?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
This study addresses the problem of optimizing composition and distribution of an ambulance fleet within an existing emergency medical system. The primary objective is to formulate a strategy aimed at minimizing response times and enhancing the system's responsiveness, particularly to critically ill patients. The optimal spatial distribution of various types of vehicles is proposed using a hierarchical p-median model. The effects of these strategies are evaluated through a detailed computer simulation model. Experimental studies have shown that optimizing station locations contributes more significantly than altering the fleet composition and associated dispatching protocols. In the context of the Slovak Republic, the proportion of high-priority incidents responded to within eight minutes could be increased by 8.7% in urban areas and 10.5% in rural areas, solely through optimal deployment of currently active ambulances. An additional improvement of nearly 2% could be achieved by introducing 13 patient transport ambulances, optimally distributed throughout the country.
Disclaimer
As a service to authors and researchers we are providing this version of an accepted manuscript (AM). Copyediting, typesetting, and review of the resulting proofs will be undertaken on this manuscript before final publication of the Version of Record (VoR). During production and pre-press, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal relate to these versions also.1. Introduction
Emergency Medical Services (EMS) aim to deliver pre-hospital medical care to individuals experiencing injuries, heart attacks, or other acute health issues. Immediate first aid is essential, particularly in life-threatening situations where each minute of delay decreases patients' survival and recovery chances (Bürger et al., 2018). Despite this, EMS accessibility has worsened over the past two decades in many developed countries, primarily due to increasing demand (Lowthian et al., 2011; Kitić Jaklič and Kovač, 2015). For instance, in Slovakia, New Zealand, and the canton of St. Gallen, Switzerland, there was a rise in ambulance trips by 18%, 16%, and 35%, respectively, over the past decade (Karaš et al., 2017; Annual reports of the EMS Command and Control Centre of the Slovak Republic; Annual reports of Hato Hone St John; Strauss et al., 2021). Although the global COVID-19 pandemic contributed to this phenomenon since early 2020 (Annual reports of Hato Hone St John; Moskatel and Slusky, 2023), long-term growth primarily results from an aging population. Elderly individuals, who are more prone to sudden health deteriorations and injuries, represent an increasing proportion of the population. Other factors escalating EMS demand include shortages of general and specialized doctors and a lack of alternative transportation means for elderly or immobile patients to reach medical facilities.
Each EMS typically follows a service process comprising the following four main steps: (i) receiving an emergency call and evaluating the situation, (ii) dispatching an ambulance or multiple ambulances to the scene if required, (iii) providing on-scene treatment, and (iv) transferring the patient to an appropriate hospital, if necessary, then returning to a station or other emergency sites. During telephone triage, medical emergency call-takers typically assign one of three priorities to each call: (1) high priority, designated for patients who are evidently in life-threatening conditions and likely to die without immediate medical intervention; (2) medium priority, for patients with urgent and potentially life-threatening conditions; and (3) low priority, for non-urgent patients whose lives are not immediately threatened. Emergency ambulance personnel are entitled to provide basic life support (BLS) or advanced life support (ALS) services. BLS ambulances are staffed by paramedics, while ALS ambulances usually have a physician on board who can perform additional life-saving procedures, such as inserting breathing tubes. EMS may also be supplemented by patient transport services (PTS) responsible for transporting non-urgent patients to hospitals.
EMS responsiveness depends on several factors: (i) the EMS system infrastructure, including the number and distribution of operating ambulances in the region; (ii) the dispatching process; and (iii) the density and quality of the road network. The dispatching process is closely tied to the ambulance fleet composition in terms of their equipment and staff qualifications. In this paper, we focus on the EMS system infrastructure, specifically the locations of ambulance base stations, and the composition and distribution of the EMS vehicle fleet. We suppose that the dispatching process is determined by emergency protocols and together with the road network are exogenous inputs to our study. We focus on land ambulances and omit air medical services. We propose several strategies to enhance EMS performance, and we evaluate the resulting performance quality indicators through computer simulation. Our motivation stems from the goals outlined in the document (Next Generation EU: Pandemic Recovery Plan, 2021) to create a greener, more innovative, and stronger Europe. Any reforms to improve service quality must account for the shortage of emergency professionals, implying that the current number of emergency ambulances will not increase. With this limitation, we see three potential ways to reduce response times by improving fleet management and composition: (i) redistributing emergency ambulances across the country, (ii) changing ambulance types, and (iii) shifting part of non-urgent trips to PTS. Although we apply these strategies in the context of Slovakia, we assess their impact relative to the current system's performance. We believe the conclusions are universal and can be applied to any country with a similar EMS system (Emergency medical services systems in the European Union, 2021).
2. Literature Review
Operations research literature offers a wealth of prescriptive and descriptive models that support decision making for all aspects of EMS planning (Aringhieri et al., 2017). The optimization of existing base station locations, where idle ambulances await dispatch, represents an evident measure to enhance service accessibility with moderate investments (Strauss et al., 2021). Given that these stations can be established in existing buildings such as healthcare facilities, shopping centers, or schools, the costs associated with station redeployment are reasonably affordable. For a comprehensive overview of basic optimization location models, please refer to (Drezner and Hamacher, 2004). Surveys conducted by Bélanger et al. (2019) and Ahmadi-Javid et al. (2017) have predominantly focused on healthcare facility location models and those related to ambulance fleet management. When optimizing ambulance locations, two common criteria emerge: (i) maximizing the number of requests served within a specified time standard, and (ii) minimizing the average response time. These criteria align with the performance standards preferred by EMS managers and policymakers across different countries. Models aimed at minimizing response time are typically variants of well-known location-allocation models widely utilized in supply chain design (Melo et al., 2009). Several studies have experimentally confirmed that solutions minimizing response time outperform those maximizing coverage (Toro-Díaz et al., 2015; Jánošíková et al., 2021). Additionally, Felder and Brinkmann (2002) emphasize that public policy should prioritize minimizing the average response time, as the survival rate is inversely proportional to the response time.
Most ambulance location models consider a homogeneous fleet of vehicles. However, in practice, emergency services are typically provided by a heterogeneous fleet. Rare exceptions dealing with a heterogeneous fleet include the papers (McLay, 2009) and (Hammami and Jebali, 2019), which optimized the distribution of BLS and ALS non-transport quick response vehicles. Andersson et al. (2020) experimented with decreasing the number of ambulances, assuming that non-urgent calls would be served by specialized transport vehicles. The models proposed by McLay (2009) and Andersson et al. (2020) are probabilistic models that address uncertainty in ambulance availability, employing queuing theory to manage this uncertainty. The probability that an ambulance will be occupied when needed is referred to as the busy fraction. Its calculation relies on the system-wide average service time, which can be accurately estimated only in a small, homogeneous region. However, this concept becomes less applicable in systems operating across geographically widespread areas, serving patients of various categories, where the dispersion of service times is substantial. Another approach within stochastic models deals with randomness in requests rather than ambulance availability, as observed in the works of Beraldi and Bruni (2009) and Bertsimas and Ng (2019). Nonetheless, these models are computationally demanding, sensitive to parameter settings, and their practical applicability has not been substantiated by case studies. Hence, we opted for a discrete location-allocation model in this study.
