Abstract
Emergency Department (ED)-based initiation of buprenorphine-naloxone is increasingly recognized as standard care in treating patients with opioid withdrawal and opioid use disorders. We provide an ED buprenorphine-naloxone order set to facilitate home and in-ED induction. This clinical tool was developed by an interdisciplinary group of experts at our institution. We were unable to identify any similar electronic decision-support tools for reference when we created our own. Our goal in sharing this order set is to accelerate the development of similar tools in other healthcare settings.
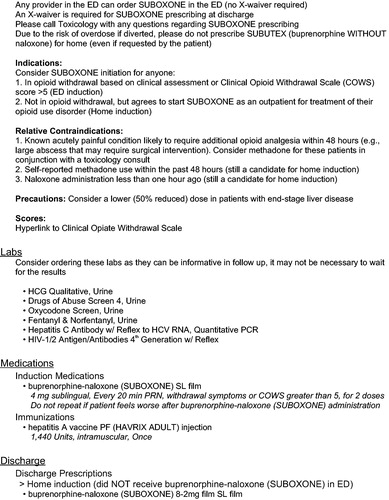
Emergency Department (ED)-based initiation of buprenorphine-naloxone is increasingly recognized as standard care in treating patients with opioid withdrawal and opioid use disorders [Citation1]. During implementation of an ED-initiated buprenorphine-naloxone program in our medical center, we developed an order set to facilitate either: 1) ED induction for patients in opioid withdrawal, or 2) home induction for patients who desire buprenorphine-naloxone treatment yet are not in withdrawal at the time of ED discharge. Experts from medical toxicology, emergency medicine, addiction medicine, addiction psychiatry, pharmacy, and informatics provided input on the content and design of this order set for our electronic health record (see ).
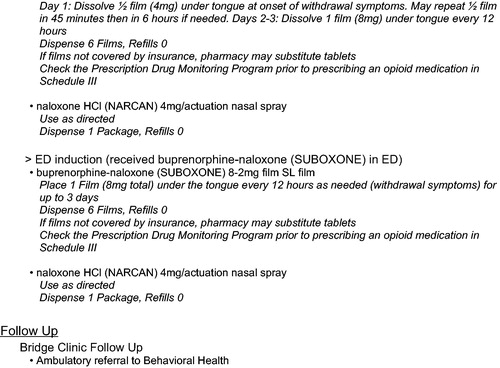
Figure 1. ED buprenorphine-naloxone (SUBOXONE) order set.
The initial text of the order set provides specific guidance regarding buprenorphine-naloxone prescribing in the United States. Any prescriber may order this medication for patients currently in the ED [Citation2, Citation3]; however, a DATA 2000 practitioner waiver (commonly called an “X-waiver”) is required for a clinician to write a prescription for buprenorphine-naloxone to be filled after discharge [Citation4]. Based on emerging evidence (and for simplicity), we selected the buprenorphine-naloxone combination product rather than buprenorphine monotherapy for all emergency department patients, regardless of pregnancy status [Citation5]. While buprenorphine monotherapy has traditionally been used for pregnant patients, several authors and programs have noted the safety of buprenorphine-naloxone in pregnancy; uniform use of buprenorphine-naloxone circumvents concerns regarding diversion of the monoproduct, coercion of pregnant women to obtain the monoproduct, and difficulties transitioning women back to buprenorphine-naloxone in the postpartum period [Citation5–7].
Noted exclusions for buprenorphine-naloxone administration in this order set include anticipated painful conditions (e.g. need for surgical procedure), self-reported methadone use within 48 h (due to risk of precipitated withdrawal), or naloxone administration less than one-hour prior. Alternative considerations for managing painful conditions include the use of full opioid agonists (other than methadone), alone or in combination with buprenorphine-naloxone at typical or higher doses.
We provide a link to the Clinical Opiate Withdrawal Scale (COWS) for additional guidance, with a score of 5 or greater recommended as the threshold for treatment [Citation8]. However, we specifically do not require a COWS score to facilitate buprenorphine-naloxone administration in patients with clinically apparent opioid withdrawal. In our setting, precipitated withdrawal would typically prompt contact with the toxicology service. In the event of precipitated withdrawal, recommendations could include medications for symptom relief (e.g. ondansetron, loperamide), or increased buprenorphine-naloxone dosing.
