Abstract
Introduction
Coronavirus disease 2019 (COVID-19), originated in late December 2019, in Wuhan, China. The World Health Organization declared a pandemic on 11 March 2020, with the rapidly rising number of cases and fatalities over hours and days all around the world.
Aim
To assess the number and the trend of the poisoning consultations to the Poison Unit in the Mansoura Emergency Hospital during the era of the COVID-19 pandemic in 2020.
Methods
We collected data from the database of the Poison Unit and the Statistics Department of the Mansoura Emergency Hospital of the cases and the calls coming to the Poison Unit in the period from January 2018 through December 2020. We compared 2020 exposures to 2018–2019 exposures by using simple logistic models to provide effect size with odds ratios.
Results
The Mansoura Emergency Hospital Poison Unit treated 1752 cases in 2020, compared to 2210 cases in 2018 and 2539 cases in 2019. The Poison Unit treated 26% fewer patients in 2020 than either 2018 or 2019), while calls increased nearly 50% in 2020 than in 2018 and 2019. Calls came more frequently from the general public than health professionals and more frequently in afternoon and evening than in the morning. There was a significant increase in the cases of pharmaceuticals ingestion, food poisoning, corrosives and households exposures in 2020 compared to 2018 and 2019 (p-value 0.004, 0.024, and 0.0002, respectively; odds ratio 1.224, 1.691, and 1.692, respectively).
Conclusion
The COVID-19 pandemic changed the pattern of poisoning exposure and use of the Poison Control Center services.
Introduction
Coronavirus disease 2019 (COVID-19) originated in late December 2019, in Wuhan, China. Since then, it has affected many people and rapidly spread to almost all countries of the world to be announced by the WHO as a pandemic on 11 March 2020 [Citation1].
The Egyptian government ordered a lockdown on 15 March 2020, to limit the fast spread of the evolving pandemic. This included closing schools, closing theatres, restricting travel, mandating quarantines for incoming travelers, closing all shops except pharmacies, and food stuffs shops. Measures included mandatory masking, distancing, and placement of barriers at cashier stands, limiting restaurants to 50% occupancy after partial opening from lockdown.
The situation created many challenges in the health sector including the Poison Management Centers. Six principles were described by Motawei, for the management of poisoning cases during the COVID-19 era, which are susceptibility, transmission, fatality rates, precautions, notification, and treatment [Citation2].
Aim
To assess the number and the trend of in-person poisoning consultations and calls to the Poison Unit in the Mansoura Emergency Hospital during the three-years period (2018- 2020); including the first year of the COVID-19 pandemic.
Methods
Data source
We used the database of the Poison Unit and the Statistics Department of the Mansoura Emergency Hospital. The calls coming to the Poison Call Center were commented upon separately. The Poison Unit provides 24 h/7 days call line for toxic exposures from the public and healthcare providers.
Case inclusion/exclusion
We included poisoning cases treated at the Poison Unit in Mansoura Emergency Hospital or calling the Poison Unit for advice. We excluded calls and visits with no confirmed toxic exposure.
Statistics
We compared the frequencies of poisoned patients’ visits and calls in 2020 to the previous two-year interval (2018 through 2019). We expressed results as number (percentage) for discrete variables (and change in proportion). We considered these 2018 and 2019 together as a reference. We used Statistical Analysis System software (v9.4, SAS Inc., Cary, NC) to calculate odds ratios (OR) and 95% confidence intervals (95% CI). In the case of multiple reference categories, we used the category with the last to the expected difference.
Results
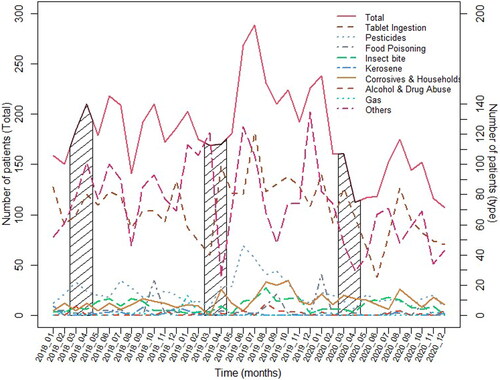
shows the number of cases attending to the Poison Unit in the Mansoura Emergency Hospital during 2020 in comparison to the mean of the two years before (2018 and 2019).
Table 1. Poisoning cases attending Mansoura Emergency Hospital Poison Unit in 2020 versus the mean of 2018 and 2019.
It shows that the overall number of types of poisonings in 2020 decreased by 26.2% compared with the average occurrence in 2018 and 2019. Among them, pesticides poisoning, kerosene poisoning, and gas poisoning decreased by more than 40%. The decline rates were 43.8%, 71.4%, and 58.3%, respectively.