Mathematical programming models reflect reality with a high level of abstraction. Because they cannot encompass all aspects of the stochastic nature of the EMS system, their objective function value is only a rough estimate of a performance indicator. A more accurate picture of system performance can be obtained using a detailed computer simulation model (Henderson and Mason, 2004; Aboueljinane et al., 2013; Strauss et al., 2021; Ridler et al., 2022). Moreover, unlike a mathematical programming model, computer simulation allows for the evaluation of multiple performance criteria, such as response time, the fraction of calls responded to within different time limits, pre-hospital time, vehicle utilization rate, or total mileage (Aboueljinane et al., 2013; Strauss et al., 2021). The paper by Aboueljinane et al. (2013) is an excellent review of simulation models applied to emergency medical service operations, covering four decades, beginning with the 1970s. The simulation studies are reviewed in terms of the decisions they address, the performance measures used, modeling of demand, processing and travel times, and verification and validation techniques. Most studies reviewed in Aboueljinane et al. (2013), as well as those published later, e.g., Strauss et al. (2021); Olave-Rojas and Nickel (2021), reported simulation experiments within the framework of a what-if analysis, without any connection to an optimization tool. However, the rapid advancement in computing power, the development of high-performance mathematical programming solvers, and the increasing availability of high-quality data have enabled the creation of efficient optimization procedures and detailed simulation models for evaluating deployment scenarios (Zaffar et al., 2016; van den Berg and van Essen, 2019; Jánošíková et al., 2019; Jánošíková et al., 2021). This study follows this trend.
In this research, we propose several modifications to the distribution, composition, and management of the EMS vehicle fleet with the aim to improve the responsiveness of the EMS system. The proposed strategies include:
1. Optimization of the EMS station network at the countrywide level.
2. Optimization of station locations in large towns (regional capitals).
3. Introducing passenger cars staffed by a driver, who simultaneously serves as a paramedic, and an emergency doctor operating in a rendezvous (RV) mode.
4. Introducing PTS ambulances.
We use discrete optimization and mathematical programming modeling to propose the redeployment of the current EMS stations, as well as the distribution of RV and PTS vehicles. The impact of the proposed strategies on performance quality indicators is evaluated using a detailed computer simulation model. We focus on two indicators that are most important from patients' perspective: response time – defined as the interval from the assignment of an ambulance by the dispatch center to its arrival at the scene, and coverage level – defined as the proportion of patients responded to within a given time threshold. Less attention is given to the economic aspects of the proposed reforms.
The paper offers a dual contribution, both methodological and practical. Methodologically, we emphasize the significance of validating results generated by mathematical programming models through a computer simulation model, further validated using real-world data. To our knowledge, no other study has integrated optimization with validated simulation. Most studies tend to evaluate solutions solely analytically, which shares the same drawback as the optimization models themselves – it overlooks the inherent complexity of a real system. In rare instances where simulation is utilized (Zaffar et al., 2016; van den Berg and van Essen, 2019), the simulation model is often significantly simplified, serving primarily for comparing different solutions rather than evaluating their practical impact.
An additional benefit of our data-driven approach is the derivation and presentation of probability distributions of time intervals along the patient pathway. Many of these distributions are regionally independent and can be applied in similar studies anywhere. For example, on-scene treatment is a standardized procedure, therefore its duration can be modelled by probability distributions presented in Table 1 regardless of the investigated region or country. These probabilistic models can be incorporated in simulation packages such as JEMSS (Ridler et al., 2022). From a practical perspective, our study offers actionable recommendations to policymakers for implementing the most effective system improvement strategies.
3. Methodology
3.1 Optimization of Stations Locations
We are faced with the challenge of determining the optimal distribution of stations of various types in a large-scale urban-rural area (e.g., a country). Based on the reasons outlined in the Literature Review Section, we have chosen the p-median model. The p-median problem is a variant of a location-allocation problem that selects stations from a set of candidate locations to minimize the average time between each demand location and its nearest station, under the assumptions that (i) the number of stations p is predetermined, and (ii) every station serves as a stand-by site for a single ambulance. Let I denote the set of candidate locations and J the set of demand points. The demand volume bj is known for each demand location j ∈ J. The shortest travel time tij from candidate location i ∈ I to demand location j ∈ J can be estimated based on the underlying road network.
The station positions are represented by variables yi , taking the value of 1 if a station is located at candidate location i, and 0 otherwise. To calculate the average travel time between stations and demand locations, we need to assign demand zones to the located stations, i.e., to determine which station will respond to the demand at each location j. This is modeled by another set of decision variables. The decision variable xij takes the value of 1 if demand zone j is assigned to a station located at node i, and 0 otherwise.
Using this notation, the model can be written as follows:(1)
(1)
(2)
(3)
(3)
(4)
(4)
(5)
(5)
The objective function (1) expresses the total travel time taken by the ambulances to reach all patients regardless of their priorities. The average travel time is calculated by dividing the objective function value by the total volume of demand . Equations (2) ensure that each demand zone will be served. Equations (3) allow demand zone j to be assigned to candidate location i only if a station is opened at node i. Equation (4) states that exactly p stations will be located. The remaining constraints (5) specify the domains of bivalent decision variables.
We apply the model at different levels of space resolution and system hierarchy. Regarding the space resolution, we determine the ambulance distribution at the nationwide level first. All municipalities are considered potential locations for stations, and correspondingly, demands are aggregated to central nodes of these municipalities. The central node of a municipality is defined as the node on the road network that has the shortest straight-line distance to the municipality’s center. The fastest routes on the road network are used to calculate travel times between municipalities.
The volume of demand has been deduced from historical data on ambulance trips. Given that the main concern of EMS involves serious incidents that may directly threaten human lives, only high and medium priority patients were included in the demand model.
The EMS system with two levels of emergency services can be regarded as a hierarchical location system with a nested hierarchy. In this structure, a higher-level facility (ALS ambulance) offers all the services provided by a lower-level facility (BLS ambulance) and some additional services (Şahin and Süral, 2007). So, at the lower hierarchical level, we solve the model irrespective of different ambulance types. However, the number of stations to be located must be reduced because some stations must remain in their current positions. The reason is that the model neglects service times and assumes ambulances are always ready to respond immediately. Therefore, to the model, it seems that ambulances have unlimited capacities, and it makes no sense to locate multiple stations at the same candidate location i (the second station at the same node i does not decrease the objective function value). However, this would lead to a practically infeasible solution because the workload of stations located in highly populated municipalities would be enormous, and as a result, the response times would rise above an acceptable value. Therefore, we must analyze the current distribution of stations and population distribution and fix one or more stations in large towns before optimization.
