Abstract
Eye exposure to hexavalent chromium (Cr(VI)) acid can cause blindness. A 42-year-old man working in a plating operation presented to the emergency department following a workplace incident. He had unintentionally fallen into a tank containing a mixture of 25% Cr(VI) and sulfuric acid (2.0 g/L) at a temperature of approximately 40 °C. The tank dimensions tank were 8 (depth) × 4 (width) × 3 (length) meters. A colleague rescued him from the tank, and he underwent a full body wash at the worksite. Emergency services adequately flushed both eyes with a 0.9% saline solution. He had significant corneal injury; however, no other significant injuries occurred. Upon presentation at the emergency department, the patient underwent a whole-body shower, and both eyes were flushed with 0.9% saline solution. As a treatment for acute chromium poisoning, he received dimercaprol and ascorbic acid. Additionally, he received eye drops for chemical corneal injury. The patient later underwent bilateral corneal transplants for chemical corneal injury but remained nearly blind. We describe a case of severe chemical corneal injury with limbal stem cell deficiency, leading to blindness due to Cr (VI) acid exposure.
Introduction
Elemental chromium is a stable, extremely rust-resistant, and harmless metal. However, hexavalent chromium (Cr(VI)) is highly toxic and is rapidly absorbed both transdermally and orally. In cases involving Cr(VI) poisoning, symptoms may become severe even with a low concentration of exposure. In accordance with the CARE guideline (https://www.care-statement.org), we present a case of a vision-threatening corneal injury leading to blindness despite corneal transplant after acute exposure to a Cr(VI) acid mixture.
Case report
A 42-year-old man working in a plating operation accidentally fell into a tank containing a mixture of Cr(VI) 25% concentration and sulfuric acid (2.0 g/L at approximately 40 °C (pH unknown). The dimensions of the tank were 8 (depth) × 4 (width) × 3 (length) meters. The worker’s entire body, including head, was submerged for several seconds, and his trunk and extremities remained within the acidic mixture for approximately five minutes. He did not drink or aspirate the solution. After a colleague rescued him, workplace decontamination procedures were initialized, including a full body wash using tap water. Both eyes were adequately flushed with 0.9% saline solution by emergency services. The patient was transported via emergency services to our hospital’s emergency department. Upon arrival, his initial axillary temperature was 36.5 °C, heart rate was 85 beats per minute, respiratory rate was 9 breaths per minute, and blood pressure was 200/121 mmHg. His Glasgow Coma Scale score was 15/15. Bilateral corneal opacity and edema were present, and the visual acuity was significantly impaired (). Visual acuity was 20/500 (uncorrectable) in both eyes. According to the Roper–Hall classification [Citation1], we diagnosed his corneal injuries as Grade IV. He had no significant traumatic injuries. Blood tests revealed mild liver dysfunction but no other abnormalities (). Whole-body computed tomography revealed normal findings.
Figure 1. Ocular findings. Patient images of right eye. The left eye showed similar findings. (A) Anterior segment image upon hospital arrival. Severe epithelial defects observed in all corneas, including the limbs, bulbar conjunctiva, and corneal stromal edema. (B) Anterior segment image with fluorescein staining 13 days after chromium exposure. Extensive corneal epithelial defects persisted, suggesting the possibility of corneal limbal stem cell deficiency. (C) Anterior segment optical coherence tomography image 13 days after chromium exposure showing corneal stromal edema.
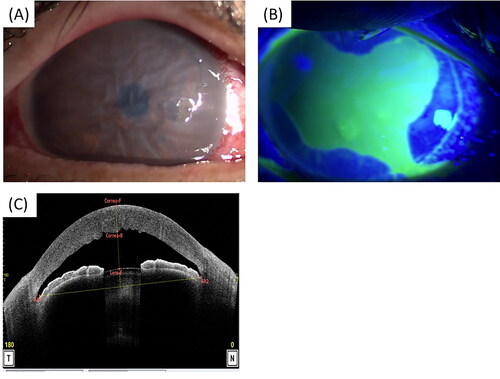
Table 1. Laboratory examination results on arrival at our hospital.
