorders in both chemotherapy nurses and pharmacy assistants. They used observation and direct measures (forearm muscle activity and thumb press forces) to monitor hand and syringe activities in chemotherapy preparation and administration processes throughout a work shift and to assess musculoskeletal risk. Their results indicated that, although there were differences between individual workers and between chemotherapy nurses versus pharmacy assistants, syringe and hand tasks contribute to muscular overload and an increased risk for work-related musculoskeletal disorders. Importantly, findings from their study can guide strategies to reduce risks, such as training on techniques to reduce muscular load and administrative controls related to task sequencing and scheduling breaks.
Arsenault-Knudsen et al. (Citation2018) also focused on addressing safety risks related to nursing work demands; however, their study aimed to evaluate a range of physical, mental, psychosocial, and shiftwork demands. Nursing work is widely recognized as hazardous, as nurses experience relatively high rates of work-related injuries and decreased well-being compared to other types of health professionals. Yet, an understanding is lacking of the simultaneous, cumulative, and interacting exposures to different types of demands that nurses experience during work. This lack of information limits the design and implementation of potential system-based programs to improve nurse health, safety, and performance, as well as patient safety. Results of their study confirmed that hospital nurses are exposed to a variety of demands and that the levels and types of demands vary between nurses, as well as within and between work shifts. This work may help to guide more robust exposure assessment tools in nursing and the design of safety systems for this group of health professionals.
Milloy and Bubric (Citation2018) also engaged nurses as critical, front-line users in their work on optimizing and standardizing a crash cart configuration used for responding to cardiac or respiratory arrest emergencies in clinical environments. Their paper demonstrates how human factors can be used to inform and improve the design of this type of healthcare technology. Following an iterative, user-centered design process, nurses evaluated the usability of the new cart design and reported positive perceptions of usability and acceptance of the new design. The methods employed in this would can be used as a guide for other organizations.
Two papers examined how system design features can impact task efficiency and performance. In the first, Weiler et al. (Citation2018) completed a laboratory simulation study to evaluate how exam room layouts, and particularly the configuration of computer equipment, impact providers’ efficiency, errors, patient-centeredness, and situation awareness during a simulated outpatient visit scenario. A mobile computer set-up changed provider/patient interactions, decreased provider workload, and increased ratings of situation awareness, compared to a traditional exam room design with a fixed computer monitor and workstation. In contrast to many of the papers in this issue, which focused on caregivers or direct patient care tasks, Xie et al. (Citation2018) assessed how work system factors – such as the type of unit, patient or family member presence in the room, and interruptions – impacted the performance of environmental care associates during hospital patient room cleaning processes. Their paper in particular highlights the range of personnel implicated in the design of the HCS; in this case, cleaners who play a critical role in infection control.
Four papers applied a systems approach to the improvement of various parts of complex healthcare systems through the use of multidisciplinary teams including human factors, safety science, and systems engineering experts (Bargal et al., Citation2018; Benda et al., Citation2018; Ibrahim Shire et al., Citation2018; Podtschaske et al., 2018). Podtschaske et al. (Citation2018) demonstrated how a human-centered design approach can be applied successfully at the organizational level in one US healthcare system. Their paper highlights the importance of running a program encompassing multiple models, methods, and stakeholders. These authors present two exemplar projects that focused on improving blood administration and cerebrospinal fluid drainage systems. Results from this work indicate that their organization-wide endeavor led to the redesign of IT systems, medical devices, and nursing procedures, and led to improvements in both safety and efficiency. In a different systems approach, Bargal et al. (Citation2018) applied one specific method – the Systems Theoretic Process Analysis (STPA) – to a specific project on an opioid prescribing process improvement in a US urban primary care clinic. This latter work identified 16 process improvement suggestions encompassing both technology and human elements, and highlights potential challenges that can occur when implementing some process changes without significant upper-level management support.
Two other papers using a systems approach highlighted the need for better staff workload management in healthcare and attempt to address the workload issue. Ibrahim Shire et al. (Citation2018) explored the potential of a system dynamics simulation approach to workload management of hospital pharmacy staffing levels. Their study demonstrates that system dynamics can provide practical insights into staffing level management in a hospital pharmacy, by accounting for dynamic factors and tradeoffs between dispensing backlog and errors. An interesting finding from their simulation-based scenario testing is that a flexible staffing level arrangement, which dynamically adjusts the number of staff to demand variability during winter pressure, was is less effective at reducing the amount of rework than maintaining an equivalent-fixed staffing level. Finally, Benda et al. (Citation2018) designed and tested a novel display for visualizing and coordinating emergency medicine physician and nurse workload. They developed an algorithm conceptualizing multiple drivers of ED clinician workload, and utilized real-time data passively aggregated from EHR to reflect patient-related factors in their workload visualization. This study highlights the importance of involving a multidisciplinary team, including developers, informaticists, human factors experts, and users.