At the upper level of the hierarchy, we search for an optimal distribution of ALS stations. We redefine the set of candidate locations I to contain only those municipalities where a station has been located by the first run of the model and solve the model to minimize the average travel time of ALS ambulances to high and medium priority patients. The remaining stations from the lower level that are not selected to house an ALS ambulance will be assigned a BLS ambulance.
Once the optimal distribution of stations across the country has been determined, we proceed to calculate the optimal locations of stations in large cities, focusing specifically on regional capitals that possess multiple stations. Currently, it is common for multiple stations to share a single building due to the cost benefits. However, it is clear that, on average, patients in the region could be reached more quickly if the stations were dispersed.
The optimal distribution of stations across a city can be achieved using the same hierarchical p-median model applied at the nationwide level, although it is not desirable to fix any stations in this context. The demand model once again consists of high and medium priority patients. Compared to the nationwide level, a more detailed spatial demand pattern is required. For instance, we can overlay the city with a rectangular grid pattern. The size of the grid cells depends on the model's computability and the spatial distribution of demand. Similar to the nationwide level, demand points are the nodes on the road network that are closest to the centroids of the cells.
While the p-median model is NP-hard, it can be optimally solved within a reasonable timeframe using transformation into a coverage-type model (Janáček and Kvet, 2016).
3.2 Introducing Rapid Response Vehicles with Doctors
The introduction of rapid response vehicles with a physician onboard could enhance the system's efficiency by achieving shorter response times at lower costs. Given their capacity to drive at higher speeds than ambulances, they can reach patients more rapidly. Additionally, as EMS ambulances with special equipment are expensive, replacing some of them with passenger cars unequipped for patient transport could generate cost savings. As these cars cannot transport patients, the doctor often rendezvouses with a supporting ambulance team at the emergency site, hence the term “rendezvous system”. This system is employed in several countries, for example in Germany (Olave-Rojas and Nickel, 2021). For simplicity, we will refer to the rapid response vehicles with a doctor onboard as RV vehicles throughout the rest of the text.
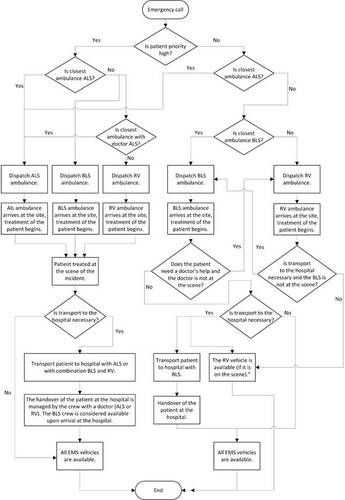
The introduction of RV vehicles necessitates changes in fleet management. The typical dispatching strategy follows this protocol: (1) for high priority calls, the closest available ambulance to the emergency site is always dispatched, regardless of its type. If a BLS ambulance is dispatched, the nearest ALS ambulance is concurrently dispatched, and the BLS ambulance becomes available after the ALS ambulance arrives; (2) for medium priority calls, the closest ambulance is dispatched; (3) for low priority calls, the nearest BLS ambulance is dispatched. If the destination is too distant, an ALS ambulance can respond to the call.
The dispatching strategy for RV vehicles differs from the one described above. RV vehicles are intended to respond only to high and medium priority calls. In the case of a high priority call, the nearest ambulance is dispatched. If the closest vehicle is a BLS ambulance, then the nearest ambulance with a doctor on board (either an RV or ALS) is dispatched concurrently. If the closest vehicle is an RV, then the nearest BLS ambulance is dispatched concurrently as well. If the BLS ambulance arrives at the scene before the RV vehicle, it waits for the doctor, with the paramedic crew assisting him until his departure.
If it is necessary to transport the patient to a hospital, both vehicles travel to the hospital and only become available again after the patient has been handed over to the hospital staff. For a medium priority call, the closest vehicle is dispatched. If it is a BLS ambulance, the crew assesses the patient’s condition and may request doctor’s support (either an ALS ambulance or an RV vehicle).
If only the RV vehicle is dispatched and the doctor determines that the patient needs to be transported to a hospital, he summons a BLS ambulance, which then transports the patient to the hospital without the doctor's accompaniment. This process is depicted in Fig. 1. For a low priority call, the nearest BLS ambulance is always dispatched.
The proposal is for RV ambulances to replace some ALS ambulances. The question then arises as to which ALS ambulances should be converted to RVs. We can again apply the p-median model, selecting candidate locations from municipalities that have an ALS station and are in close proximity to a BLS station.
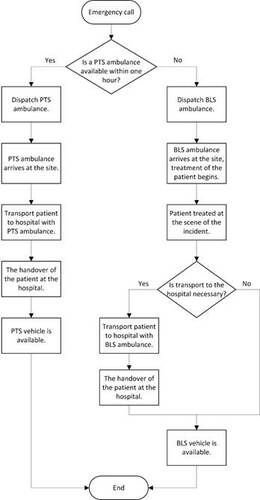
3.3 Introducing Patient Transport Ambulances
Transport ambulances are currently utilized for pre-arranged patient transport to and from healthcare appointments. The surge in the number of emergency calls, particularly those of non-urgent nature, has led public health experts to consider transferring a portion of these non-urgent calls to patient transport services. The proposed solution involves introducing transport ambulances that could operate around the clock and cater to low priority patients. It is anticipated that if a PTS ambulance is dispatched to a patient, the patient will be transported to a hospital rather than treated at home. As the patients’ condition is expected to be non-acute, their response time can be extended (up to 1 hour). Fig. 2 illustrates the dispatching protocol with PTS ambulances.
Our objective is to determine the necessary number of PTS ambulances and their optimal placement. Once again, mathematical optimization proves to be a valuable tool for solution. The minimum required number of PTS ambulances is calculated using the location set covering model (Bélanger et al., 2019; Church and Murray, 2018). This model establishes the minimum number of facilities necessary to cover every demand point. A demand point is deemed covered if it is within a predefined travel time threshold Tmax from a facility.
Using the previously defined notation, represents the set of candidate locations within the vicinity of demand location j. The model can be written as follows:
(6)
(6)
(7)
(7)
(8)
(8)
The objective function yields the number of locations, p, required to reach all demand locations within the maximum of Tmax minutes. Constraints (7) ensure that each municipality j will be covered. Constraints (8) are integrality constraints.