We utilize an initial starting dose of 4 mg of the buprenorphine-naloxone film, with up to two subsequent 4 mg doses every 20 min as needed for continued withdrawal symptoms. We considered alternative initiation dosing, including a “test dose” of 2 mg as well as a starting dose of 8 mg; however, we ultimately selected the specified regimen for safety and simplicity. The order set includes a recommendation for 50% dose reduction for patients with end-stage liver disease [Citation4]. We do not require any analytical testing prior to initiation of buprenorphine/naloxone; suggested laboratory studies are included primarily to facilitate follow-up. Because of a recent hepatitis A outbreak among local injection drug users, we include an order for hepatitis A vaccination. While hepatitis A vaccines are usually administered as a series, “a single dose of vaccine rapidly provides 95% seroprotection from infection; this protection lasts at least 11 years and has been demonstrated to curb outbreaks.” [Citation9]
Patients who receive their first dose of buprenorphine-naloxone in the ED (“ED induction”) are discharged with a prescription for buprenorphine-naloxone 8-2mg twice daily for three days. Patients who undergo home induction receive a prescription that mirrors the National Institute on Drug Abuse (NIDA) home induction instructions [Citation10]. Our prescriptions allow for pharmacy substitution of tablets for films to accommodate insurance formularies without the need for additional provider contact. After either ED or home induction, naloxone (4 mg actuation spray x 2 units) is co-prescribed.
Undoubtedly, other centers have created similar electronic decision-support tools to facilitate ED-based buprenorphine-naloxone prescribing, and we anticipate differences in the details. However, we were unable to identify any similar order sets for reference when we wrote our own. Our goal in sharing this version is to accelerate the development of similar tools in other healthcare settings.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Love JS, Perrone J, Nelson LS. Should buprenorphine be administered to patients with opioid withdrawal in the emergency department?. Ann Emerg Med. 2018;72(1):26–28.
- Substance Abuse and Mental Health Services Administration. Special Circumstances for Providing Buprenorphine 2019 [updated March 2019. Available from: https://www.samhsa.gov/medication-assisted-treatment/legislation-regulations-guidelines/special.
- American College of Emergency Physicians. BUPE: Buprenorphine use in the Emergency Department Tool [cited 2019 November 21]. Available from: https://www.acep.org/patient-care/bupe/.
- SUBOXONE® (buprenorphine and naloxone) sublingual film, for sublingual or buccal use CIII 2018 August 30, 2019. Available from: https://www.suboxone.com/pdfs/prescribing-information.pdf.
- Dooley J, Gerber-Finn L, Antone I, et al. Buprenorphine-naloxone use in pregnancy for treatment of opioid dependence: Retrospective cohort study of 30 patients [Utilisation de la buprénorphine-naloxone durant la grossesse pour traiter la dépendance aux opiacés]. Can Fam Physician. 2016;62:e194–e200.
- Debelak K, Morrone WR, O'Grady KE, et al. Buprenorphine + naloxone in the treatment of opioid dependence during pregnancy-initial patient care and outcome data. Am J Addict. 2013;22(3):252–254.
- Center for Addiction Recovery in Pregnancy and Parenting. Use of Buprenorphine-Naloxone (Suboxone) in Pregnancy Available from: https://med.dartmouth-hitchcock.org/documents/Use-of-Buprenorphine-Naloxone-in-Pregnancy.pdf.
- Wesson DR, Ling W. The Clinical Opiate Withdrawal Scale (COWS). J Psychoact Drugs. 2003;35(2):253–259.
- Commonwealth of Massachusetts, Executive Office of Health and Human Services. Hepatitis A virus infection in persons experiencing homelessness and substance use disorder. Boston, Ma: Department of Public Health, Bureau of Infectious Disease and Laboratory Sciences, editor. 2018.
- National Institute on Drug Abuse. A Guide for Patients Beginning Buprenorphine Treatment at Home 2018. Available from: https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/home_buprenorphine_initiation.pdf.