While the summary shown in suggests that no single study addresses all aspect of human factors and both human and system effects directly, it can be seen that, as a set, the research spans all of these dimensions. There may be a lesson in this for researchers: no one study can grasp all the complex issues in HCSs completely, and thus every study has limitations. In particular though, the paucity of studies considering psychosocial factors seems to be a gap in this sample – a concerning absence if this is true of HCS engineering research in general. Taken as a whole, however, the papers in this special issue demonstrate how multiple studies are contributing to a more complete and sophisticated understanding of how HSCs can be designed in ways that provide superior results, and that provide the best solutions for healthcare personnel and hence for patients. There will always be a need to integrate results found from across a variety of studies to gain a more complete and sophisticated view of how to design safe, efficient, and effective healthcare systems. Put another way, this analysis illustrates that the road to success is not the greatness of individual studies, but rather by establishing a broader cooperation providing united front to the challenges that face us in a global society. Researchers and decision makers working in this challenging area need to consider human factors broadly in the design of healthcare systems if they are to contribute to creating safe and efficient systems that meet the needs of system personnel, so they can provide efficient and high-quality care to patients.
A companion special issue of the IISE Transactions on Healthcare Systems Engineering is available (https://www.tandfonline.com/loi/uhse20), entitled “Advanced Sensing, Systems Modeling, and Ergonomics for Smart and Connected Health”. This special issue includes the following papers, which might be of interest to the reader.
Scheduling appointments for multiple classes of patients in presence of unscheduled arrivals: Case study of a CT department
Bhattacharjee, P., & Ray, P.
Remote physiological monitoring in a Mars analog field setting
Hill, J., Caldwell, B., Downs, M., Miller, M., & Lim, D.
Geographic modeling of best transport options for treatment of acute ischemic stroke patients: Applied to policy decision making in the USA and Northern Ireland
Kamal, N., Wiggam, M., Holodinsky, J., Francis, M., Hopkins, E., Frei, D., Baxter, B., Williams, M., Nygren, A., Goyal, M., Hill, M., & Jayaraman, M.
Inventory management strategies for mitigating unfolding epidemics
Paul, S., & Venkateswaran, J.
Detect depression from communication: How computer vision, signal processing, and sentiment analysis join forces
Samareh, A., Jin, Y., Wang, Z, Chang, X., & Huang, S.
Empirical Bayes transfer learning for uncertainty characterization in predicting Parkinson's disease severity
Zou, N., & Huang, X.
References
- Aiken, L. H., Sloane, D. M., Clarke, S., Poghosyan, L., Cho, E., You, L., … Aungsuroch, Y. (2011). Importance of work environments on hospital outcomes in nine countries. International Journal for Quality in Health Care, 23(4), 357–364. doi:10.1093/intqhc/mzr022
- Arsenault-Knudsen, É. N., Brzozowski, S. L., & Steege, L. M. (2018). Measuring work demands in hospital nursing: A feasibility study. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1509910
- Bargal, B., Benneyan, J. C., Eisner, J., Atalay, A. J., Jacobson, M., & Singer, S. J. (2018). Use of systems-theoretic process analysis to design safer opioid prescribing processes. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1521887
- Benda, N. C., Blumenthal, H. J., Hettinger, Z., Hoffman, D. J., LaVergne, D. T., Franklin, E. S. … Bisantz, A. M. (2018). Human factors design in the clinical environment: Development and assessment of an interface for visualizing emergency medicine clinician workload. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1522392
- Bourbonnais, R., Comeau, M., Vézina, M., Dion, G. (1998). Job Strain, Psychological Distress, and Burnout in Nurses. American Journal of Industrial Medicine, 34, 20–28.
- Broberg, O. (1997). Integrating ergonomics into the product development process. International Journal of Industrial Ergonomics, 19(4), 317–327. doi:10.1016/S0169-8141(96)00041-8
- Carayon, P., Bass, E. J., Bellandi, T., Gurses, A. P., Hallbeck, M. S., & Mollo, V. (2011). Sociotechnical systems analysis in health care: A research agenda. IIE Transactions on Healthcare Systems Engineering, 1(3), 145–160. doi:10.1080/19488300.2011.619158
- Carayon, P., Hundt, A. S., Karsh, B., Gurses, A., Alvarado, C., Smith, M., & Brennan, P. F. (2006). Work system design for patient safety: The SEIPS model. Quality and Safety in Health Care, 15(Suppl. 1), i50–i58. doi:10.1136/qshc.2005.015842
- Doss, R., Robathan, J., Abdel-Malek, D., & Holmes, M. W. R. (2018). Posture coaching and feedback during patient handling in a student nurse population. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1428838
- Helander, M. (2006). A guide to human factors and ergonomics (2nd ed.). Toronto ON, Canada: Taylor & Francis.