Models based on the coverage principle have the disadvantage of overlooking the weight of demand points. As a result, a facility may be located in a small village near a large town if it covers the same region. However, placing facilities at heavy demand points is more efficient than doing so at smaller demand points. Median-based models emphasize the efficiency of facilities, hence the p-median model should be applied subsequently. The coefficient p is set to the calculated minimum number of transport ambulances. The demands bj
comprise only low priority patients. An additional constraint (9) must be included in the p-median model (1)-(5) to ensure that the response time limit Tmax
will not be exceeded at any municipality:(9)
(9)
3.4 Computer Simulation Model
We have developed a comprehensive microscopic computer simulation model of the EMS system, calibrated using real historical data. Current data is essential for accurately depicting the temporal and spatial patterns of all ongoing processes within the EMS system. For every call we have all important times (for example arrival of the crew at the scene, arrival at the hospital,…). The simulation model is constructed using an agent-based architecture and is implemented in the Java language.
The movement of an ambulance follows the established road network. In the simulation model, an ambulance always takes the route with the shortest estimated travel time, which is determined using historical data on average ambulance speeds, factoring in the road type and time of day. Traffic delays during the morning and afternoon rush hours are also considered.
While traveling back to the station, the vehicle remains available and can be dispatched to a new patient if needed. This functionality enables the use of an agent-based approach. The simulation model accurately mimics all decisions and processes involved.
The dispatch logic in the model closely mirrors real-world practices. When an emergency call is received, the operations center staff assess the patient's condition, locate the nearest available ambulance, and dispatch it to the scene. Upon arrival, the ambulance crew provides initial treatment.
All time-related aspects are modeled using probability distributions. The service time model encompasses every phase of the ambulance journey: traveling to the patient, providing treatment at the scene, transporting the patient to the hospital, drop-off time at the hospital, and returning to the base station. At the hospital, the rescue team transfers the patient to the hospital staff and may spend additional time cleaning and resupplying the vehicle. This period, known as drop-off time, is modeled with a unique probability distribution for each hospital.
4. Case Study
We have implemented the models under the conditions specific to Slovakia. As of February 2023, the country hosts 274 stations distributed across its territory, with 85 designated as physician ALS type and the remaining 189 serving as paramedic BLS ambulance stations. Government regulations stipulate the municipalities where stations should be located but do not precisely define their exact positions. Stations are operated by both private and state providers. When a provider obtains a license to operate a station in a municipality, it locates a suitable building with a garage for the vehicle and an office for the staff. In cases where a provider holds multiple licenses in a town, these stations can share the same building. Stand-by sites other than the stations are not present.
The demand volumes used in the mathematical programming models were derived from historical data on ambulance trips spanning from January 2019 to October 2022. This data, collected by the EMS Command and Control Centre of the Slovak Republic, were provided to us in a depersonalized form. Each trip record includes timestamps, the priority level assigned to the patient by the call-taker, the patient's diagnosis, the destination hospital, and the type of ambulance. We have not considered demand elasticity, i.e., the potential influence of EMS service supply on demand. This is because accessibility to prehospital care is declining due to a decreasing number of general practitioners, making EMS the primary choice for elderly, disabled, and vulnerable individuals to receive professional first aid, even in areas with longer ambulance response times.
Travel times were calculated using the digital road network (OpenStreetMap database, 2019). The average speeds of ambulances were derived from historical GPS tracking data on ambulance movements (Jánošíková et al., 2019). Ambulance speed is contingent on the road category and whether the road is within or outside the built-up area of a village or town.
4.1 Calibration of the Computer Simulation Model
We calibrated the parameters of the simulation model using data from 435,655 EMS patients served from January to October 2022. The temporal distribution of emergency calls does not show significant variations between weekdays and weekends (Fig. 3a), nor are there noticeable monthly changes (Fig. 3b). This observation is consistent with other studies, such as Strauss et al. (2021). However, the call arrival rate fluctuates considerably throughout the day. Fig. 3c illustrates the number of trips initiated each hour of an average day. Based on this analysis, the simulated arrival of calls follows a non-homogeneous Poisson process, with a specific hourly rate.
The spatial pattern of incidents in the simulation model is also based on historical data. Incident locations are generated randomly in accordance with the number of incidents in each region and the population density data sourced from the LandScan Global database (LandScan database, 2017). This database provides realistic estimates of population distribution, reflecting people's probable locations throughout the day, not just their residential locations as reported in official censuses. In its 30 arc-seconds resolution (approximately 1 km), the database contains ambient (24-hour average) population distribution. LandScan models leverage satellite imagery, spatial data, and census data, processing them using modern geospatial technology and machine learning approaches.
The simulation model accurately replicates patient management. After a call is generated, the model assigns age, diagnosis, and priority to the patient. The probability of assigning specific characteristics is derived from the analysis of real historical data. The priority affects the dispatcher’s decision on the responding ambulance(s), as previously described. The priority correlates with the patient’s age and diagnosis, which influences the selection of the hospital to which the patient will be transported.
Hospitals have assigned attributes defining their competencies, for instance, a hospital might only admit pediatric patients or patients with specific diagnoses, such as heart diseases. This allows the selection of the nearest suitable hospital for the call type. The hospital handover time is modeled by a specific probability distribution for each hospital, where the average handover time varies between 12.9 to 31.7 minutes. Additionally, the patient's diagnosis influences the duration that a crew spends at the incident site. The on-scene time is modeled separately, also employing a specific probability distribution for each combination of diagnosis group and crew qualification (Table 1).
In the model, ambulances are expected to follow the fastest routes. To provide more accurate estimates of travel times, we utilized up-to-date GPS traces of ambulance trips, which in turn enhanced the model’s effectiveness. These routes are computed during the simulation as soon as the journey’s origin and destination are known. Travel times are deterministic and vary over time. Vehicle speeds are set for different periods of the day and ambulance travel modes (regular, or with lights and sirens activated). Speeds are decreased during peak hours (from 6:30 to 9 am and from 3 to 6 pm). On the contrary, speeds increase when the ambulance is rushing to a patient or transporting a patient with lights and sirens activated. Therefore, the travel time along a route depends on the travel mode and the trip’s start time. Additionally, the road category is assessed, and the simulation model verifies whether the road is within the city boundaries.
In the agent-based architecture, the status of the ambulance (e.g., idle, travelling with lights and sirens, returning to the station, providing on-scene treatment, etc.) and its current geographical position are known at any moment. This feature facilitates the modeling of en-route redispatching, which means that the ambulance does not need to return to the base station after completing a service but can be dispatched to another call while travelling back.
In addition to responding to emergency calls, emergency ambulances also carry out secondary transports of patients. Secondary transports include transfers of patients between hospitals and, on rare occasions, planned transports to healthcare appointments. Currently, 23.8% of secondary transports are performed by emergency ambulances. Although secondary transports account for only 2.2% of all trips, we do not neglect them; instead, they are incorporated into the simulation model.
