ABSTRACT
The incidence of iron poisoning, once the most common cause of fatal pediatric unintentional ingestions, and the use of its antidote deferoxamine have declined. We describe a case of a 17-year-old girl who presented to a hospital following an intentional polysubstance ingestion, which included ferrous sulfate. She developed severe gastrointestinal symptoms including hematemesis, as well as anion gap metabolic acidosis, coagulopathy, and liver toxicity. She was treated with a prolonged course of greater than 24 h with deferoxamine due to a markedly elevated serum iron concentration of 2565 g/dL and worsening clinical status. Clinical features and management of complex iron poisoning are discussed. This case demonstrates the benefit of early poison control center and medial toxicology involvement in instances regarding the off-label usage of deferoxamine in the treatment of severe iron toxicity.
ABBREVIATIONS:
Introduction
The incidence of serious iron poisoning has drastically decreased over the last 30 years. Iron poisoning was once the most frequent cause of fatal pediatric unintentional ingestions [Citation1]. However, public health measures mandated by the U.S. Food and Drug Administration (FDA) following urging from the American Association of Poison Control Centers (AAPCC) have resulted in fewer ingestions and fewer fatalities. The AAPCC reported 5455 iron exposures in 2014. Of those, 2095 occurred in children under 6 years of age, and 547 were intentional ingestions. Only one fatality from iron toxicity was reported to the AAPCC in 2014 [Citation2]. Since 2005, the incidence of severe iron poisoning and subsequently the use of deferoxamine (DFO) have declined. This has resulted in provider inexperience with prescribing this chelator. We report a case of serious iron poisoning resulting from an intentional polysubstance ingestion that included ferrous sulfate. The patient's treatment included a complex regimen of DFO due to extremely elevated serum iron concentrations.
Case description
A 17-year-old girl presented to a local emergency department (ED) following intentional polysubstance ingestion. In the ED, she was lethargic but able to state that she ingested an unknown number of ferrous sulfate tablets. In addition, she also swallowed an unknown number of two over-the-counter products: Tylenol PM® (each containing 500 mg of acetaminophen and 25 mg of diphenhydramine) and Excedrin Extra Strength® (each containing 250 mg of acetaminophen, 250 mg aspirin, and 65 mg of caffeine). Her initial vital signs were as follows: temperature: 35.4 °C; heart rate: 153 beats per minute; respiratory rate: 20 breaths per minute; blood pressure: 154/103 mmHg; and oxygen saturation: 100% on 1 L/min of oxygen by nasal cannula. On examination, she was alert and oriented without focal neurologic deficits. She obeyed commands and was conversant though she was noted to have a flat affect. Her cardiovascular exam was notable for a peripheral capillary refill of greater than three seconds, and her abdominal exam was unremarkable. During her initial evaluation, she had an episode of hematemesis. An abdominal X-ray did not demonstrate tablets in her gastrointestinal system. Laboratory values revealed a metabolic acidosis on venous blood gas with pH, 7.16; pCO2, 43 mmHg; lactate, 10.4 mmol/L; and bicarbonate, 15 mmol/L. Other notable laboratory studies included the following: white blood cell count, 19.6 K/mm3; hemoglobin, 19 g/dL; platelets, 393 K/mm3; acetaminophen concentration, 74.6 µg/mL (2 h after reported ingestion); salicylate concentration, 7.3 mg/dL; and iron concentration, 2565 µg/dL. Urine drug screen performed by immunoassay was positive for cocaine metabolite. An electrocardiogram was significant for sinus tachycardia at a rate of 151 beats per minute and QTc of 535 ms. The patient received 50 mEq of intravenous sodium bicarbonate and then transferred to a Pediatric Intensive Care Unit (PICU) of a tertiary referral children's hospital.