On the contrary, food poisoning and corrosives & household poisoning increased by 12.3% and 12.4%, respectively, compared with the average occurrence in 2018 and 2019. The odds ratio, food poisoning, and corrosives & households poisoning are higher than 1 relative to other poisonings. shows the comparison of the poisoning cases attendance in the March–April period of the two years with the year 2020 (The period of beginning of the lockdown in Egypt).
Table 2. Poisoning Cases attending Mansoura Emergency Hospital Poison Unit in 2020 versus mean of 2018–2019 (March and April).
It shows that the overall number of types of poisonings in 2020 decreased by 26.2% compared with the average occurrence in March–April of 2018 and 2019. Among them, pesticides poisoning and others poisoning decreased by more than 50%. The decline rates were 58.1% and 52.8%, respectively.
On the contrary, food poisoning and corrosives and households poisoning increased by 60% and 71.4%, respectively, compared with the average occurrence in March–April of 2018 and 2019. The odds ratios, Tablets ingestion poisoning, corrosives and households poisoning are statistically significantly greater than one relative to other poisonings, 2.21 and 3.64, respectively.
represents the pattern of patients treated in the Poison Unit for the three-year period from 1 January 2018 through 31 December 2020.
Discussion
The effect of the COVID-19 pandemic that struck the world by late December 2019 was studied on the pattern and the trend of poisoning exposures. Mehrpour and Sadeghi reported that 700 people died in Iran from misusing denatured alcohols containing methanol, as disinfectants against COVID-19 infection [Citation3]. Chang et al. studied data from the National Poison Data System in the US for the three-month period of January through March 2020 in comparison to the same three-month interval in 2018 and 2019. They found sharp increases in exposures to cleaning agents and disinfectants during March 2020 compared to previous months and compared to the same month in previous years [Citation4]. Similar trends occurred in France and Pakistan during the same time interval [Citation5,Citation6].
The number of poisoning patients attending the Mansoura Emergency Hospital Poison Unit decreased by about (3.26%) in 2020 to the mean of the previous two years (p = 0.056), while calls to the hotline increased by approximately 50%.
Three types of poisoning (Tablets “pharmaceuticals” Ingestion, Food Poisoning, and Corrosives and Households) showed a change in the pattern in 2020 than in 2018 and 2019 (odds ratios show significantly different from 2020 than the mean of 2018 and 2019. The number of patients with tablet ingestion significantly decreased in 2020 relative to 2018 and 2019. The number of patients with food poisoning and corrosives and households showed a significant increase and a highly significant increase in 2020, relative to 2018 and 2019 ().
Unlike in most countries, the rate of alcohol consumption and poisoning decreased in our population in 2020 compared than before (2019 and 2018). This is mostly because the decrease in availability by the lockdown, and by the punitive legislations against people who consume alcohol and drive a vehicle.
An overall decrease in the number of cases attending to the Poison Unit by 3.26% and a large increase in calls by about 50% mostly from general public than health professionals, was observed in our study. This is different from what was reported from the French PCC that observed an overall increase in exposures by 5.6% and a small increase in calls [Citation7]. This denotes the people’s attitude in our locality in the early COVID-19 period of fear from hospitals to avoid catching an infection.
These are similar to Le Roux et al. and McCulley et al. [Citation7,Citation8]. Le Roux et al. in France analyzed poisoning exposures during the COVID-19 outbreak and lockdown. They found an increase in disinfectants and alcohol-based hand sanitizers exposures and a decrease in recreational, addictive, and pharmaceuticals exposures [Citation7]. McCulley et al. reported an increase in alcohol-based hand sanitizer exposures and their effects on young children in the U.S. during the early COVID-19 pandemic [Citation8].
The lockdown issued in Egypt on 15 March 2020, was directly reflected on the population behavior with the use of healthcare and the Poison Control Center services. Schools and universities were closed, industrial activities were greatly reduced, and work was mostly converted to teleworking for non-industrial activities. Only stores for food and pharmaceuticals were allowed to remain open. Our results go with these changes, patients’ attendance to hospital decreased and calls increased significantly than the same period of the previous two years; 2018 and 2019. This is concomitant with the people’s fear to catch the COVID-19 infection and to go with the health regulations of social distancing.
This is evident here in this study, by the significant decrease in total numbers of patients attending the Poison Unit in (March–April) in 2020 as compared by the previous two years (p = 0.001) ( and ).
This goes with what is reported by Hartnett and colleagues who studied the effects of the pandemic and lockdown on ED visits in the US in 2020 and found decreases in ED visits by 42% in the early pandemic period (March 29–April 25, 2020) compared to the same period a year earlier. The visits were mostly for serious conditions like myocardial infarction not for mild or moderate conditions [Citation9]. Also, Thornton reported a decrease by 25% in week in ED visits after lockdown in the United Kingdom [Citation10].