Most of the behavior described above is captured in simulation tools used in emergency systems worldwide. However, our simulation model has some unique features not present in the state-of-the-art simulation models, like those in Strauss et al. (2021), Olave-Rojas and Nickel (2021), and Ridler et al. (2022). These features include:
• additional attributes assigned to calls and hospitals, such as the patient’s age and diagnosis;
• the duration of on-scene treatment depends on the patient’s condition and the intervening team;
• secondary transports;
• cooperation of multiple intervening teams only occurs in Olave-Rojas and Nickel (2021).
The simulation model was verified and validated through consultations with medical experts and by comparing the average response times to actual statistics from the real system (Table 2). The model yields slightly more optimistic results compared to the real system because some processes had to be neglected due to the lack of reliable data, e.g., technical breaks of vehicles. However, the differences are so small that we consider the model valid.
The simulation model allows for the evaluation of most ambulance quality indicators monitored by the EMS authorities. In the numerical analysis in Section 4.2, we focus on the following system indicators:
1. Average response time, evaluated separately for each patient's priority.
2. Percentage of high priority calls responded to within eight minutes.
3. Percentage of high and medium priority calls responded to within 15 minutes.
4. Percentage of low priority calls responded to within 15 minutes.
The National Recovery and Resilience Plan, which constitutes the Slovak part of the Next Generation EU pandemic recovery plan, sets the target of reaching 80% of high priority incidents within eight minutes and 90% of high and medium priority patients within 15 minutes.
4.2 Optimization and simulation results
The optimal distribution of ALS and BLS stations across the country, as well as in regional capitals, was calculated using the hierarchical p-median model (1)-(5). This model exhibits certain limitations, with the primary drawback being the assumption that the nearest ambulance is always available and prepared to respond immediately to a call. Consequently, the average response time calculated by the model is not realistic; instead, it represents a lower bound of the actual response time. This rough estimate requires refinement through computer simulation. Table 3 illustrates the theoretical Average Response Time (ART), calculated by summing the demand-weighted average travel time and the preparation time elapsed between the ambulance receiving the notification and departing from the station. The preparation time is assumed to be one minute.
A previous financial analysis suggested replacing 23 ALS ambulances with RV ambulances. ALS stations to be switched to RV stations were also selected by the model (1)-(5).
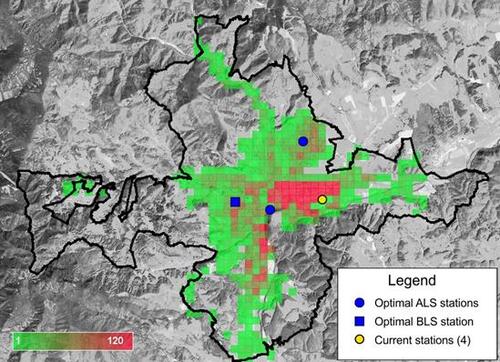
As for the third design of the ambulance fleet, the minimum number of transport ambulances required to cover every municipality within an hour was calculated by the mathematical programming model (6)-(8), resulting in 13 PTS ambulances. Their optimal distribution was determined by the p-median model (1)-(5) with the additional constraint (9).
The computational experiments were performed on a PC with an Intel® Core™ i7 5500U processor, 2.4 GHz and 16 GB RAM. The optimization software FICO XPRESS 8.0 (64-bit, release 2016) was used to solve the location models.
Different configurations of the ambulance fleet were evaluated in a simulation study. Each configuration represents one scenario for the simulation experiment. Thus, the following scenarios were simulated:
1. Current deployment (February 2023) of the stations.
2. Optimal deployment of 85 ALS stations and 189 BLS stations (including optimization in regional capitals).
3. Optimal deployment of 62 ALS stations, 189 BLS stations, and 23 RV stations.
4. Optimal deployment of 85 ALS stations, 189 BLS stations, and 13 transport ambulance stations.
The replication method was used to estimate means and confidence intervals of the performance measures mentioned in the previous section. One replication simulated 91 days of system operation. For every configuration of the fleet, 10 replications were performed. The mean values of the performance indicators are reported in the following tables. Table 4 provides the values of the indicators for the whole country, while Tables 5 and 6 pertain to urban and rural areas, respectively. Urban areas are territories of those municipalities that are declared as towns by the National Council of the Slovak Republic. The towns are economic, administrative and cultural centers, and have at least 5000 inhabitants.
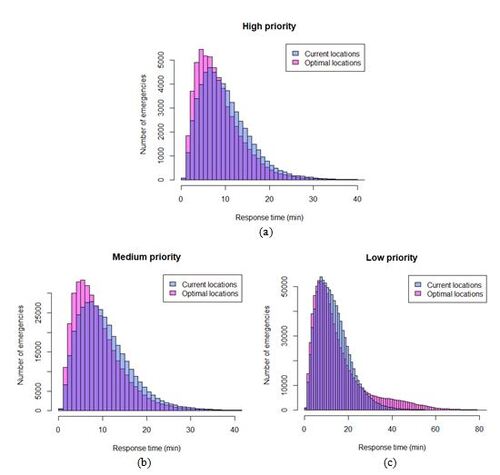
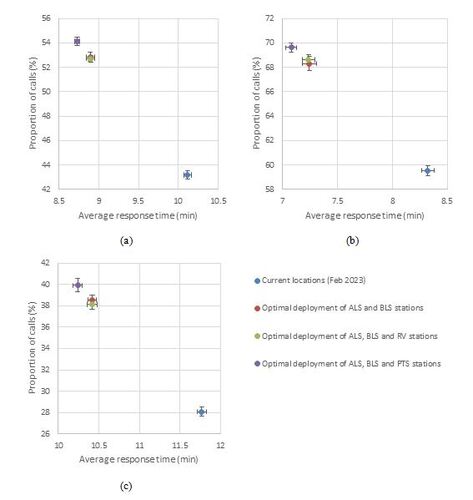
The differences among the fleet configurations are illustrated by Figure 4, which shows the coverage level against the average response time for high priority calls and the 8-minute target.
As evident from the tables and figures, optimizing the station locations proves to be more beneficial than altering the fleet composition. At the nationwide level, the average response times (ARTs) are 1.3 minutes shorter with the optimal distribution of the ALS and BLS ambulances compared to the current infrastructure. When comparing urban and rural areas, the optimization impact is more pronounced in rural regions. In rural areas, the reductions in ARTs are 1.4, 1.4, and 1.7 minutes for high, medium, and low priority calls, respectively. Changes in the fleet composition have only marginal effects relative to the optimization. Introducing rapid response RV vehicles, following the dispatching protocol depicted in Figure 1, does not improve the system indicators. The primary reason is that doctor’s cars are not equipped for passenger transport; therefore, a BLS ambulance must be dispatched concurrently when transport to a hospital is needed, thereby reducing the availability of BLS ambulances for other calls. RV vehicles are only justifiable from an economic perspective, as they are cheaper than ambulances.