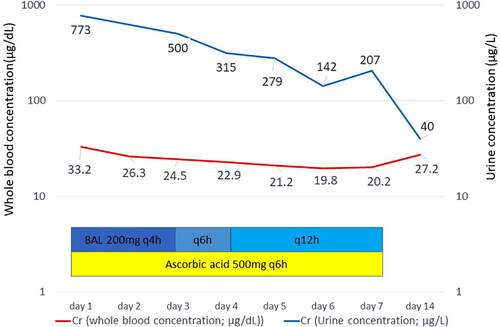
To treat acute hexavalent chromium poisoning, he received dimercaprol [Citation2], and ascorbic acid [Citation3] planned for 10 days ().
Although expected, renal and hepatic injury due to acute chromium poisoning did not occur. He received levofloxacin, betamethasone, hyaluronic acid eye drops, and ofloxacin eye ointment to treat chemical injury to the cornea. Seven days after admission, we discontinued dimercaprol and ascorbic acid because the possibility of organ injury was quite low. There was no relapse of organ or skin injuries.
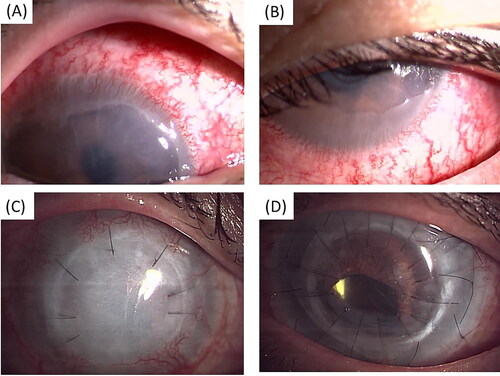
Thirteen days after admission, he continued to have mild corneal opacity in both eyes by slit lamp photography, prolonged extensive corneal epithelial defect by fluorescein staining (), and severe corneal stromal edema on anterior segment optical coherence tomography (). Twenty-six days after admission, slit lamp photography revealed corneal neovascularization and invasion of conjunctival epithelial cells into the cornea in both eyes by (). The patient was discharged on the 28th day of hospitalization.
Figure 3. Ocular findings. (A, C) Patient’s right eye, (B, D) patient’s left eye. (A, B) Anterior segment image at 26 days after the chromium exposure shows corneal neovascularization and conjunctiva invasion into cornea. (C) Postoperative anterior segment image of deep anterior lamellar keratoplasty and corneal limbal transplantation. (D) Postoperative anterior segment image of full-thickness penetrating keratoplasty and corneal limbal transplantation.
We measured the concentration of chromium in the blood and urine daily from the time of injury to the seventh day after admission. shows the progression of chromium concentration in blood and urine.
Despite continued treatment for chemical corneal injury, his vision failed to improve. Therefore, four months after the injury, the patient underwent corneal limbal transplantation in the right eye and deep anterior lamellar keratoplasty using the same donor cornea, considering the possibility of high rejection in corneal limbal transplantation (). However, due to endothelial chemical injury and possibly due to the high permeability of hexavalent chromium, corneal stromal edema persisted, indicating a need for endothelial transplantation. Fifty months after the injury, the patient underwent full-thickness penetrating keratoplasty and corneal limbal transplantation in the left eye (). Despite transplantation, corneal opacity continued, and the patient’s eyesight deteriorated further to the point where his visual acuity was severely impaired, especially in the right eye. Visual acuity was measured by counting fingers from 10 cm in the right eye and 20 cm in the left eye.
Discussion
Acid injuries typically cause more limited injury of the ocular surface than alkali injuries. Ocular exposure to Cr (VI) can cause conjunctivitis, keratitis, corneal injury (opacification, scarring, and vitiligo), and even blindness [Citation4, Citation5].
Conclusions
Exposure to Cr(VI) and sulfuric acid exposure a case of severe chemical corneal injury that led to corneal limbal stem cell deficiency and permanent vision loss.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc U K. 1965;85:631–653.
- Bradberry SM, Vale JA. Therapeutic review: is ascorbic acid of value in chromium poisoning and chromium dermatitis? J Toxicol Clin Toxicol. 1999;37(2):195–200.
- Blanusa M, Varnai VM, Piasek M, et al. Chelators as antidotes of metal toxicity: therapeutic and experimental aspects. Curr Med Chem. 2005;12(23):2771–2794.
- Haddad LM, Shannon MW, Winchester JF. Clinical management of poisoning and drug overdose. 3rd ed. Philadelphia (US): Saunders; 1998; p. 794–795.
- Shoichiro Y, Michiharu H, Futoshi Y, et al. Kyusei chudoku jyoho file. 3rd ed. Tokyo (Japan): Hirokawa; 1996; p. 383.