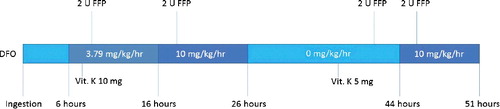
On arrival to the PICU, the patient's repeat laboratory values were significant for the following: iron concentration, 2793 µg/dL; acetaminophen concentration, 48 µg/mL (4 h post-ingestion) (); creatinine, 0.9 mg/dL; international normalized ratio (INR), 2.5 (). The patient was initially treated with a DFO infusion starting at 3.79 mg/kg/h for 10 h (). The on-call pharmacist did not feel comfortable exceeding the package insert's recommended maximum daily dose of 6 g, resulting in the initial rate choice. After consultation with the local poison control center, the rate was increased to 10 mg/kg/h. She received the DFO infusion at this rate for another 10 h. During this time, she continued to have episodes of frank hematemesis. She received 2 units of fresh frozen plasma (FFP) with a subsequent INR of 1.8 and decreased episodes of hematemesis. After 20.5 hours of DFO therapy, her infusion was held for 18 h, then resumed at 10 mg/kg/h for another 7 h. During this time, she did not develop any respiratory distress or hemodynamic instability.
Table 1. Serologic levels of ingested substances by time after ingestion.
Table 2. Serologic markers by time after ingestion.
Figure 1. Summary of DFO infusion rate and other therapies received by time after ingestion. DFO: deferoxamine; FFP: fresh frozen plasma; Vit K: phytonadione.
One day after the ingestion, the patient's iron concentration was 329 µg/dL. Approximately 36 h after the ingestion, the patient developed evidence of hepatotoxicity with aspartate aminotransferase (AST) rising from 199 to 1607 IU/L and alanine aminotransferase (ALT) rising from 96 to 2072 IU/L. Her conjugated bilirubin peaked at 1.9 mg/dL and unconjugated bilirubin peaked at 2.3 mg/dL. Given the patient's co-ingestion of acetaminophen, the providers initiated intravenous N-acetylcysteine therapy in case her reported time of ingestion was incorrect. She received a 21-hour course for presumed acetaminophen toxicity. During this time, she received an additional 2 units of FFP for persistently abnormal INR measurements. Three days post-ingestion, she began to show improvement in her ALT concentration, hyperbilirubinemia, and coagulopathy.
She transferred out of the PICU five days after admission and subsequently discharged from the hospital nine days after admission. Four weeks after the ingestion, the patient was evaluated in an outpatient gastroenterology clinic for emesis, poor oral intake and weight loss. A barium upper gastrointestinal fluoroscopy with small bowel follow-through showed no evidence of gastric outlet obstruction or stricture. However, due to continued feeding intolerance, six weeks after her ingestion, she underwent an esophagogastroduodenoscopy, which showed evidence of gastric outlet obstruction. She subsequently underwent two gastric dilations with the placement of a nasojejunal feeding tube. Six months after her ingestion, she has had appropriate weight gain despite intermittent symptoms of nausea.
Discussion
Once a leading cause of pediatric poisoning, the incidence of iron overdose has markedly diminished, largely due to a series of preventative measures, including warning labels and unit dose packaging, instituted by the U.S. FDA in the late 1990s [Citation3]. Only one death from iron overdose was reported in the 2014 National Poison Data System (NPDS) Annual Report [Citation2]. Despite the rarity of severe overdose, clinicians should remain aware of the indications for treatment of iron toxicity with deferoxamine and its associated risks.