Further reduction in response time is possible by introducing an additional 13 PTS ambulances to serve a portion of the low priority calls. Utilizing these ambulances will reduce the workload of BLS ambulances, making them available as first responders to high and medium priority calls. The ART for these two groups of patients is approximately 10 seconds shorter with PTS ambulances than without them, representing a statistically significant improvement. Additionally, the coverage for high and medium priority patients is the best with this fleet composition. On the downside, the ART for low priority patients increases by almost four minutes, and there are even patients who must wait more than an hour. However, even a small improvement for high and medium priority patients can save lives, so it is worth the trade-off for low priority patients whose lives are not in immediate danger. Of course, this strategy assumes that the severity of the call is evaluated with a low rate of classification errors. The induced investment costs would not be very high, as PTS ambulances need not be equipped with life-saving devices. Histograms of calls responded to within a time threshold provide a more detailed view of the impact of optimization and fleet restructuring. Figure 5 displays the histograms of the simulated calls for the current distribution of the stations and the optimal deployment of ALS, BLS and PTS ambulances. We observe a higher proportion of high and medium priority calls being responded to within 8-minute and 15-minute targets by ambulances optimally distributed throughout the country. However, the introduction of PTS ambulances results in an increased number of low priority calls experiencing relatively long response times, approaching an hour.
The optimization of the station network in regional capitals has led to a considerable reduction in response times within the cities, particularly for high-risk patients. The most significant improvement is observed in Banská Bystrica. At present, there are two ALS and two BLS stations located at the same address outside the city center. The optimization model suggests relocating these to different areas throughout the city, reducing the number of stations to two ALS and one BLS stations. Despite the decrease in the number of stations, the response times to high and medium priority calls are shortened by six minutes, and for low priority calls, by 40 seconds. The proportion of high priority cases covered within eight minutes increases dramatically from 18.3% (according to real data from 2022, it is 21.3%) to 89.6%. Figure 6 illustrates the distribution of demand within the city in the simulation model, as well as the current and optimal locations of the stations.
Comparing our results with other EMS systems worldwide is instructive. For instance, performance targets in England do not distinguish between urban and rural areas. The national standard mandates that ambulances respond to high priority (Category 1) calls in seven minutes on average and respond to 90% of them in 15 minutes (Ambulance response times, 2023). With our fleet containing PTS ambulances, we nearly meet these targets, with an ART of 8:44 minutes and 88% of calls responded to within 15 minutes. This aligns with official statistics from the National Health Service in England, which show that in March 2023, the ART was 8:49 and the 90th percentile was 15:38 (Ambulance Quality Indicators Data 2022-23, 2023). For medium priority (Category 2) calls, ambulances must respond in 18 minutes on average, and respond to 90% of calls in 30 minutes. The Category 2 average in March 2023 was 39:33, and the 90th percentile was 1:26:15. The Slovak system provides better quality services for this patient class.
EMS accessibility is better in urban areas than in rural settlements, where the distances between stations, patients’ locations, and hospitals are longer. This is reflected in different performance targets for urban and rural areas in some countries. For instance, in New Zealand, the urban targets state that 50% of high priority (purple) incidents should be reached within six minutes, and 50% of medium (red) priority incidents within eight minutes (Annual reports of Hato Hone St John, 2023). Rural targets are 10 and 12 minutes for high and medium priorities, respectively. According to the report for the year between 1 July 2021 and 30 June 2022, the actual urban coverage was below the target (47.1% and 39.5%, respectively), while rural coverage was higher, specifically 53.8% and 44.2% for high and medium priorities, respectively. In Slovakia, urban 6-minute coverage of high priority calls is 41.9% with the current infrastructure and could be increased to 53.4% with optimal distribution of ALS and PTS ambulances. Urban 8-minute coverage of medium priority patients is 56.2% currently, and with the best fleet strategy, it could reach 67.4%. Rural 10-minute coverage of high priority calls is currently 44.5% with a potential increase to 57.1%. Rural 12-minute coverage of medium priority patients is 55.7%; introducing PTS ambulances could result in 67.3%.
Although the proposed strategies for the ambulance fleet could improve the performance of the EMS system, the targets stated in the National Recovery and Resilience Plan cannot be achieved at the nationwide level. The optimal distribution of ambulances will meet the 15-minute target for high and medium priorities only in urban areas. Strong thresholds are desirable from a medical perspective, but they are challenging to achieve with limited resources. At the nationwide level, 43.2% of high priority patients have a response time below eight minutes. This fraction could be increased to 54.1%. A similar 8-minute coverage of about 40% in mixed urban-rural areas is reported in other studies, for example, McLay and Mayorga (2013). To achieve more than 80% coverage would necessitate a high density of ambulances.
5. Conclusions and Future Work
This article presents several strategies in ambulance management and fleet composition, aiming to enhance the responsiveness of the EMS system for critical patients. The impact of these strategies on system quality indicators is assessed using a detailed computer simulation model and real-world data. The results suggest that optimizing the deployment of the stations has a greater impact than introducing rapid response vehicles for doctors. Response times for high and medium priority incidents can be further reduced by incorporating transport ambulances to serve low priority patients.
The outcomes of our study support strategic as well as tactical decisions made by EMS managers and urgent health care providers. Our approach can be applied to any region with diverse geography, varied road network quality, and uneven population density, where a tiered EMS system with different types of vehicles operates based on the Franco-German model. Such systems are common in many European countries, including Germany (Strauss et al., 2021), Hungary (Gondocs et al., 2010), Poland (Sagan et al., 2016), and Austria (Fritze et al., 2018), among others. The proposed methodology is universal and can be directly applied to solve the problems of fleet composition and distribution in different countries. The only components that depend on the specific territory are related to the calibration of the optimization and simulation model and include the temporal and spatial distribution of emergency calls, certain dispatching protocols, road infrastructure, and the network of hospitals.
We acknowledge that our research has certain limitations. Our mathematical programming models only include central nodes of municipalities or grid elements in the sets of potential locations, which does not take into account practical considerations such as the availability of suitable facilities, leasing costs, and connectivity to the road network. Thus, the solutions derived from the models should be interpreted in terms of the zones surrounding the calculated optimal station locations, rather than the precise addresses of the stations. Nonetheless, this interpretation is beneficial for decision-makers as our aim was to estimate potential improvements resulting from changes in the ambulance fleet, rather than to determine the exact locations of the stations. Furthermore, we did not take into account the costs associated with closing existing stations and opening new ones due to the optimization of station locations. Economists will conduct a financial analysis of the proposed changes, which may result in limitations on the number of stations that can be relocated or requirements for certain stations to remain at their current locations. These additional requirements can be integrated into the models by appropriately modifying the parameter p and fixing certain variables yi .