- Hinderer, K.A., VonRueden, K.T., Friedmann, E., McQuillan, K.A., Gilmore, R., Kramer, B., Murray, M. (2014). Burnout, Compassion Fatigue, Compassion Satisfaction, and Secondary Traumatic Stress in Trauma Nurses, Journal of Trauma Nursing, 21, 160–169.
- Holden, R. J., Carayon, P., Gurses, A. P., Hoonakker, P., Hundt, A. S., Ozok, A. A., & Rivera-Rodriguez, A. J. (2013). Seips 2.0: A human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics, 56(11), 1669–1686. doi:10.1080/00140139.2013.838643
- Ibrahim Shire, M., Thomas Jun, G., & Robinson, S. (2018). A system dynamics approach to workload management of hospital pharmacy staff: Modelling the trade-off between dispensing backlog and dispensing errors, IISE Transactions on Occupational Ergonomics and Human Factors.
- IEA Council (2014). Definition and domains of ergonomics. In: Secondary IEA Council (Ed.), Secondary definition and domains of ergonomics. International Ergonomics Association. http://www.iea.cc/whats/index.html
- Kieft, R. A. M. M., de Brouwer, B. B. J. M., Francke, A. L., & Delnoij, D. M. J. (2014). How nurses and their work environment affect patient experiences of the quality of care: A qualitative study. BMC Health Services Research, 14, 249.
- Kolus, A., Wells, R., Neumann, P. (2018). Production Quality and Human Factors Engineering: A Systematic Review and Theoretical Framework. Applied Ergonomics, 73, 55–89.
- MacDonald, V., & Keir, P. J. (2018). Assessment of musculoskeletal disorder risk with hand and syringe use in chemotherapy nurses and pharmacy assistants. IISE Transactions on Occupational Ergonomics and Human Factors, 1–15. 02698. doi:10.1080/24725838.2018
- Milloy, S., & Bubric, K. (2018). A four-stage method for optimizing and standardizing a crash cart configuration. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1434574
- Moon, S. D., & Sauter, S. L. (1996). Beyond biomechanics: Psychosocial aspects of musculoskeletal disorders. London: Taylor & Francis.
- Neumann, W. P., Winkel, J., Medbo, L., Magneberg, R., & Mathiassen, S. E. (2006). Production system design elements influencing productivity and ergonomics. International Journal of Operations & Production Management, 26, 904–923. doi:10.1108/01443570610678666
- Neumann, W. P., & Village, J. (2012). Ergonomics action research II: A framework for integrating Hf into work system design. Ergonomics, 55(10), 1140–1156.
- Podtschaske, B. V., Salazar, N., & Rao, M. B. (2018). Proactive, transdisciplinary safer-system redesign. A field report from the hospital frontline. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1450794
- Poghosyan, L., Clarke, S.P., Finlayson, M., Aiken, L.H. (2010). Nurse Burnout and Quality of Care: Cross-National Investigation in Six Countries, Research in Nursing & Health, 33, 288–298.
- Salmon, P. M., & Read, G. J. M. (2018). Using principles from the past to solve the problems of the future: Human factors and sociotechnical systems thinking in the design of future work. Human Factors and Ergonomics in Manufacturing & Service Industries, 28, 277–280. doi:10.1002/hfm.20777
- Spence Laschinger, H. K., Shamian, J., & Thomson, D. (2001). Impact of magnet hospital characteristics on nurses' perceptions of trust, burnout, quality of care, and work satisfaction. Nursing Economics, 19, 209–219.
- Weiler, D. T., Satterly, T., Rehman, S. U., Nussbaum, M. A., Chumbler, N. R., Fischer, G. M., & Saleem, J. J. (2018). Ambulatory clinic exam room design with respect to computing devices: A laboratory simulation study. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1456988
- Xie, A., Rock, C., Hsu, Y.-J., Osei, P., Andonian, J., Scheeler, V. … Gurses, A. P. (2018). Improving daily patient room cleaning: An observational study using a human factors and systems engineering approach. IISE Transactions on Occupational Ergonomics and Human Factors, 1. doi:10.1080/24725838.2018.1487348