The number of calls to our Poison Unit has changed in pattern and timing, this may be due to the changed sleep-wake cycle with the lockdown and the remote working that made blurred boundaries between the work and the family life. Chary et al. saw similar changes in poison center calls in greater Boston area in the US [Citation11].
Alcohol-based hand sanitizers (ABHS) normally contain ethanol or isopropanol as the disinfecting alcohol. The shortage of ABHS at the beginning of the COVID-19 pandemic led to the production of home-made alcohol-based hand sanitizers that may use cheap alcohols “Methanol” and are usually stored in unlabeled containers that had led to increasing the risk of alcohol-based hand sanitizers poisoning and accidental ingestion. The same observation was reported by Yip et al. in 2020 [Citation12].
Despite the COVID-19 pandemic and the home isolation were suggested to increase anxiety, depression, distress, sleep disturbance, and suicidal ideation, our results showed a decrease in Pharmaceuticals overdose poisoning. This mirrors similar trends seen in France, the US, the UK, Germany, and China [Citation7,Citation13–16].
One limitation of our study is that the data of the calls are approximate. Further follow up for the rate in 2021 and 2022, with recording of the sociodemographic data, the circumstances of exposure and death tolls should be done. Also, categorizing pharmaceuticals ingestion in a more detailed manner in hospital records (e.g. antidepressants, antihistaminic, β-blockers, hypoglycemics … etc.).
Conclusion
The COVID-19 pandemic period saw a change in the number and pattern of poisoning cases and the way of seeking the medical care. The Poison Unit cared for 26% fewer patients in 2020 than the two years before the pandemic while receiving 50% more calls mostly from the general public than from health professionals.
Exposures to corrosives/household products increased while pharmaceutical ingestions declined in 2020 compared to 2018–2019.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- World Health Organization. [cited 2022 Mar 12]. Available from: who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- Motawei SM. Coronavirus disease 2019 (COVID-19): Emerging and Future Challenges in Toxicology Practice. JVAT. 2020;1(2):3–5.
- Mehrpour O, Sadeghi M. Toll of acute methanol poisoning for preventing COVID-19. Arch Toxicol. 2020;94(6):2259–2260.
- Chang A, Schnall AH, Law R, et al. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19 - National Poison Data System, United States, January 1, 2020-March 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(16):496–498.
- Le Roux G, Sinno-Tellier S, Descatha A. COVID-19: home poisoning throughout the containment period. Lancet Public Health. 2020;5(6):e314.
- Mahmood A, Eqan M, Pervez S, et al . COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Sci Total Environ. 2020;742:140561.
- Le Roux G, Sinno-Tellier S, Puskarczyk E, French PCC Research Group, et al. Poisoning during the COVID-19 outbreak and lockdown: retrospective analysis of exposures reported to French poison control centres. Clin Toxicol (Phila). 2021;59(9):832–839.
- McCulley L, Cheng C, Mentari E, et al. Alcohol-based hand sanitizer exposures and effects on young children in the U.S. during the COVID-19 pandemic. Clin Toxicol (Phila). 2021;59(4):355–356.
- Hartnett KP, Kite-Powell A, DeVies J, National Syndromic Surveillance Program Community of Practice, et al. Impact of the COVID-19 pandemic on emergency department visits – United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704.
- Thornton J. COVID-19: a&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401.
- Chary MA, Overbeek DL, Papadimoulis A, et al. Geospatial correlation between COVID-19 health misinformation and poisoning with household cleaners in the Greater Boston Area. Clin Toxicol (Phila). 2021;59(4):320–325. Apr
- Yip L, Bixler D, Brooks DE, et al. Serious adverse health events, including death, associated with ingesting alcohol-based hand sanitizers containing methanol - Arizona and New Mexico, May-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1070–1073.
- Fisher KA, Tenforde MW, Feldstein LR, CDC COVID-19 Response Team, et al. Community and close contact exposures associated with COVID-19 among symptomatic adults ≥18 years in 11 outpatient health care facilities - United States, July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1258–1264. Sep 11 Erratum in: MMWR Morb Mortal Wkly Rep. 2020 Sep 25;69(38):1380.
- Cook MA, Brooke N. Event-based surveillance of poisonings and potentially hazardous exposures over 12 months of the COVID-19 pandemic. IJERPH. 2021;18(21):11133.
- Skalny AV, Lima TR, Ke T, et al. Toxic metal exposure as a possible risk factor for COVID-19 and other respiratory infectious diseases. Food Chem Toxicol. 2020;146:111809.
- Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. JCM. 2020;9(2):575.