One key input parameter that influences not only the optimal locations but also the simulation results is the travel time across the road network, which depends on the average speed of the ambulances. In our study, we used relatively old estimates of speeds provided by the Falck company for ambulances. We applied the same speed profiles for RV vehicles, despite the fact they are expected to travel at higher speeds than ambulances. However, we anticipate acquiring up-to-date GPS traces of ambulance trips in the future and deriving more accurate estimates, similar to the approach taken in Buzna and Czimmermann (2021).
Acknowledgements
The authors acknowledge the generous support from the Slovak Research and Development Agency, grant number APVV-19-0441, and from the Scientific Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic and the Slovak Academy of Sciences, grant number VEGA 1/0216/21.
Disclosure statement
The authors report there are no competing interests to declare.
Data availability
The data that support the findings of this study are available at https://zenodo.org/records/12766103.
Table 1. Probability distribution and the average on-scene time for different types of ambulances.
Table 2. Actual and simulated average response times (ART) in Slovakia.
Table 3. Theoretical average response times for the optimal network of ALS and BLS stations.
Table 4. Simulation results for Slovakia.
Table 5. Simulation results for urban areas.
Table 6. Simulation results for rural areas.
Figure 3. (a) The ratio of the number of trips on individual days to the daily average; (b) The ratio of the number of trips in individual months to the monthly average; (c) The average number of trips per hour.
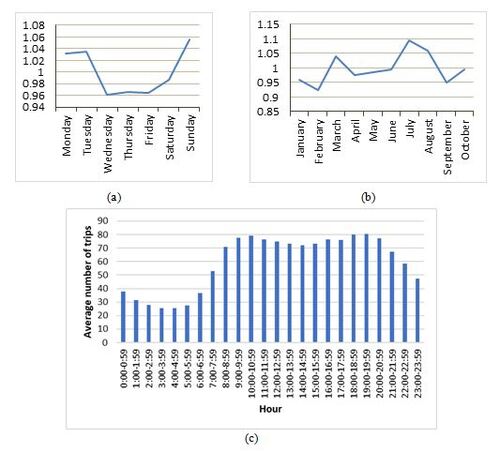
Figure 4. Proportion of high priority calls responded to within 8 min against the average response time. Error bars are 95% confidence intervals. (a) Slovakia; (b) urban areas; (c) rural areas.
Reproducibility Report
Download PDF (191.7 KB)Additional information
Notes on contributors
Peter Jankovič
Peter Jankovič (ORCID 0000-0002-0005-8128) is a highly skilled professional with expertise in the field of Applied Informatics. He graduated from the University of Žilina, majoring in Information and Control Systems, with a specialization in Applied Informatics. During his studies, he actively participated in solving practical simulation tasks, honing his practical skills. In 2012, he completed his tertiary education, defending his dissertation, which involved computer simulation for creating work schedules at one of Europe's largest inland container terminals. Since then, he has contributed to the development of various simulation software applications. Currently, he holds the position of a teacher at the University of Žilina. His research work focuses on the optimization and simulation of rescue station networks, and he has co-authored multiple publications in this field.
Ľudmila Jánošíková
Ľudmila Jánošíková (ORCID 0000-0003-3983-6713) is a Professor of Applied Informatics at the University of Žilina. She is a head of the Department of Mathematical Methods and Operations Research. Her research interests include strategic planning and optimization of public service systems. She focuses on the development of mathematical models and application of operations research methods. Professor Jánošíková has authored over 30 publications in archival journals and refereed proceedings.
Marek Kvet
Marek Kvet (ORCID 0000-0001-5851-1530) is an associated professor of Applied Informatics at the University of Žilina. His research and publication activities are aimed at location science, modelling, optimization and advanced exact and heuristic algorithms development. He is the author or a co-author of more than 70 scientific papers published in journals and conference proceedings indexed in Web of Science or SCOPUS. His teaching subjects cover the basics of programming and data structures.
Jozef Karaš
Jozef Karaš is a medical director at the AGEL Merea a.s. He has worked for many years as an anaesthesiologist in intensive care and emergency medicine, including pre-hospital emergency medicine. As a managing director he has managed a district general hospital and as a medical director and CEO managed the largest EMS company in Slovakia. He is the author or co-author of 4 books in the field of prehospital emergency medicine.
Gaston Ivanov
Gaston Ivanov is a healthcare analyst currently working as director of strategy for the largest health insurance fund in Slovakia. Previously, he worked on various public and private positions focusing on data analysis and strategy.
Ernest Caban
Ernest Caban is a CEO of AGEL Merea. He has worked in pre-hospital emergency health care for several years. He has served as the HEMS Center Chief Paramedic, EMS Paramedic, EMS Operations Manager, and Emergency Line Operator. He is co-author of the book “Proposal for changes in the concept of EMS and PTS”
References
- Aboueljinane, L., Sahin, E. and Jemai, Z. (2013) A review on simulation models applied to emergency medical service operations. Computers & Industrial Engineering 66, 734–750.
- Ahmadi-Javid, A., Seyedi, P. and Syam, S. S. (2017) A survey of healthcare facility location. Computers & Operations Research, 79, 223–263.
- Ambulance Quality Indicators Data 2022-23. NHS England. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulance-quality-indicators-data-2022-23/ (accessed 27 April 2023).
- Ambulance response times. Nuffield Trust. Available at https://www.nuffieldtrust.org.uk/resource/ambulance-response-times (accessed 27 April 2023).
- Andersson, H., Granberg, T.A., Christiansen, M., Aartun, E.S. and Leknes, H. (2020) Using optimization to provide decision support for strategic emergency medical service planning – Three case studies. International Journal of Medical Informatics, 133, 103975.
- Annual reports of Hato Hone St John. Available at https://www.stjohn.org.nz/news–info/our-performance/annual-reports/ (accessed 24 April 2023).
- Annual reports of the EMS Command and Control Centre of the Slovak Republic [in Slovak]. Available at https://155.sk/vyrocne-spravy/ (accessed 23 February 2023).
- Aringhieri, R., Bruni, M.E., Khodaparasti, S. and van Essen, J.T. (2017) Emergency medical services and beyond: Addressing new challenges through a wide literature review. Computers & Operations Research, 78, 349–368.
- Bélanger, V., Ruiz, A. and Soriano, P. (2019) Recent optimization models and trends in location, relocations, and dispatching of emergency vehicles. European Journal of Operational Research, 272, 1–23.