Deferoxamine, an iron-specific chelator, can be used for acute or chronic iron overload. Following acute overdose, it is usually recommended for patients exhibiting evidence of serious poisoning (e.g. metabolic acidosis, shock) or with serum iron concentrations greater than 500 µg/dL [Citation4]. The standard recommended infusion rate is 15 mg/kg/h, though some authors advise starting at lower doses and titrating up to avoid hypotension, which may follow rapid infusion [Citation5,Citation6]. In this case, the patient received an initial rate of infusion at 3.79 mg/kg/h, which calculated by the hospital pharmacist based on the package insert that reported the maximum dose over a 24-hour period is 6 g. Current practice accepts that DFO often exceeds this 6 g limit. Deferoxamine is ideally administered early, while the majority of iron is accessible for chelation in the serum compartment, and for a short duration, to avoid side effects associated with prolonged infusion. Because of the extremely elevated serum iron concentration, the poison control center recommended increasing the rate of DFO infusion to at least 15 mg/kg/h with options to increase it up to 40 mg/kg/h if the patient could tolerate the infusion. Perhaps, the most concerning of deferoxamine's potential side effects is development of acute respiratory distress syndrome (ARDS). Significant pulmonary toxicity has been reported following intravenous infusions for greater than 24 h [Citation7,Citation8]. Proposed mechanisms for pulmonary injury include free radical formation and intracellular catalase depletion [Citation9]. Given the patient's markedly elevated serum iron concentration, concern existed regarding the possibility of a lengthy treatment course. In an attempt to avoid pulmonary complications, we recommended at least a 12-hour deferoxamine “holiday” once the patient's initial treatment approached 24 h. We found only one prior report of an intermittent dosing approach following acute iron overdose [Citation10]. The patient in that case developed ARDS on the second hospital day, but was treated with a higher infusion rate (25 mg/kg/h) due to his poor presenting condition and exceedingly high serum iron concentration (16,706 μg/dL). Fortunately, our patient's clinical status markedly improved following approximately 27.5 hours of therapy, and she showed no evidence of pulmonary toxicity during her hospitalization.
The co-ingestions of acetaminophen-containing products confounded the clinical presentation of this patient. She developed signs of hepatotoxicity between 24 and 48 h post-ingestion with rising transaminases and development of coagulopathy. Liver toxicity is a relatively late clinical feature of severe iron poisoning, typically occurring between 2 and 3 days following ingestion. Iron causes local oxidative damage upon entering the liver [Citation4,Citation5]. While it is possible that the patient developed acetaminophen-induced liver injury, perhaps due to an inaccurate history of time of ingestion, it is more likely that the patient's hepatotoxicity was a result of iron toxicity.
Conclusion
Clinically significant iron poisoning occurs less frequently following preventative measures instituted by the FDA in prior decades. This decrease has resulted in provider inexperience with evaluation and management of cases, particularly in the prescribing of DFO. This case of severe iron toxicity highlights successful management in collaboration with medical toxicologists who recommended an off-label, prolonged and intermittent DFO infusion. Early consultation of a medical toxicologist or poison control center can help providers navigate complicated cases of iron toxicity, especially in the context of decreasing frequency of such cases.
Disclosure statement
The authors have no potential conflicts of interest.
References
- Litovitz T, Manoguerra A. “Comparison of pediatric poisoning hazards: an analysis of 3.8 million exposure incidents. A report from the American Association of Poison Control Centers.” Pediatrics. 89(6 Pt 1):999–1006.
- Mowry JB, Spyker DA, Brooks DE, et al. 2014 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd annual report. Clin Toxicol (Phila). 2015;53(10):962–1147.
- Tenenbein M. Unit dose packaging of iron supplements and reduction of iron poisoning in young children. Arch Pediatr Adolesc Med. 2005;159:593–595.
- Perrone J. Iron. In: Goldfrank LR, editor. Goldfrank's toxicologic emergencies. 10th ed. New York (NY): McGraw-Hill.
- Howland MA. Antidotes in depth: deferoxamine. In: Goldfrank LR, editor. Goldfrank's toxicologic emergencies. 10th ed. New York (NY): McGraw-Hill.
- Wetslin W. Deferoxamine in the treatment of acute iron poisoning. Clinical experiences with 172 children. Clin Pediatr. 1966;5:531–535.
- Ioannides AS, Panisello JM. Acute respiratory distress syndrome in children with acute iron poisoning. The role of intravenous desferrioxamine. Eur J Pediatr. 2000;159:158–159.
- Adamson I, Sienko A, Tenenbein M. Pulmonary toxicity of deferoxamine in iron-poisoned mice. Toxicol Appl Pharmacol. 1993;120:13–19.
- Tenenbein M, Kowalski S, Sienko A, et al. Pulmonary toxic effects of continuous administration in acute iron poisoning. Lancet. 1992;339:699–701.
- Cheney K, Gumbiner C, Benson B, et al. Survival after a severe iron poisoning treated with intermittent infusions of deferoxamine. J Toxicol Clin Toxicol. 1995;33:61–66.