- Beraldi, P. and Bruni, M.E. (2009) A probabilistic model applied to emergency service vehicle location. European Journal of Operational Research, 196, 323–331.
- Bertsimas, D. and Ng, Y. (2019) Robust and stochastic formulations for ambulance deployment and dispatch. European Journal of Operational Research, 279, 557–571.
- Bürger, A., Wnent, J., Bohn, A., Jantzen, T., Brenner, S., Lefering, R., Seewald, S., Gräsner, J.T. and Fischer, M. (2018) The Effect of Ambulance Response Time on Survival Following Out-of-Hospital Cardiac Arrest. Deutsches Ärzteblatt International, 115, 541–548.
- Buzna, Ľ. and Czimmermann, P. (2021) On the Modelling of Emergency Ambulance Trips: The Case of the Žilina Region in Slovakia. Mathematics, 9, 2165.
- Church, R.L. and Murray, A. (2018) Location Covering Models: History, Applications and Advancements. Springer: Cham, Switzerland.
- Drezner, Z. and Hamacher, H.W. (2004) Facility Location: Applications and Theory. Springer: Heidelberg, Germany.
- Emergency medical services systems in the European Union. World Health Organization, 2008. Available at https://www.euro.who.int/data/assets/pdf_file/0016/114406/E92038.pdf. Accessed 28 May 2021.
- Felder, S. and Brinkmann, H. (2002) Spatial allocation of emergency medical services: minimising the death rate or providing equal access? Regional Science and Urban Economics, 32, 27–45.
- Fritze, R., Graser, A. and Sinnl, M. (2018) Combining spatial information and optimization for locating emergency medical service stations: A case study for Lower Austria. International Journal of Medical Informatics, 111, 24–36.
- Gondocs, Z., Olah, A., Marton-Simora, J., Nagy, G., Schaefer, J. and Betlehem, J. (2010) Prehospital emergency care in Hungary: What can we learn from the past? The Journal of Emergency Medicine, 39, 512–518.
- Hammami, S. and Jebali, A. (2021) Designing modular capacitated emergency medical service using information on ambulance trip. Operational Research, 21, 1723–1742.
- Henderson, S.G. and Mason, A.J. (2004) Ambulance service planning: simulation and data visualization, in M. Brandeau. F. Sainfort and W. Pierskalla (eds.), Operations research and health care: a handbook of methods and applications. International series in operations research & management science, Vol 70, Chap 4, pp 77–102, Kluwer, Dordrecht.
- Janáček, J. and Kvet, M. (2016) Sequential approximate approach to the p-median problem. Computers & Industrial Engineering, 94, 83–92.
- Jánošíková, Ľ., Jankovič, P., Kvet, M., Ivanov, G., Holod, J. and Berta, I. (2022) Reorganization of an emergency medical system in a mixed urban-rural area. International Journal of Environmental Research and Public Health, 19, 12369.
- Jánošíková, Ľ., Jankovič, P., Kvet, M. and Zajacová, F. (2021) Coverage versus response time objectives in ambulance location. International Journal of Health Geographics, 20, 32.
- Jánošíková, Ľ., Kvet, M., Jankovič, P. and Gábrišová, L. (2019) An optimization and simulation approach to emergency stations relocation. Central European Journal of Operations Research, 27, 737–758.
- Karaš, J., Weinciller, M., Havlíková, E., Caban, E., Humaj, M., Jánošíková, Ľ. et al. (2017) Proposal of changes in the concept of EMS and TMS (Návrh zmien v koncepcii ZZS a DZS) [in Slovak], SAPFO, Cassonic: Košice.
- Kitić Jaklič, T. and Kovač, J. (2015) The impact of demographic changes on the organization of emergency medical services: the case of Slovenia. Organizacija, 48, 247–259.
- LandScan database. Oak Ridge National Laboratory. Available at https://landscan.ornl.gov (accessed 15 October 2017).
- Lowthian, J.A., Cameron, P.A., Stoelwinder, J.U., Curtis, A., Currell, A., Cooke, M.W. et al. (2011) Increasing utilisation of emergency ambulances. Australian Health Review, 35, 63–69.
- McLay, L.A. (2009) A maximum expected covering location model with two types of servers. IIE Transactions, 41, 730–741.
- McLay, L.A. and Mayorga, M.E. (2013) A model for optimally dispatching ambulances to emergency calls with classification errors in patient priorities. IIE Transactions, 45, 1–24.
- Melo, M.T., Nickel, S. and Saldanha-da-Gama, F. (2009) Facility location and supply chain management – A review. European Journal of Operational Research, 196, 401–412.
- Moskatel, L.S. and Slusky, D.J.G. (2023) The impact of COVID-19 incidence on emergency medical services utilization. The Journal of Emergency Medicine, 65, e111–e118.
- Next Generation EU: Pandemic Recovery Plan (2021) [in Slovak]. Available at https://www.planobnovy.sk/site/assets/files/1019/kompletny-plan-obnovy.pdf (accessed 12 March 2021).
- Olave-Rojas, D. and Nickel, S. (2021) Modeling a pre-hospital emergency medical service using hybrid simulation and a machine learning approach. Simulation Modelling Practice and Theory, 109, 102302.
- OpenStreetMap database. Available at https://www.openstreetmap.org (accessed 16 April 2019).
- Ridler, S., Mason, A.J. and Raith, A. (2022) A simulation and optimisation package for emergency medical services. European Journal of Operational Research, 298, 1101–1113.
- Sagan, A., Kowalska-Bobko, I. and Mokrzycka, A. (2016) The 2015 emergency care reform in Poland: Some improvements, some unmet demands and some looming conflicts. Health Policy, 120, 1220–1225.
- Şahin, G. and Süral, H. (2007) A review of hierarchical facility location models. Computers & Operations Research, 34, 2310–2331.
- Strauss, C., Bildstein, G., Efe, J., Flacher, T., Hofmann, K., Huggler, M. et al. (2021) Optimizing emergency medical service structures using a rule-based discrete event simulation - a practitioner’s point of view. International Journal of Environmental Research and Public Health, 18, 2649.
- Toro-Díaz, H., Mayorga, M.E., McLay, L.A., Rajagopalan, H.K. and Saydam, C. Reducing disparities in large-scale emergency medical service systems. Journal of the Operational Research Society, 66, 1169-1181.
- van den Berg, P.L. and van Essen, J.T. (2019) Comparison of static ambulance location models. International Journal of Logistics Systems and Management, 32, 292–321.
- Zaffar, M.A., Rajagopalan, H.K., Saydam, C., Mayorga, M. and Sharer, E. (2016) Coverage, survivability or response time: A comparative study of performance statistics used in ambulance location models via simulation-optimization. Operations Research for Health Care, 11, 1–12.